Coronavirus (COVID-19)
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
This page is undergoing major revisions to address the latest knowledge and understanding about the SARS-CoV-2 virus and COVID-19.
For ocular associations with COVID-19 and related vaccines, see Ophthalmology Related Coronavirus EyeWiki Articles.
Ophthalmology-Related Topics
- COVID Conjunctivitis
- COVID-19 Associated Orbital Mucormycosis
- COVID-19 and Glaucoma Management
- Ocular Adverse Reactions after Receiving COVID-19 Vaccine
- Optic Neuropathy after COVID-19
- Retinal Manifestations of COVID-19
American Academy of Ophthalmology Update
The Academy has daily updates on this evolving situation: Important coronavirus updates for ophthalmologists (American Academy of Ophthalmology, San Francisco, 2020).
Disease Entity
Coronavirus Disease 2019 (COVID-19) is the official name given by the World Health Organization (WHO) for the infectious disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).[1] The disease was first identified in Wuhan, China in December 12 2019, then rapidly spread worldwide, and a pandemic was declared on March 11, 2020. [2] An excellent summary of the disease in a Nature news article is available on line[3]
It has been reported that ophthalmologists and ear, nose, and throat specialists in Wuhan, China were at increased risk of acquiring COVID-19. [4] Numerous ophthalmologists and ophthalmology trainees have become ill with and died from proven or suspected COVID-19. [5]
Disease
Signs and symptoms
After a patient is exposed to SARS-CoV-2, the incubation period typically lasts for 1-14 days (with an estimated mean of 5-6 days) before they develop symptoms. According to the WHO-China Joint Mission on Coronavirus Disease 2019, the most common signs and symptoms in 55,923 cases were:[6]
- Fever(87.9%)
- Dry cough (67.7%)
- Fatigue (38.1%)
- Sputum production (33.4%)
- Shortness of breath (18.6%)
- Sore throat (13.9%)
- Headache (13.6%)
- Myalgia or arthralgia (14.8%)
- Chills (11.4%)
- Nausea or vomiting (5.0%)
- Nasal congestion (4.8%)
- Diarrhea (3.7%)
- Hemoptysis (0.9%)
- Conjunctivitis or conjunctival congestion (0.8%)
Giant cell arteritis (GCA) and COVID-19 share many common symptoms, and thus clinicians and especially ophthalmologists need to conduct a thorough review of systems. Both can present with headache, fatigue, myalgia but vision loss and jaw claudication are specific for GCA only.[7]
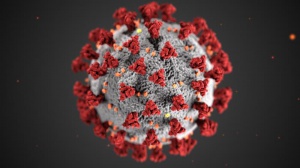
Etiology
COVID-19 is caused by an infection with SARS-CoV-2. This β-coronavirus is an enveloped positive-sense single-stranded RNA virus of the subfamily Orthocoronavirinae of the Coronaviridae family.[8][9] Bat was thought to be the natural reservoir of this virus, as the outbreak began in a seafood market in Wuhan, China, where several wild animal species including bat were sold on a daily basis. Of note, bat was also reported to be the culprit of SARS and MERS epidemics in 2002 and 2012, respectively.[10][11][12] Direct contact with intermediate hosts or consumption of wild animals is likely the initial route of SARS-CoV-2 transmission, and transmission from animals remains a source of concern. Human-to-human transmission is the key factor for rapid spread of SARS-CoV-2, while nosocomial transmission was the most common route of infection for SARS and MERS.[13][14]
Risk Factors
Advanced age is the primary risk factor for developing COVID-19. Older patients also have higher mortality. [15] Zhou et al. show that patients who required admission for COVID-19 at a hospital in Wuhan more likely presented with systemic co-morbidities including hypertension (30%), diabetes (19%), coronary artery disease (8%), COPD (3%).[16]
Pathophysiology
Person-to-person transmission via respiratory droplets is believed to be the primary method, similarly to other Coronavirus and other comparable viruses such as influenza. Transmission may potentially occur through the eyes ,[17] via the fecal-oral route, and via fomites (human contact and inanimate objects). Animals (dogs, cats, livestock are a potential but unproven source of transmission to humans.
Multiple respiratory droplets may be released when an infected person coughs, sneezes or speaks. Once a respiratory droplet exits an infected individual it can be directly inhaled by another person. Droplets can also contaminate surfaces which may be touched by another person. Transmission occurs when viral particles from the respiratory droplets contact host mucus membranes. Upon contact an epithelial cell, the virus particle gains entry inside using the SARS-CoV-2 spike (S) glycoprotein which binds to the cell membrane protein angiotensin-converting enzyme 2 (ACE2). The S glycoprotein is composed of 2 subunits S1 and S2. The S2 subunit is shown to be highly conserved with a fusion peptide, a transmembrane domain and a cytoplasmic domain. This could serve as a target for producing antiviral drugs.
