Optic Pits
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
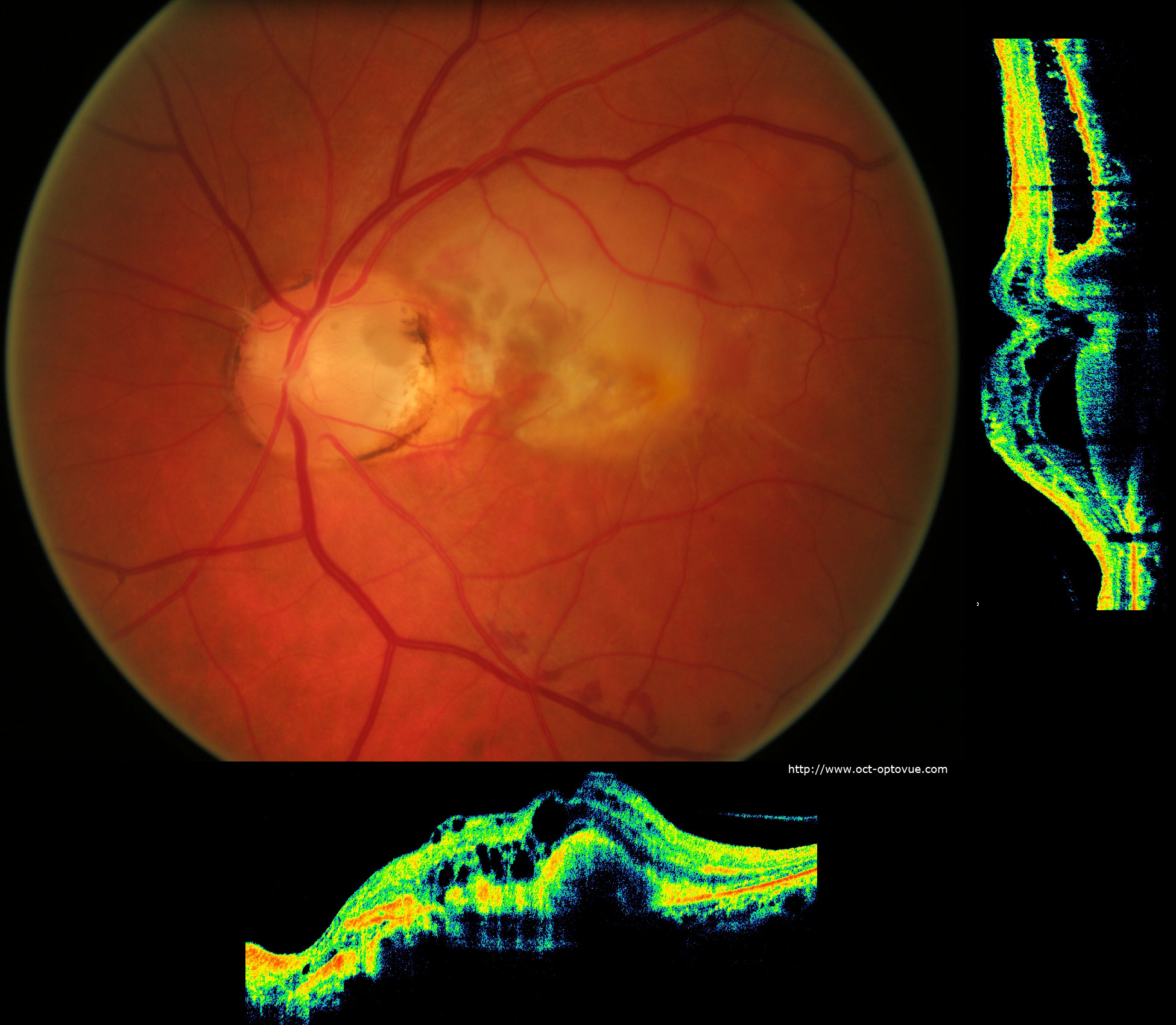
Optic Pits (also known as optic nerve pits, optic disc pits, or less commonly optic holes) are congenital defects presumably arising from the failure of fetal fissure closure in embryogenesis.
