Exudative Retinal Detachment
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Exudative (or serous) retinal detachment (ERD) occurs when fluid accumulates in the subretinal space between the sensory retina and the retinal pigmented epithelium (RPE) resulting in retinal detachment. Causes for fluid accumulation include inflammatory, infectious, and neoplastic diseases of the choroid or retina.[1][2]
Causes
Inflammatory
- Vogt-Koyanagi-Harada (VKH) syndrome
- Sympathetic ophthalmia (SO)
- Idiopathic Orbital Inflammatory Syndrome (IOIS)
- Posterior Scleritis (PS)
- Serpiginous Choroiditis
- Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE)
- Unilateral Acute Idiopathic Maculopathy (UAIM)
- Behçet Disease (BD)
- Relapsing Polychondritis (RPC)
- Intermediate Uveitis
- Sarcoid Uveitis
- Acute Retinal Necrosis
Infectious
- Tuberculosis (TB)
- Toxoplasmosis
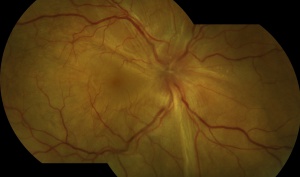
 Acute Toxoplasmosis Neuroretinitis By Hamid Ahmadieh, MD. Color fundus photograph of the left eye of a 26-year-old man with clinical picture of acute neuroretinitis and serologic evidence of Toxoplasma gondii infection. Disc swelling, necrotizing retinitis with overlying vitreous inflammation, retinal vasculitis, and localized exudative retinal detachment are visible.
Acute Toxoplasmosis Neuroretinitis By Hamid Ahmadieh, MD. Color fundus photograph of the left eye of a 26-year-old man with clinical picture of acute neuroretinitis and serologic evidence of Toxoplasma gondii infection. Disc swelling, necrotizing retinitis with overlying vitreous inflammation, retinal vasculitis, and localized exudative retinal detachment are visible. - Syphilis
- Dengue fever (DF)
- Lyme disease
- Cytomegalovirus (CMV)
- Nematodes (Cysticercosis and Toxocariasis)
- Fungi (Candidiasis, Aspergillosis, Histoplasmosis, and Cryptococcosis)
Neoplastic
- Choroidal Melanoma
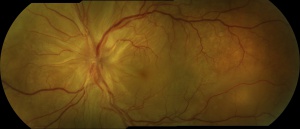
 Choroidal Melanoma By Karen Panzegrau. Ultra-wide field Optos image of a 27-year-old male patient who presented with loss of vision for about 6-8 weeks. Previous choroidal nevus seen. Recommended annual monitoring. No exam for since 10/2014. Brachytherapy vs enucleation was discussed. Brachytherapy was decided as treatment. Full metastatic work up is being performed.
Choroidal Melanoma By Karen Panzegrau. Ultra-wide field Optos image of a 27-year-old male patient who presented with loss of vision for about 6-8 weeks. Previous choroidal nevus seen. Recommended annual monitoring. No exam for since 10/2014. Brachytherapy vs enucleation was discussed. Brachytherapy was decided as treatment. Full metastatic work up is being performed. - Choroidal Osteoma
- Choroidal Hemangioma
- Choroidal Lymphoma
- Choroidal Metastasis
- Hematologic Malignancies
- Retinal Vasoproliferative Tumor (VPT)
- Retinal Astrocytic Hamartoma (Tuberous Sclerosis)
- Vitreoretinal Lymphoma
Other
- Familial Exudative Vitreoretinopathy (FEVR)
- Retinal Vein Occlusion (RVO)
- Coats' Disease (Retinal Telangiectasis)
- Diabetic Macular Edema (DME)
- Pre-eclampsia/Eclampsia/ HELLP
- Hemolytic Uremic Syndrome (HUS) and Thrombotic Thrombocytopenic Purpura (TTP)
- Idiopathic Macular Telangiectasia (IMT)
- Age-related Macular Degeneration (AMD)
- Central Serous Chorioretinopathy (CSC)
- MEK Inhibitor-associated Retinopathy
- Uveal Effusion Syndrome (UES)
- Cavitary Optic Disc Anomalies
- Paraneoplastic Retinopathy
- Bilateral Diffuse Uveal Melanocytic Proliferation (BDUMP)
- Acute Paraneoplastic Polymorphous Vitelliform Maculopathy (AEPPVM)
- Polypoidal Choroidal Vasculopathy
- Optic Pits
- Retinopathy of Prematurity
Pathophysiology
The subretinal space, a remnant of the embryonic optic vesicle, is practically nonexistent in a healthy eye. However, pathologies that disrupt the integrity of the blood-retina barrier (BRB) can cause leakage of fluid that enlarges the subretinal space and separates the sensory retina from the RPE resulting in retinal detachment.[1]
The BRB has an inner and outer component. The inner blood-retina barrier (iBRB) is composed of tight junctions in between cells of the retinal endothelium whereas the outer blood-retina barrier (oBRB) is composed of tight junctions between cells of the RPE. [3]
Diagnosis
Diagnosis of ERD begins with a detailed history and ophthalmic exam.