Once inside, the virus starts to transcribe its genome and synthesize many proteins required for rapid replication. Among the protein products, the non-structural proteins (nsp) are particularly important for pathophysiology of COVID-19, as they have the ability to disable the host's innate immune response.[8] [18][19]
Social distancing
It is crucial to keep hand hygiene and practice "social distancing" to stop the spread of SARS-CoV-2. It has been shown that SARS-COV-2 remained viable in aerosol for up to three hours, so airborne precautions with full personal protective equipment (PPE) is strongly recommended, particularly in case requiring aerosol generating procedure. Additionally, the researchers have shown that SARS-CoV-2 survives on stainless steel and plastic for up to 72 hours, cardboard for up to 24 hours, and copper for up to 4 hours.[20]
Vaccination
On December 13th 2020, the US Food and Drug Administration (FDA) issued an emergency use authorization for a COVID-19 vaccine developed by Pfizer and BioNTech after it was shown to be 95% effective against COVID-19 in phase 3 clinical trials. This mRNA vaccine, approved for people 16 years or older, targets the spike (S) glycoprotein and hence blocks the SARS-CoV-2's entry into the cells. Given the new mRNA technology, this vaccine does not carry live virus and will not cause infection in the vaccinated individuals. Currently, this vaccines are given in 2 doses that are 21 days apart with 4 days of grace period, and protection is thought to start on day 28 after the first dose. It is also recommended for people with a history of asymptomatic or symptomatic COVID-19 infection, as data from phase 2 and 3 clinical trials showed both efficacy and safety in these groups.[21][22] The same vaccine was approved for use in the UK on December 3rd 2020.
Similarly, the US FDA authorized the use of mRNA-1273, a COVID-19 vaccine developed by Moderna, for emergency use in individuals 18 years or older. The decision came after this vaccine showed efficacy in 94.1% in clinical trials. In their primary efficacy analysis, all 30 severe cases (defined by either clinical signs of severe systemic illness, a diagnosis of respiratory failure or acute respiratory distress syndrome, significant acute renal/hepatic/neurologic dysfunction, admission to an intensive care unit or death) were from the placebo group. The most common adverse effects were: pain at injection site (88.2%), erythema (8.6%), swelling (12.2%) and ipsilateral lymphadenopathy (14.2%). Moderna vaccines are currently given in 2 doses 28 days apart - another key difference between this and the Pfizer/BioNTech vaccine.[23]
Other vaccines currently in Phase 3 clinical trials were developed by AstraZeneca and Janssen.
Diagnosis
History
A detailed history should include documentation of risk factors such as:
- Presence of fever or any respiratory symptoms including but not limited to cough, sputum production, hemoptysis, sore throat, headache, fatigue, myalgia.
- Presence of conjunctivitis symptoms including red eye, itchiness, tearing, foreign body sensation, photosensitivity, swollen eyelids.
- Close contact with an individual with known or suspected COVID-19 or pneumonia of unknown cause
- Residence in—or travel to—an area with widespread ongoing transmission, including: New York, New Jersey, California, Washington, New Orleans, as well as China, Iran, South Korea, and most of Europe.
- History of chronic systemic diseases including hypertension, diabetes, or immunocompromised state.
Physical Examination
Conjunctivitis has been identified as an infrequent ophthalmic sign of Covid-19, with the virus being isolated from tears and conjunctival secretions. Only 8 out of 121 COVID-19 cases seen in a hospital in Wuhan, China showed ocular symptoms and findings. However, the majority of these cases occurred in patients with more severe or critical respiratory disease . These patients were also found to have higher levels of white blood cells, neutrophils, lactic dehydrogenase, and C-reactive protein. However, ocular signs, symptoms and viral detection in conjunctival swab were not found to correlate with the duration of COVID-19.[24]
Signs
The most common exam findings as detailed by Wu et al. in a study in Hubei, China included:[24]
- Conjunctival hyperemia
- Follicles
- Chemosis
- Epiphora
- Increased secretions
Symptoms
The most common symptoms as detailed by Zhou et al. included:[25]
- Itching (62.5%)
- Redness (37.5%)
- Tearing (37.5%)
- Discharge (25%)
- Foreign body sensation (25%)
Other reported ocular associations
- Episcleritis[26]
- Panuveitis[27]
- Optic neuritis [27][28][29][30][31] with one bilateral case associated with anti-MOG antibody[32]
- Papilledema associated with idiopathic intracranial hypertension[33] or cerebral venous thrombosis[34]
- Cranial nerve palsies: CN III[35], CN IV[36], CN VI[37][38]. One case was reported with both CN III and VI[38] palsies.
- Central retinal artery occlusion[39][40]
- Central retinal vein occlusion[41] with 1 reported bilateral case[42]
- Guillan-Barre/Miller Fisher syndrome with complete ophthalmoplegia[43]
Clinical Diagnosis
Conjunctivitis due to SARS-CoV-2 can be diagnosed clinically based on signs and symptoms in the settings of exposure to COVID-19.
Diagnostic procedures
SARS-CoV-2 can be detected in tears or conjunctival swab via PCR testing. However laboratory testing is rarely done in ocular-asymptomatic patients given low sensitivity.[44]
Laboratory test
FDA-approved COVID-19 tests are listed on the FDA Emergency Use Authorizations page [45] PCR testing of nasopharygeal swab samples is notoriously unreliable, with false negatives of up to 40%, in part do to improper collection methods. More detailed information on serologic antibody tests, including sensitivity and specificity, are available at the FDA's EUA Authorized Serology Test Performance page, [46] although censorship by the Federal Government [47] calls into question the reliability of any health information coming from Federal agencies.