Disease Entity
Overview
Optic Disc Pits (ODP) were first described in 1882 by Wiethe in a 62-year-old female. Since then, they have typically been an incidental finding on routine dilated fundus exam. Rarely, they may cause visual field defects or macular changes.
Detailed description
An ODP usually presents itself as a unilateral, solitary, ovoid, grey-white excavation of the optic disc, most commonly in the inferotemporal quadrant of the nerve head. 15% of ODP’s are thought to occur bilaterally. The size of the pit can occupy 1/8 -1/4 of the size of the disc.[1]Depending on the optic disc size and location, they may cause arcuate field defects or an enlarged blind spot. Visual acuity is typically not affected unless macular involvement is present, either by a serous retinal detachment, retinal schisis or cystoid macular edema. [2]Patients with optic disc pit maculopathy initially notice a drop in visual acuity to around 20/70 in the affected eye.[2]
Epidemiology and risk factors
Optic nerve pits are a rare entity. In a study by Reis in 1908, the frequency of this anomaly was estimated to be 1 out of 11,000 people[1]. In a study by Wang el al, the prevalence was found to be 0.1%. [3] Of those with ODP, 25-75% experience visual symptoms . [2] Further, numerous studies report that 30-75% of optic disc pit patients may experience maculopathy.[4] They are thought to occur sporadically with no known risk factors in particular. Men and women are affected equally.
Etiology and pathophysiology
Optic pits are thought to be a result of incomplete closure of the superior edge of the embryonic fissure. This has been the subject of some debate in the literature. The mechanisms of subretinal fluid accumulation in optic disc pit maculopathy are not well understood. It has been postulated that the fluid may arise from one of several sources; the vitreous cavity, cerebrospinal fluid (CSF) , the surrounding orbital space or dural leaking vessels at the base of the pit .[5]
The membrane overlying the optic nerve pit demonstrates structural complexity, with some studies identifying it as glial tissue without evident defects, while others report the presence of holes, particularly at the temporal margin of the pit.[6][7] An intact membrane is thought to offer a protective role against maculopathy, whereas defects, such as those visualized via OCT, are associated with an increased risk of severe maculopathy due to potential fluid leakage into the subretinal space. [8]
As for the theory suggesting the fluid arising from vitreous cavity, pre-existing vitreous traction on the macula and the optic disc is thought to play a role in the development of negative pressure with subsequent entrance of fluid through the ODP into the submacular space. [9] Whereas, the theory of CSF leaking into the macular schisis or subretinal space is thought to be from a direct communication of the subarachnoid space through the ODP that transmits fluid into the intra- and subretinal space. [9]
Histopathology
On microscopic examination, there is usually herniation of the surrounding dysplastic retina and fibrous tissue into the meninges (subarachnoid space) and adjacent optic nerve through a defect in the lamina cribrosa.
Diagnosis
History
Patients are generally asymptomatic and findings are usually incidentally found on routine exam. However, patients may complain of metamophopsia, micropsia, blurred vision, or a noticeable blind spot if the optic pit is associated with a serous retinal detachment.[10]
Exam
Optic pits are generally found inferotemporally within the nerve, however up to one-third are central. They appear as a round or oval depression that differs in color from the surrounding disc (grey, yellow or black). [11] The color variation depends on the amount and location of the glial tissue in the pit. There may associated macular edema, serous macular detachment; schisis or pigmentary changes within the macula.
A pit can be seen with direct or indirect ophthalmoscopy. For detailed evaluation, slit lamp biomicroscopic binocular examination should be performed.
Shallow serous macular detachments can be seen in upto three-fourths of eyes with inferotemporal pits. They usually become symptomatic in the 3rd or 4th decade of life though reports in children have been described.