History
ERD may develop from localized ocular disease or as a manifestation of wide-spread systemic disease and thus a thorough ocular and medial history is required.[1] Some patients report a progressive, fluctuating loss of peripheral vision. [4]
Physical Exam
Slit-lamp examination, dilated fundoscopy, and indirect ophthalmoscopy with scleral depression should all be performed. ERD can appear as shifting fluid beneath the retina. The fluid shifts with gravity and can change location according to patient position.[4] Exudative detachment looks smooth compared to a jagged, rhegmatogenous detachment.
Testing
Fluorescein angiography, Indocyanine green angiography (ICGA), Optical Coherence Tomography and echography aid in diagnosis. Blood tests, X-rays, CT scan, and Magnetic Resonance Imaging can identify systemic correlates that reveal the etiology.[1]
Diagnostic vitrectomy is crucial for infectious and neoplastic causes of ERD.
Management
Treatment
Unlike rhegmatogenous and tractional detachment which are treated surgically, ERD is generally treated medically. Treatment focuses on the underlying pathology causing the fluid buildup.
Medical
Immunosuppressive
For ERD caused by non-infectious uveitis (e.g. VKH syndrome), common treatment is high dose IV steroids followed by oral steroid taper. Intravitreal triamcinolone has also been used. Alternatives to steroids include cyclosporine A, azathioprine, methotrexate, mycophenolate mofetil and infliximab.[1]
Biologics
Tumor necrosis factor (TNF) alpha inhibitors (etanercept, infliximab, adalimumab), interferon alpha-2, interferon-beta, specific cell inhibitors (rituximab, daclizumab) and receptors antagonists (anakinra, efalizumab).
Anti-VEGF
Intravitreal bevacizumab (IVB) can be helpful for subretinal fluid exudation due to its anti-angiogenic and anti-permeability properties.[1]
Other
Eplerenone (mineralocorticoid receptor antagonist) for CSC.[1]
Interventional
Focal laser photocoagulation, cryotherapy, low-dose plaque radiotherapy, photodynamic therapy (PDT) and pars plana vitrectomy (PPV).
Prognosis
Prognosis for ERD is highly variable and heavily dependent on etiology. Acute, self-limited causes of ERD have a favorable prognosis whereas chronic, irreversible causes have a poor prognosis.[1] Prognosis is particularly poor if there is macular involvement and in cases of metastatic and paraneoplastic disease.
Additional Resources
https://www.aao.org/1-minute-video/shifting-fluid-in-patients-with-retinal-detachment
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Amer R, Nalcı H, Yalçındağ N, Exudative Retinal Detachment, Survey of Ophthalmology (2017), doi: 10.1016/j.survophthal.2017.05.001.
- ↑ Blair K, Czyz CN. Retinal Detachment. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551502/
- ↑ Cunha-Vaz J, Bernardes R, Lobo C. Blood-retinal barrier. Eur J Ophthalmol. 2011;21 Suppl 6:S3-9. doi: 10.5301/EJO.2010.6049. PMID: 23264323.
- ↑ 4.0 4.1 Fineman, M. S., & Ho, A. C. (2012). Color Atlas & Synopsis of Clinical Ophthalmology: Retina. Lippincott Williams & Wilkins.