If clinical suspicion for COVID-19 is high in the setting of a negative PCR test, one should consider repeating the test in 1-2 days or obtaining a CT chest. Nasopharyngeal swabs have a higher diagnostic yield than oropharyngeal. Test positivity is most likely obtained if performed within the first week of symptom onset.
SARS-CoV-2 is infrequently detected in tears or conjunctival secretions. [44]
Differential diagnosis
Other viral illnesses including but not limited to influenza and respiratory syncytial virus (RSV) likely elevate the need for classify illnesses with higher degree of certainty with lab testing given similar presentations.
Management
Medical therapy
Randomized clinical trials are underway for a number of COVID-19 treatments, but at present clinical decisions must be made based upon limited data. The National Institutes of Health "Coronavirus 2019 (COVID-19) Treatment Guidelines," (updated 4/21/2020), states that "there are insufficient data to recommend either for or against any antiviral or immunomodulatory therapy in patients with COVID-19" illness. [48]
A recent study demonstrated that treatment with interferon beta-1b, lopinavir-ritonavir, and ribavirin " was safe and superior to lopinavir–ritonavir alone in alleviating symptoms and shortening the duration of viral shedding and hospital stay in patients with mild to moderate COVID-19, cutting clinical recovery time in half, viral shedding time by 40% and hospitalization duration by one third " [49] No patients died during this study so that it provided no information on the effect of the medication combination on mortality.
Pre-publication results from the National Institute of Allergy and Infectious Diseases (NIAID) Adaptive COVID-19 Treatment Trial (ACTT) study show that for patients with "Advanced COVID-19 and lung involvement," those treated with Remdesivir "had a 31% reduction in time to recovery than those who received placebo (11 days vs. 15 day for placebo, p<0.001) and "suggested a survival benefit, with a mortality rate of 8.0% for the group receiving remdesivir versus 11.6% for the placebo group (p=0.059)". [50] In another recent study, remdesivir did not have a statistically significant benefit ("clinical improvement, mortality, or time to clearance of virus") to patients with severe COID-19 disease [51]
The Massachusetts General Hospital COVID-19 Treatment Guide (updated 5/8/2020) notes that "for patients with evidence of cytokine release syndrome, with ID input, tocilizumab (Actemra) can be considered, and "for patients with evidence of sHLH-like features , with ID input, anakinra (Kineret) can be considered[52].
Current National Institute of Health COVID-19 Treatment Guidelines, Therapeutic Options for COVID-19 Currently Under Investigation. Summary Recommendations includes the recommendation against use of the combination of azithromycin plus hydroxychloroquine because of potential toxicities. [53] The Massachusetts General Hospital COVID-19 Treatment Guide (updated 5/8/2020) indicates that they "generally favor not initiating [hydroxychloroquine] outside of clinical trial but it may be considered on a case by case basis." [54] A retrospective Veteran's Administration study found "overall increased mortality ... in patients treated with hydroxychloroquine alone." [55] An observational study of 1,446 patients at New York Presbyterian Columbia showed no effect of hydroxychloroquine on rates of intubation or death. [56] An observational study of 1,438 patients showed that "among patients hospitalized in metropolitan New York with COVID-19, treatment with hydroxychloroquine, azithromycin, or both, compared with neither treatment, was not significantly associated with differences in in-hospital mortality." [57]
Postexposure Prophylaxsis
Inhalational aerosol/droplet exposure
There is currently no proven postexposure prophylaxis for COVID-19 [58] For patients and personnel exposed to COVID-19, clinical trials are underway. [59] Exposed personnel should self quarantine for 14 days. The National Institutes of Health "Coronavirus 2019 (COVID-19) Treatment Guidelines," (updated 4/21/2020), states that "at present, no agent is known to be effective for preventing SARS-CoV-2 infection after an exposure."
Ocular exposure to droplets or blood
For patients and healthcare workers with ocular exposure (e.g. due to close proximity coughing droplets or blood splash), consider immediate irrigation (perhaps with repeat irrigation five minutes later) with 5% povidone iodine or an ophthalmic preparation containing 0.2% benzalkonium chloride (e.g. latanaprost (Xalatan)) [60] and although bloodborne transmission of COVID-19 has not been reported (as per Dr. James Chodosh) consideration could be given to self quarantine for 14 days.
Surgery
For cases of emergent certain orbital fracture/open globe/penetrating/perforating injuries/large PKP dehiscence with concomitant or reasonable risk of expulsion, particular caution must be taken for the risks of deep nasopharyngeal swab encouraging further damage to the eye from reflex cough or Valsalva. This likely necessitates categorical use of N95 respirator masks or PAPR and avoidance of swabbing. The difficulties of PAPR use for microscopic delicate work present particular difficulties as certain equipment designs not easily accommodate ocular instrument use.
Surgical follow up
Follow up of any urgent/emergent surgery for COVID-19 positive patients necessitate dual agreement of masking both staff and patients in isolated designated workflow areas that can accommodate patients separately from non COVID-19 patients. These are frequently driven by facility protocols and require novel workflow operational design.