Investigations
Due to the incidental nature of this disc anomaly, investigations are usually done to diagnose, and to detect complications. Sub-retinal fluid, or macular schisis are complications that can be detected with a macular optical coherence tomography (OCT). Moreover, investigations are used to monitor for the success of treatment. Serial OCTs of the retinal nerve fiber layer along with serial Humphrey visual fields are beneficial to differentiate between ODP and other progressive optic neuropathies such as glaucoma. ODP can present with visual field deficits such as arcuate scotoma, central scotoma or an enlarged blind spot.
Fluorescein Angiography is not particularly useful in diagnosing optic pit, however it may be helpful in eliminating other diseases in the differential of serous detachment.
Fundus autofluorescence may reveal hyperfluorescence in a granular pattern due to subretinal precipitation, while areas of serous retinal detachment and inner retinal schisis typically appear as hypofluorescence.[12]
An Amsler grid can be used to monitor the onset of macular involvement of an optic pit with a serous detachment.
Differential diagnosis
DDx of Optic disc pits includes other congenital optic disc anomalies (optic disc coloboma, morning glory anomaly, hypoplastic disc or tilted discs), scleral crescent, circumpapillary staphyloma, and glaucomatous disc cupping.
DDx of optic nerve pit maculopathy include idiopathic central serous retinopathy, and subretinal neovascular membrane
Management and treatment
The first treatment modality is observation especially if there is no macular involvement. The patient is made aware of his condition and counselled with regards to the possibility of vision loss. Should the macula be affected, the treatment options include the following:
- laser photocoagulation: the objective of treatment includes repair of a serous detachment if occurred as a complication of an optic nerve pit. The technique includes laser application temporal to the disc area to create a barrier for fluid not to enter the macula. Laser photocoagulation therapy has not had much success in most studies, patients treated did not notice improvement, in fact some reported more visual disturbance after the treatment. [9]
- Surgical options: most commonly, a pars plana vitrectomy (PPV) is performed, with or without internal limiting membrane peel, with or without endolaser, and gas tamponade. The success of this method is based on the theory of vitreous traction leading to formation of fluid (discussed earlier). Studies have shown promising long-term results in both retinal re-attachments (50-95% of patients) and visual improvement(>50% of patients). [9] Human amniotic membrane patch graft implant into the pit during vitrectomy with air tamponade has been successful in many series. [13] [14]Injection of platelets into the ODP area following PPV has demonstrated improved outcomes in cases of ODP-related macular detachment.[15]
A emerging surgical technique for managing ODP’s is PPV combined with inverted ILM flap to cover the optic disc and the ODP. This technique has shown promising results however evidence remains low due to the limited studies. [9]
There are studies that reported high success rates with injecting gas tamponade with or without barrier laser at the temporal disc edge. There was 50-75% fluid resolution and significant vision improvement, however there was a need for re-injection of gas frequently due to recurrence. [9]
Macular buckle is an option of treatment to promote reattachment of the macula via ab externo compression when detachment involves the macula. This procedure is considered technically challenging despite the good anatomical and visual outcomes hence it is not widely applied. [9]
Performing inner retinal fenestrations to create passage for the fluid to travel to the vitreous have been reported, showing fluid resolution in 95%, and vision improvement in 56%. Controlled active aspiration of the intraretinal fluid using a 38 gauge cannula for treatment of foveoschisis has been recently described.[16]
When optic disc pits lead to serous maculopathy, a more comprehensive treatment approach may be necessary. Below are the clinical features and management options for this specific complication:
Serous maculopathy associated with optic nerve head pits
History: Wiethe was the first one to describe this condition in 1882. Clinical Features: It is seen as greyish-white excavation in optic nerve head, often in the temporal disc.
