Retinal Detachment
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Retinal detachment is a sight threatening condition with an incidence of approximately 1 in 10000.[2] [3] Before the 1920’s, this was a permanently blinding condition. In subsequent years, Jules Gonin, MD, pioneered the first repair of retinal detachments in Lausanne, Switzerland.[4] In 1945 after the development of the binocular indirect ophthalmoscope by Charles Schepens, MD, techniques for retinal detachment repair improved. In the last 50 years techniques in scleral buckling, pneumatic retinopexy and vitrectomy have made the repair of retinal detachments significantly more manageable with better visual outcomes.
Risk Factors for Rhegmatogenous Retinal Detachment
- Lattice degeneration
- Peripheral retinal breaks
- Pathologic myopia
- Previous intraocular surgery
- Trauma
- Previous retinal detachment
- Family history
Lattice degeneration is considered the most important peripheral retinal degeneration process that predisposes to a rhegmatogenous retinal detachment.[5] Other peripheral lesions having slight increased risk of retinal detachment include ora bays, meridional folds and complexes, and cystic retinal tufts.
Pathophysiology
Normally, the retinal pigment epithelium (RPE) is able to maintain adhesion with the overlying neurosensory retina through a variety of mechanisms. These mechanisms include active transport of subretinal fluid across RPE , metabolic activity of RPE, and interdigitation of the photoreceptor outer segments and the RPE microvilli. With retinal detachment, these mechanisms are overwhelmed leading to separation of the neurosensory retina from the retinal pigment epithelial layer.
Retinal detachment occurs when subretinal fluid accumulates between the neurosensory retina and the retinal pigment epithelium. This process can occur in three ways. One mechanism involves occurrence of a break in the retina allowing liquified vitreous to directly enter the subretinal space. This is known as a rhegmatogenous retinal detachment. Rhegmatogenous retinal detachments are often due to retinal tears associated with posterior vitreous detachment or trauma.
Although this monograph focuses on rhegmatogenous retinal detachment, it is pertinent to note the other major causes of retinal detachment. A second mechanism involves proliferative membranes on the surface of the retina or vitreous. These membranes can pull on the neurosensory retina causing a physical separation between the neurosensory retina and retinal pigment epithelium. This is called a tractional retinal detachment. Tractional retinal detachments can be seen in proliferative retinopathy due to diabetic disease, sickle cell and other disease processes leading to neovascularization of the retina. Tractional retinal detachments can also be due to proliferative vitreoretinopathy after trauma or surgery. The third mechanism for retinal detachment is due to accumulation of subretinal fluid due to inflammatory mediators or exudation of fluid from a mass lesion or insufficient RPE function. This mechanism is known as a serous or exudative retinal detachment. Serous detachments are caused by a number of inflammatory, or exudative retinal disease processes such as Sarcoidosis, medication toxicity, myeloma, or choroidal neoplasms. Serous retinal detachments may also be the presenting sign in patients with aggressive metastatic cancer, such as testicular cancer.[6]
Primary Prevention
Patients with known risk factors for retinal detachment should have serial dilated fundus examinations with scleral depression, often yearly. Protective eyewear is recommended for individuals with high myopia that participate in contact sports. Patients undergoing cataract surgery should be counseled about the importance of reporting symptoms of retinal tears and detachments.
Diagnosis
History
Patients who present with symptoms of new onset significant photopsias and/or persistent new floaters should be suspected of having a retinal tear, which could lead to a retinal detachment. A patient with constant fixed or slowly progressive visual field loss should be suspected of having a detachment until proven otherwise. Important information in the history includes onset of symptoms, presence and duration of decreased central visual acuity, prior trauma, prior surgery, hemorrhage, and a complete past medical history and review of systems.
Physical examination
Visual acuity, pupillary examination, visual field testing and intraocular pressure measurement are important parts of the pre-dilated ophthalmic examination to evaluate patients with symptoms of retinal detachment. Additional examination to include color vision in the visual field.
Slit lamp examination of the anterior segment should be completed prior to dilation. Examination of the anterior vitreous for pigment (Schaffer's sign) or vitreous hemorrhage is critical. A thorough fundus examination to include indirect ophthalmoscopy with scleral depression and visualization to the ora serrata should be completed. A detailed drawing describing the detachment with location of retinal pathology may be documented.