Prognosis
In the United States, between February 12 and March 16, 2020, 12% of diagnosed cases required hospitalization. 18% of cases requiring hospitalization were patients 45–54 years, and 20% were patients 20–44 years. Mortality ranged from 10%–27% in patients aged ≥85 years to <1% in patients aged 20–54 years.[61] In Washington state, the first epicenter of America, between February 20, 2020, and March 5, 2020, Evergreen Hospital in Kirkland, WA treated 21 patients with COVID-19. Mechanical ventilation was initiated in 15 of the 21 patients (71%). Cardiomyopathy was observed in 7 patients (33%). As of March 17, 2020, mortality was 67% while another 24% remained critically ill, and 9.5% had been discharged from the ICU.[62]
Emerging data from China suggests that most cases (around 80%) are mild and do not require hospitalization. Individuals with severe disease have up to 28% in-hospital mortality.[63] For hospitalized patients, risk of death is increased with older age, higher Sequential Organ Failure Assessment (SOFA) score, and d-dimer greater than 1 μg/mL. Median duration of viral shedding was 20 days, and the longest observed duration of viral shedding in survivors was 37 days.[63]
Guidelines for Ophthalmologists and Staff
General guidelines
Several general points can be considered in addressing COVID-19 in ophthalmologic patient care[64]
- Minimize ambient noise so people do not need to speak loudly: turn off televisions/music; use fans which generate minimal noise.
- Restrooms: require people to wait several minutes after someone leaves the restroom before going in (to allow time for droplets to settle). Bathroom surfaces should be considered contaminated unless no one has used the restroom since it was disinfected. Consider restroom signage and possible monitoring.
- Any environment that is enclosed, with poor air circulation and high density of people, spells trouble. Being in an enclosed space, sharing the same air for a prolonged period, increases the chances of exposure and infection. Limit small enclosed work spaces to one (?) employee. Move diagnostic equipment currently in small rooms/alcoves to larger work spaces.
- Airflow -- people downwind of others are at higher risk: map airflow patterns to identify higher risk areas and curtail use of those areas as feasible; maximize ventilation -- open doors; open windows; maximize fan intensity/air flow with central air systems; use single pass (outside air) rather than recycled air in central air systems; increase ventilation of elevators if this is feasible.
- Fomite transfer (in addition to medical equipment) is in need of attention: countertops, cell phones, ID's, door handles, pens, clipboards, tissue dispensers, water coolers, elevator buttons etc.
- Social distancing guidelines don't hold in indoor spaces (with limited air exchange or recycled air and lots of people) where you spend a lot of time, as people on the opposite side of the room from a COVID-19 spreader can get infected. Social distancing rules are really to protect you with brief exposures.
Triage and Scheduling Staff
On March 18, 2020, the American Academy of Ophthalmology issued an advisory that all ophthalmologists to cease non-urgent eye care until further notice. On April 17, 2020, Dr. David Parke, recognizing the appropriate necessity of ramping up care, amended this advisory to state: "while the Academy made a national recommendation to curtail ophthalmic practice, the decisions to reopen more normal practice will be local and regional."
Ophthalmology Patient Triage
The following is meant as a guide to assist with decision making. Patients must be evaluated on a case-by-case basis.
| Ophthalmology Patient Triage | |||
|---|---|---|---|
| Specialty | High Risk (In person visit) | Telemedicine or Phone Visit (Note: all patients require telephonic triage before telemedicine consultation) | Low risk (Rebook in 3-6 months) |
| Contact Lens | |||
| New | None | None | Can be delayed |
| Follow-up | Pain, redness, photophobia (needs risk assessment) | Delays acceptable in other patients | |
| Cornea and Cataract | |||
| New | Patient by patient triage but likely delayed | Patient by patient triage but likely delayed | all routine, dry eye |
| Follow-up |
|
|
|
| Surgery | Urgent cases/perforations | Cataract | |
| General Ophthalmology | |||
| New |
|
Eye pain, discomfort |
|
| Follow-up | Phone/video consultation as necessary | Postponement or discharge from phone/video triage | |
| Genetics | |||
| New | All patients | ||
| Follow-up | All patients unless exceptional circumstances | ||
| Glaucoma | |||
| New |
|
Patient by patient triage of new referrals needed | |
| Follow-up |
|
|
|
| Surgery |
|
| |
| Ocular Oncology | |||
| New | All new referrals but with enhanced triage by team | ||
| Follow-up | Patients on less than 12 month follow-up interval | Patients on greater 12 month follow-up interval | Patients with no issues on video/telephone triage could be delayed further |
| Surgery | Expected to continue unless extenuating circumstances | ||
| Oculoplastics | |||
| New |
|
|
|
| Follow-up |
|
|
|
| Surgery | Tumor cases or orbital conditions with visual loss | Most other surgery could be postponed | |
| Pediatrics and Strabismus | |||
| New |
|
Case by case basis for failed vision screen age 5 or less |
|
| Follow-up |
|
|
Patient by patient triage by attending |
| Surgery | Cataract, glaucoma, dacryocele, severe ptosis in baby | ||
| Retina | |||
| New | Referral for RD, tear, CNVM, CRVO, Retinopathy noted on Diabetic screening, community optometry, A&E |
| |
| Follow-up |
|
|
|
| Surgery | New Detachments, monocular hemorrhage in good eye, endophthalmitis, ruptured globe, uncontrolled IOP, acute subfoveal hemorrhage, dislocated lens with inflammation and elevated IOP | ERM, macular hole, VMT with no change, lens dislocations | |
| Neuro-Ophthalmology | |||
| New | Patient by patient triage needed | Neuromuscular disorders | |
| Follow-up | Patient by patient triage needed | Neuromuscular disorders | Stable followup on a patient by patient basis |
| Uveitis | |||
| New |
|
Unlikely to be helpful in new uveitis patients | Anterior uveitis in A&E could be given an 8-10 week tapering course of drops then review in 3 months |
| Follow-up | Reviewed on a patient by patient basis but potentially 1/3 of patients may have to continue to attend |
|
|
| Surgery | Cataract surgery for uveitis patients could be delayed | ||
Registration Staff
- Reschedule outpatient visits, follow-ups or procedures that are not urgent should be postponed (as above).