- Size of the disc is normal
- Subretinal fluid extending from disc and involving macula which may wax and wane naturally without intervention
Pathophysiology: Subretinal fluid origin is debated, but derivation is thought to be from:
- Vitreous
- Subarachnoid space
- Abnormal vessels from base of the pit
Treatment:
- Observation
- Intravitreal gas injection
- Pars plana vitrectomy with many possible components or combination of components, including:
- Laser photocoagulation along the temporal disc margin
- Internal limiting membrane peeling, sometimes laying the membrane graft over the pit defect
- Air-fluid exchange
- Intravitreal gas injection
- Injection of autologous platelet-rich plasmin or fibrin glue into the optic pit has been reported
Serous maculopathy associated with dysplastic disc
Clinical Features: Disc dysplasia, or an abnormally-looking disc that does not fit into any other recognizable category
Pathophysiology: Could be similar to that of optic nerve head pit
Management: Photocoagulation along temporal margin of disc has been described
Prognosis
The presence of an optic disc pit has good to poor prognosis depending on clinical findings and complications. Isolated optic pits have an excellent prognosis and usually have no sequelae. Should a patient develop optic disc maculopathy, 80% will progress to a visual acuity of 20/200 or worse. Without treatment, reduction in visual acuity due to optic disc maculopathy typically manifests within 6 months. [17] (Favorable anatomic and functional results have been reported after surgery with an 87% success rate reported recently in the literature.
References
- ↑ Jump up to: 1.0 1.1 Gordon R, Chatfield RK. Pits in the optic disc associated with macular degeneration. The British journal of ophthalmology. 1969;53(7):481–9.
- ↑ Jump up to: 2.0 2.1 2.2 Optic disc pit: a review. Source: Graefe's archive for clinical and experimental ophthalmology [0721-832X] Georgalas, Ilias yr:2011 vol:249 iss:8 pg:1113 -1122.
- ↑ Wang Y, Xu L, Jonas JB. Prevalence of congenital optic disc pits in adult Chinese: The Beijing Eye Study.
- ↑ Oli A, Balakrishnan D. Treatment outcomes of optic disc pit maculopathy over two decades. Ther Adv Ophthalmol. 2021;13:25158414211027715. Published 2021 Jun 30. doi:10.1177/25158414211027715
- ↑ Ferry AP (1963) Macular detachment associated with congenital pit of the optic nerve head. Pathologic findings in two cases simulating malignant melanoma of the choroid. Arch Ophthalmol 70:346–357
- ↑ Bonnet M. Serous macular detachment associated with optic nerve pits. Graefes Arch Clin Exp Ophthalmol. 1991;229(6):526–532.
- ↑ Brockhurst RJ. Optic pits and posterior retinal detachment. Trans Am Ophthalmol Soc. 1975;73:264–291.
- ↑ Doyle E, Trivedi D, Good P, Scott RA, Kirkby GR. High-resolution optical coherence tomography demonstration of membranes spanning optic disc pits and colobomas. Br J Ophthalmol. 2009;93(3):360–365.
- ↑ Jump up to: 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Chatziralli I, Theodossiadis P, Theodossiadis GP. Optic disk pit maculopathy: Current management strategies. Vol. 12, Clinical Ophthalmology. Dove Medical Press Ltd; 2018. p. 1417–22.
- ↑ Christoforidis JB, Terrell W, Davidorf FH. Histopathology of optic nerve pit-associated maculopathy. Clin Ophthalmol. 2012;6:1169-1174. doi:10.2147/OPTH.S34706
- ↑ Ashourizadeh H, Grinspan N, Armstrong GW. Color fundus photography interpretation of ophthalmic findings. EyeWiki. Available at: https://eyewiki.org/Color_Fundus_Photography_Interpretation_of_Ophthalmic_Findings#Optic_Nerve_Pit. Accessed September 22, 2024.
- ↑ Schiefer C, Kaleem MA, Aouchiche R. Diagnosis and management of optic disc pits. EyeNet Magazine. February 2020. Available at: https://www.aao.org/eyenet/article /diagnosis-and-management-of-optic-disc-pits. Accessed September 22, 2024.