If there is no view to the posterior pole such as in hemorrhage or media opacity, B-scan ultrasound should be used to evaluate the retinal and vitreous status.
Clinical diagnosis
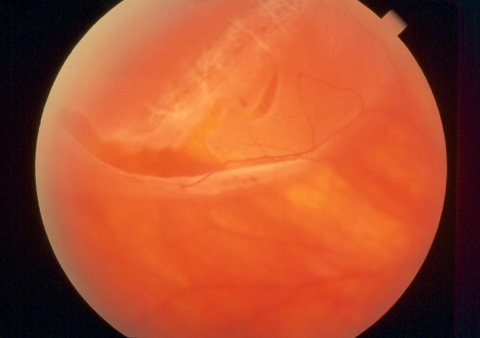
Rhegmatogenous retinal detachment has a characteristic appearance differentiating it from a tractional or serous detachment. A rhegmatogenous retinal detachment has a corrugated appearance and undulates with eye movements. Tractional detachments have smooth concave surfaces with minimal shifting with eye movements. Serous detachments show a smooth retinal surface and shifting fluid depending on patient positioning. In the vast majority of cases, a retinal break will be identified with proper examination, thus confirming a rhegmatogenous retinal detachment. Without visualization of a retinal break, the diagnosis of rhegmatogenous retinal detachment should be questioned, however there are cases where the retinal break is obscured by vitreous hemorrhage or other media opacities; occasionally the offending retinal breaks are too small to visualize.
Laboratory/Ancillary testing
Rhegmatogenous retinal detachment is a clinical diagnosis. Where available, it is sometimes appropriate to examine and document macula status with ocular coherence tomography and/or wide field fundus photography. Additionally, in cases of media opacities, B-scan ultrasound is indicated and may be a critical diagnostic tool.
Laboratory testing is typically only indicated in traction or exudative detachments. If a cause for the traction retinal detachment cannot be determined by history, further laboratory analysis may be required to determine if diabetes, sickle cell, carotid disease or another systemic or ocular process is the source for proliferative retinopathy. Since exudative detachments may be due to a systemic or ocular inflammatory process, laboratory investigation may be indicated. In these cases, fluorescein angiography may be indicated to further clarify exudative processes such as macular degeneration, central serous chorioretinopathy, and Vogt-Koyanagi-Harada syndrome or other uveitic processes. Ultrasound is a useful imaging modality to evaluate choroidal masses or posterior scleritis.
Differential diagnosis
The differential diagnosis of retinal detachment includes retinoschisis and choroidal mass. Rhegmatogenous retinal detachment is most often confused with retinoschisis and serous retinal detachment. Retinoschsis can be distinguished from retinal detachment by appearance on ultrasound, the presence of inner layer dots (Muller footplates), uptake of photocoagulation with retinoschisis, and absolute scotoma with retinoschisis versus relative scotoma in retinal detachment. Choroidal masses can be distinguished from retinal detachment by observing the characteristics of imaging with ultrasound. In addition, retinal detachments may be associated with other findings include choroidal detachment and macular hole.[7]
Management
General treatment
Once a retinal detachment has been identified, one must determine what type of detachment is present. Surgical management is indicated for rhegmatogenous and tractional detachments.
For rhegmatogenous detachments, all retinal breaks should be identified, treated and closed. Techniques for repair include laser retinopexy, pneumatic retinopexy, scleral buckle or vitrectomy, or combinations of these techniques.
- Laser retinopexy is typically reserved for small, localized detachments in which laser barricade can be safely performed without interfering with the patient’s visual function while preventing propagation of the detachment.
- Pneumatic retinopexy involves the injection of an intraocular gas bubble along with retinopexy using cryotherapy or laser, typically in a clinic setting. An important part in the successful repair of retinal detachment with pneumatic retinopexy involves head positioning so that the gas bubble tamponades the retinal tear. Pneumatic retinopexy is typically only used with retinal detachments due to retinal tears in the superior eight clock hours and involving a single break less than one clock hour, although exact criteria are controversial and largely depend on surgeon and patient factors.