- For urgent cases, these questions should be asked before any patient or visitor enters the building or waiting room:
- Presence of fever or respiratory symptoms: cough, sputum production, hemoptysis, sore throat, headache, fatigue, myalgia.
- Travel history or exposure to somebody who traveled to the high-risk areas (China, South Korea, Iran, Italy, Washington, New York or California) in the past 14 days.
- If a patient answers yes to either of the above questions, they should be sent home and encouraged to speak to their primary care provider
- If symptoms are severe, they should be sent to the Emergency Department of a hospital capable of handling COVID-19.
- Waiting room should be as empty as possible, and patients should be encourage to sit at least 6 ft from each other.
All Clinical Staff
- Registration clerks are to wear procedural masks.
- Wash your hands before and after each patient. When cleaning your hands with soap and water, wet your hands first with water, apply the amount of product recommended by the manufacturer to your hands, and rub your hands together vigorously for at least 20 seconds, covering all surfaces of the hands and fingers. Rinse your hands with water and use disposable towels to dry.
- Use a towel to turn off the faucet. Avoid using hot water, to prevent drying of skin.
Technicians and Optometrists
- Technicians assess each patient by taking a history, measuring spectacles, recording vision, and refracting.
- Gloves are recommended for all technicians and providers.
- Technicians should not perform slit lamp exams.
- Lanes need to be cleaned after each patient. Scrub of room should include faucets.
- Phoropters should be cleaned before and after each use and covered when not being used.
All Ophthalmologists
- Be on alert for patients who present with conjunctivitis, especially with flu-like symptoms (fever, cough, sore throat, runny or stuffy nose, head congestion, headache, nausea, shortness of breath, fatigue). Please alert the nursing staff if you identify such a patient.
- All patients with conjunctivitis are to be considered at risk for COVID-19.
- One visitor is allowed to accompany each patient to an appointment, unless an aide or assistant is required.
- All patient movement through the practice should be as limited as possible.
- Hand-sanitize frequently.
Consultation and examination
Rapid Treat and Release
- Rapid Treat and Release is the expeditious performance, with minimal use of instrumentation, of the minimally necessary medically appropriate evaluation and treatment in order to
- minimize the risk of COVID-19 transmission by reducing waiting room time, reducing provider contact time with patient, and minimizing use of instrumentation, and
- conserve resources.
- Rapid Treat and Release should be considered in areas with incidence of COVID-19 infection.
Rapid Treat and Release general principles
- Some conditions (e.g., non-traumatic subconjunctival hemorrhage, chalazion) may not require slit-lamp examination.
- Do not dilate all patients. If chief complaint is anterior or exterior, only examine the anterior segment.
- Use the Tonopen or a disposable tip on Goldmann tonometer for taking pressures.
- Save retinal exams and accessory lens use for patients who really need it, i.e., if something is not explained by anterior segment findings.
- Residents, technicians, nurses, and physician assistants should have lower threshold for asking supervising physicians when they are not sure if a patient should be rescheduled for later.
- Defer routine visits, especially for more vulnerable patients with pre-existing conditions at this time.
- All should have a low threshold for wearing gloves and procedure mask. Reuse masks until soiled or damaged in order to conserve supplies.