- ↑ Rizzo S, Caporossi T, Pacini B, De Angelis L, De Vitto ML, Gainsanti F. Management of Optic Disk Pit-associated Macular Detachment with Human Amniotic Membrane Patch. Retina. 2023 Jan 1;43(1):144-147.
- ↑ Caporossi T, D'Amico G, Tartaro R, Governatori L, Scampoli A, Amorelli G, De Vico U, Rizzo S. Optic Disk Pit Maculopathy Treatment Using a Human Amniotic Membrane Patch: One-Year Results. Am J Ophthalmol. 2022 Aug;240:30-36.
- ↑ Ooto S, Mittra RA, Ridley ME, Spaide RF. Vitrectomy with inner retinal fenestration for optic disc pit maculopathy. Ophthalmology. 2014;121(9):1727-1733. doi:10.1016/j.ophtha.2014.04.006
- ↑ El Rayes EN, Habib AM, Soliman AH, Ibrahim OM, El Sawwah KMH. Novel Technique for Treatment of Foveoschisis Associated With Optic Disk Pits: Active Aspiration of Intraretinal Fluid. Retina. 2022 Jul 1;42(7):1406-1410.
- ↑ Sobol WM, Blodi CF, Folk JC, et al. Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology 1990; 97: 1539–1542.
- Annesley, W, Brown, G, Bolling, J, Goldberg, R, Fischer, D. “Treatment of retinal detachment with congenital optic pit by krypton laser photocoagulation.” Graefe's Archive for Clinical and Experimental Ophthalmology 1987; 225:5.
- Brown, G, Tasman, W. Congenital anomalies of the optic disc. Grune & Stratton, New York 1983, p. 31.
- Brown, GC, Shields, JA, Goldberg, RE. “Congenital pits of the optic nerve head.” Clinical studies in humans. Ophthalmology 1980; 87:51.
- Creel, D. “Clinical Electrophysiology.” http://retina.umh.es/Webvision/ClinicalERG.html
- Ferry, AP. “Macular detachment associated with congenital pit of the optic nerve head.” Arch Ophthalmol 1963; 70:346.
- Hirakata A, Okada AA, Hida T. “Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit.” Ophthalmology. 2005 Aug;112(8):1430-5.
- Magli A, Greco A, Alfieri MC, Pignalosa B. “Hereditary colobomatous anomalies of the optic nerve head.” Ophthalmic Paediatr Genet. 1986 Aug;7(2):127-30.
- Ooto S, Mittra RA, Ridley ME, Spaide RF. Vitrectomy with inner retinal fenestration for optic disc pit maculopathy. Ophthalmology. 2014
- Park SC, De Moraes CG, Teng CC, Tello C, Liebmann JM, Ritch R. “Enhanced depth imaging optical coherence tomography of deep optic nerve complex structures in glaucoma.” Ophthalmology. 2012 Jan;119(1):3-9.
- Reed D. (1999) Congenital pits of the optic nerve. Clin Eye Vis Care. 1999 11(2):75–80.
- Sadun, AA. “Optic Disc Pits and Associated Serous Macular Detachment.” Medical Retina 4th Ed., 2005, Chapter 111.
- Slusher MM, Weaver RG Jr, Greven CM, Mundorf TK, Cashwell LF. “The spectrum of cavitary optic disc anomalies in a family.” Ophthalmology. 1989 Mar;96(3):342-7.
- Stefko ST, Campochiaro P, Wang P, Li Y, Zhu D, Traboulsi EI. Dominant inheritance of optic pits. Am J Ophthalmol 1997; 124(1):112–113.
- Theodossiadis GP, Theodossiadis PG. “Optical coherence tomography in optic disk pit maculopathy treated by the macular buckling procedure.” Am J Ophthalmol. 2001 Aug; 132(2):184-90.
- Theodossiadis GP, Theodossiadis PG. “The macular buckling procedure in the treatment of retinal detachment in highly myopic eyes with macular hole and posterior staphyloma: mean follow-up of 15 years.” Ophthalmology. 2005 Aug; 112(8):1430-5.