- Scleral buckles are silicone bands permanently placed around the outside of the globe under the extraocular rectus muscles to relieve any traction and support retinal tears. Scleral buckling is combined with retinopexy, typically cryotherapy. This is the oldest method of repair and still has excellent results in well-trained hands. This procedure is performed in the operating room.
- Pars plana vitrectomy with 20 gauge, 23 gauge, 25 gauge, or 27 gauge instruments involves removal of the vitreous by way of cutting the vitreous strands with a vitrectomy machine/handpiece and flattening of the retina through a direct intraocular process.
In tractional detachments, tractional elements (usually epiretinal or subretinal membranes) must be relieved. This is typically accomplished with pars plana vitrectomy, but may be combined with scleral buckling as an adjunct.
For serous detachments, management is nonsurgical. Any inflammatory disease or underlying mass should be identified and treated if possible.
Complications
Proliferative retinopathy (PVR) is the most common cause of repair failure and occurs in about 8–10% of patients undergoing primary retinal detachment repair. [8] [9] Risk factors for PVR include:
- Age
- Giant retinal tears
- Retinal detachments involving more than 2 quadrants
- Previous retinal detachment repair
- Use of cryotherapy
- Vitreous hemorrhage
- Choroidal detachment[10]
- Trauma
PVR requires surgical intervention to release the traction caused by membranes and has a poor visual prognosis.[11]
Additional Resources
- Gudgel DT, Boyd K, McKinney JK. Flashes of Light. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/symptoms/flashes-of-light-list. Accessed March 13, 2019.
- Boyd K, Maturi RK. Retinal Detachment. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/retinal-detachment-list. Accessed March 25, 2019.
- http://www.asrs.org/
References
- ↑ American Academy of Ophthalmology. Retinal detachment. https://www.aao.org/image/retinal-detachment-4 Accessed July 26, 2019.
- ↑ Haimann MH, Burton TC, Brown CK. Epidemiology of retinal detachment. Arch Ophthalmol. Feb 1982; 100(2):289-92.
- ↑ Go SL, Hoyng CB, Klaver CC. Genetic risk of rhegmatogenous retinal detachment: a familial aggregation study. Arch Ophthalmol. 2005; 123: 1237-41.
- ↑ Gonin J. Treatment of detached retina by searing the retinal tears. Arch Ophthalmol 1930;4:621-625.
- ↑ Lewis H. Peripheral Retinal Degenerations and the Risk of Retinal Detachment. Am J Ophthalmol 2003; 136:155–160.
- ↑ Phelps, P. O., et al. "Metastatic mixed germ-cell neoplasm presenting as retinal detachment." Journal of clinical oncology: official journal of the American Society of Clinical Oncology 30.13 (2012): e133.
- ↑ Tsui JC, Brucker AJ, Kolomeyer AM. RHEGMATOGENOUS RETINAL DETACHMENT WITH CONCURRENT CHOROIDAL DETACHMENT AND MACULAR HOLE FORMATION AFTER UNCOMPLICATED CATARACT EXTRACTION AND INTRAOCULAR LENS IMPLANTATION: A CASE REPORT AND REVIEW OF LITERATURE. Retin Cases Brief Rep. 2024;18(2):168-172. doi:10.1097/ICB.0000000000001359
- ↑ Brucker AJ, Hopkins TB. Retinal Detachment Surgery: The Latest in Current Management. Retina. 2006; 26: S28-S33.
- ↑ Leaver PK. Proliferative vitreoretinopathy. Br J Ophthalmol. 1995 October; 79(10): 871–872.
- ↑ Tsui JC, Brucker AJ, Kim BJ, Kolomeyer AM. COMBINED RHEGMATOGENOUS RETINAL AND CHOROIDAL DETACHMENT: A Systematic Review. Retina. 2023;43(8):1226-1239. doi:10.1097/IAE.0000000000003770
- ↑ Girard P, Mimoun G, Karpouzas I, et al. Clinical risk factors for proliferative vitreoretinopathy after retinal detachment surgery. Retina. 1995; 14:417–424.