External Ocular Disease Rapid Treat and Release
- Rapid Treat and Release is especially suited to complaints related to external ocular irritation. These complaints include:
- Itching
- Burning
- Foreign body sensation/scratchiness
- Dryness
- Tearing
- Crusting
- Fluctuating blur
- Lid tenderness/swelling
- Non-traumatic subconjunctival hemorrhage
- The following conditions must be ruled out either by history or examination:
- Conjunctivitis associated with COVID-19
- Herpes simplex infection
- Varicella zoster infection
- Iritis
- Keratitis
- Acute angle closure glaucoma
- Cellulitis
- Deeper processes (orbital inflammation, temporal arteritis)
- Complaints/conditions that are less amenable to Rapid Treat and Release and require more in depth evaluation
- New onset flashes and floaters
- Retinal tear or detachment
- Uveitis
- PVD
- Painless acute vision loss
- Venous occlusion
- Arterial occlusion
- Retinal detachment
- Uveitis
- Central serous retinopathy
- Macular degeneration/CNV/hemorrhage
- Vitreous hemorrhage
- Optic neuritis/neuropathy
- Painful vision loss
- Corneal ulcer
- Foreign body
- Glaucoma
- Uveitis
- Tumor
- Trauma
- Scleritis
- Optic neuritis
- Chronic eye disease requiring frequent monitoring/treatment
- Proliferative diabetic retinopathy
- Diabetes with significant macular edema
- Vein occlusion with macular edema
- Macular degeneration with CNV
- Glaucoma with poor disease control
- Pediatric amblyopia monitoring
- Acute onset diplopia
- Ischemia
- Neurological disease
- Stroke
- Tumor
- Muscle entrapment
- Muscle paralysis
- Postop patients
- Those in the immediate postoperative period
- Those with concern for elevated IOP, retinal detachment, inflammation, rejection, etc)
- Ocular trauma
- Possible cornea or conjunctival abrasion or laceration
- Possible cornea or conjunctival foreign body
- Any blunt trauma to the globe
- Contact lens wearer with redness, pain, or visual symptoms
- New onset flashes and floaters
Tele-Ophthalmology
Using telemedicine for remote consultations or appointment alternatives can help curb the COVID-19 outbreak by serving as an effective triage mechanism, decreasing patient travel and limiting provider exposure. In some cases, telehealth information may be sufficient to make treatment recommendations. In many cases, telemedicine may not allow necessary elements of an evaluation such that providers should direct a patient to the appropriate location and specialist within a suitable timeframe and plan appropriate infection control measures. Telemedicine consultations may be directly between the ophthalmologist and the patient, or between the ophthalmologist and a consulting provider in a primary care office, emergency center, nursing home, or inpatient hospital setting. Telemedicine options include the patient uploading digital photos of their eye to their patient portal in the EMR or videoconferencing with live interaction.
Common ophthalmic issues that have the potential to be managed remotely include:
- Itching
- Burning
- Foreign body sensation/scratchiness
- Dryness
- Tearing
- Crusting
- Fluctuating, blurred vision
- Lid tenderness/swelling/chalazion/preseptal cellulitis
- Subconjunctival hemorrhage
- Follow-up on oculoplastics procedures with routine healing
Fundus photos, MRI and CT imaging can also be shared for decision making
For practices that do not currently have a direct-to-patient telemedicine program, WebEx or Zoom are two commonly used video conference systems that are HIPAA compliant. Numerous other compliant telemedicine platforms are available, such as VSee, EyecareLive, and Chiron. The office would schedule the virtual visit as normal and send the video conference link via email to both the provider and patient for the appointment time. To help with the COVID-19 outbreak many platforms are discounting subscription fees.
Additionally, mobile versions of Epic (Haiku and Canto) can be used for inpatient rounding while Vidyo can be used to connect with inpatients who are in isolation/quarantine.
Because commercial payers do not consistently reimburse for telemedicine services, the practice will need to decide how to bill patients for these telemedicine services. If it is decided to bill, the office should communicate the maximum out of pocket cost to patients before scheduling. Visits can be scheduled for a preset duration (i.e. $X for 15 minutes).
In response to the COVID-19 outbreak, on March 6, 2020, Congress has waived or modified requirements for reimbursement for telehealth services within any identified emergency area during the current emergency period with the Coronavirus Preparedness and Response Supplemental Appropriations Act.[65] This will allow physicians to bill Medical and Medicaid. Specific new time-based service codes have been created: 99421, 99422 , 99423.
For all patients with conjunctivitis
- Once a patient is identified by any staff member as having conjunctivitis, the patient should wear a procedural mask.
- All staff interacting with a conjunctivitis patient should wear a procedural mask and eye protection.
- The conjunctivitis patient should be screened for COVID-19.
For patients with conjunctivitis who screen positive for COVID-19
- Follow the Instruction for handling suspected COVID-19
- If ophthalmic evaluation is necessary, please follow the guidelines that follow.
For patients with conjunctivitis who screen negative for COVID-19 infection
- The patient should wear a procedural mask.
- All staff interacting with the patient should wear a procedural mask and eye protection.
- Isolate the patient in an examination room immediately.
- The examining physician should wear a procedural mask.
- The physician will use his/her best medical judgement in evaluating and treating the patient, including deciding if slit lamp examination is appropriate and necessary.
- If during or after evaluating the patient, the designated physician has a strong suspicion of COVID-19, follow standard COVID-19 protocol.
For all patients who screen positive for possible COVID-19 or who have tested positive for COVID-19 (COVID-19 patients) who require ophthalmic evaluation
If in the unlikely event that an ophthalmology consultation on a COVID-19 patient is requested, the ophthalmologist responsible for handling the consultation should ask the following questions of the requesting physician to ascertain if ophthalmology consultation is medically necessary:
- Did the patient have any recent ocular procedure/surgery? (we don't want to miss the rare event of endophthalmitis)
- Has patient vision changed?
- Does the patient have photophobia (light sensitivity)?
- Is the patient a contact lens wearer, and, if so, is the patient wearing contact lenses?
- Did the patient have recent ophthalmic trauma (including any risk of a cornea/conjunctiva foreign body)?
- Is the patient complaining of double vision?
The ophthalmologist responsible for handling the consultation request then makes recommendations to the requesting physician regarding management of the patient. The ophthalmologist will follow standard consultation policy and will perform a consultation if, after discussion with the requesting physician, the requesting physician still requests a consultation.
For examination of COVID-19 patients, follow the CDC Interim guidelines (referenced below) with the following amendments and clarifications
- For ophthalmologic evaluations not necessitating slit lamp or direct ophthalmoscopy examination, standard CDC-recommended personal protective (facemask, eye shield/goggles, gowns and gloves) equipment is mandatory. Shoe covers (not addressed in CDC recommendations) are mandatory.
- N95 respirators and eye shields, along with all other recommended personal protective equipment (listed above) are to be worn for:
- Portable or standard slit lamp evaluation (this extremely close contact examination is not addressed in CDC guidelines),
- Direct ophthalmoscopy (this extremely close contact examination is not addressed in CDC guidelines), which should only be performed if slit lamp 78 or 90 diopter fundoscopy or funduscopic imaging is unavailable, and
- All ophthalmic procedures, including injections, laser surgery, and incisional surgery
As per CDC guidelines, only designated equipment should be used when caring for patients with known or suspected COVID-19. If dedicated equipment is unavailable, all equipment used in the evaluation of a COVID-19 patient is to undergo disinfection (please see above for cleaning protocol)
Diagnostic Procedures
Non-essential imaging/testing should be deferred, and equipment use should be kept at a minimum.
- Tonometry: Intraocular pressure will be checked using a Tonopen with a disposable tip. If Goldmann tonometry is needed, a disposable tip should be considered. If a reusable tip is used, it must be free of defects (cracks, scratches, etc.) and disinfected as per manufacturers recommendations.
- Gonioscopy: Should only be performed with a strong medical indication. If performed, a disposable gonioprism should be used. If a disposable gonioprism is not available, the reusable gonioprism should undergo high level disinfection.
- Ultrasound Pachymetry: Should not be performed.
- Direct ophthalmoscopy: Should only be performed if there is a strong medical indication. High magnification fundoscopy should be performed with 90 or 78 diopter lenses at the slit lamp.
- Slit Lamp: Should be used with commercially available slit-lamp barriers or breath shield.
- Humphrey Visual Fields: The need for visual field testing should be determined for each patient by his/her doctor. Our goal is to use perimetry for those patients at high risk for progression, surgical decision-making, and new patients. Routine perimetry should be deferred to the next visit if possible. Detailed cleaning guidance for the Humphrey Visual Field Analyzer are available: [66]
- Optical Coherence Tomography (OCT): The need for imaging testing should be determined for each patient by his/her doctor. Our goal is to use imaging for those patients at high risk for progression, surgical decision-making, and new patients. Routine imaging should be deferred to the next visit if possible.
Therapeutic procedures requiring contact lenses
- Ophthalmic laser treatments should be kept to a minimum. Elective lasers (e.g., for posterior capsulotomy in a patient with adequate visual function) should be deferred.
- Ophthalmic lasers that cannot be deferred should be performed with single use disposable laser lenses. If a single-use lens is not available, the reusable lens should undergo high level disinfection.
Cleaning protocols
- Front desk workstations and waiting room furniture should be cleaned hourly with an EPA recommended disinfectant. Additional cleans should be done after patients who present with conjunctivitis or with flu-like symptoms.
- All imaging equipment should be cleaned before and after each patient, using the technique recommended by each manufacturer.
- Rooms and instruments should be thoroughly disinfected after each patient encounter. Wear disposable gloves when cleaning and disinfecting surfaces. Slit lamps, including controls and accompanying breath shields, should be disinfected, particularly wherever patients put their hands and face. The current CDC recommendations for disinfectants specific to COVID-19 include:
- Diluted household bleach (5 tablespoons bleach per gallon of water)
- Alcohol solutions with at least 70% alcohol.
- Common EPA-registered household disinfectants currently recommended for use against SARS-CoV-2 include Clorox brand products (e.g., disinfecting wipes, multi-surface cleaner + bleach, clean up cleaner + bleach), Lysol brand products (e.g., professional disinfectant spray, clean and fresh multi-surface cleaner, disinfectant max cover mist), Purell professional surface disinfectant wipes and more. The EPA offers a full list of antimicrobial products expected to be effective against COVID-19 based on data for similar viruses.
Surgical Procedures
In order to prevent unnecessary exposure to asymptomatic patients with COVID-19, as well as to conserve the limited supply of masks, face shields, and other protective equipment, the CDC recommends the cancellation and reduction of all elective surgeries, particularly in Seattle (Washington), Santa Clara (California), New Rochelle (New York), Florida, and Massachusetts as of March 14, 2020.
Getting back to business
It is anticipated that locally, viral illnesses will peak and abate (perhaps waxing and waning). This will allow a step wise opening of society, as detailed in the leaked draft of shelved CDC Guidance, [67] and return to ophthalmologic practice, depending on local conditions. A relative surge in requests for care by patients with ophthalmic issues can be anticipated when patients are no longer afraid to leave their homes to see a physician. There will be a backlog of previously scheduled but cancelled patients. At the same time, there may be constraints on the number of patients that can bee seen in the office and on the availability of operating rooms. The American Academy of Ophthalmology frequently updates information on returning to practice. [68]
Establishing a safe environment and reassuring your patients
Patients will be appropriately wary or entering any public space if they do not perceive that it is safe. The establishment of a relatively safe environment is multifaceted, including:
- Strict instrument and environmental disinfection protocols,
- Optimization of patient flow, isolation/separation of patients from other patients, and COVID-19 symptom testing (e.g. temperature checks and questionnaires),
- Recognition that lack of symptoms and negative PCR testing are merely a suggestion, not a guarantee, that an individual is not infected with COVID-19,
- Minimizing physical contact by staff with patients by incorporation of telemedicine for patient interview/history/assessment and plan,
- COVID-19 antibody testing for staff,
- Physical reconfiguration of office to achieve the above, and
- A carefully thought out patient schedule, including ramping up volume and prioritizing patient visits by urgency (see below).
Office visits
Review patient charts, especially those with appointments that were cancelled during the pandemic, and triage visits along the lines adopted by Columbia Doctors Ophthalmology (courtesy of Ms. Bonnie Wang, Mr. Daniel Trese, and Dr. George A. Cioffi):
Urgent = Patient needs to be seen in the office
Priority level A = Patient should be seen May 15th - June 30th
Priority level B = Patient should be seen July 1st - August 31st
Priority level C = Patient can be seen after September 1st
Video Visit = Patient should be scheduled for a video visit
Telephone Call = Provider will call patient
The process of triaging should begin well before easing of social distancing.
Surgical triaging
The American College of Surgeons issued general Guidance for Triage of Non-Emergent Surgical Procedures in response to the COVID-19 pandemic. [69] The American Academy of Ophthalmology prepared a "List of urgent and emergent ophthalmic procedures" [70] Both these guidance documents can be used to prepare a triage system such as the Cataract Surgery Triage Guidelines developed by Leejee Suh, MD and Jeffrey Liebmann, MD at Columbia University:
| Groups Description | Description | Rationale for surgery |
|---|---|---|
| Group A
Urgent/Emergency surgery |
1. Vision 20/200 or worse
2. Anisometropia causing diplopia/vertigo 3. Phacomorphic cataract with imminent angle closure 4. Cataract precludes examination of fundus 5. Combined cases driven by other medical needs (retinal, glaucoma, trauma) 6. Congenital cataract in amblyopic period 7. Cataract in monocular patient |
-Legal blindness
-High fall risk due to vision -Diplopia/vertigo caused by unequal refractive error -Risk of permanent vision loss from acute angle closure glaucoma -Inability to visualize fundus due to cataract -Cataract removal beneficial in conjunction with other surgery (ie. retina, cornea, glaucoma) -Reduce risk of irreversible amblyopia with congenital cataract removal -Inability to function with daily activities of living in a monocular patient due to cataract -Inability to perform daily activities of living due to vision |
| Group B | 1. Vision 20/50 to 20/150 (including by glare testing)
2. Concurrent pseudoexfoliation syndrome 3. Concurrent Fuchs dystrophy or risk for corneal decompensation |
-Inability to drive legally
-Fall risk due to vision -Inability to perform daily activities of living due to vision -Risk of zonular dehiscence and surgical complications with delay in surgery -Risk of need for further procedures including corneal transplantation with delay in surgery |
| Group C | 1. Vision 20/25 to 20/40 | -Inability to drive due to glare
-Inability to adequately perform daily activities of living -Inability to work due to impaired vision |
Additional Resources
- American Academy of Ophthalmology. Alert: Important coronavirus updates for ophthalmologists https://www.aao.org/headline/alert-important-coronavirus-context San Francisco: American Academy of Ophthalmology, 2020. Accessed March 09, 2020.
- Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html. Accessed March 14, 2020.
- Lai, Tracy H.T., Tang, Emily W.H., Chau, Sandy K.Y., Fung, Kitty S.C., Li, Kenneth K.W. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefe's Archive for Clinical and Experimental Ophthalmology. 2020.
References
- ↑ Naming the coronavirus disease (COVID-19) and the virus that causes it. World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. Accessed March 15, 2020.
- ↑ WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. World Health Organization. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed March 15, 2020.
- ↑ Cyranoski D. Profile of a killer: the complex biology powering the coronavirus pandemic. nature https://www.nature.com/articles/d41586-020-01315-7. Accessed May 10, 2020
- ↑ Bloomberg News. Europe’s Doctors Repeat Errors Made in Wuhan, China Medics Say Bloomberg https://www.bloomberg.com/news/articles/2020-03-17/europe-s-doctors-getting-sick-like-in-wuhan-chinese-doctors-say Accessed March 17, 2020.
- ↑ American Academy of Ophthalmology. In Memoriam: Ophthalmologist Deaths From COVID-19 https://www.aao.org/coronavirus/deaths Accessed May 9, 2020.
- ↑ Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). World Health Organization. 2020.
- ↑ Mehta P, Sattui S, van der Geest K, Brouwer E, Conway R, Putman M, Robinson P, Mackie S. Giant cell arteritis and COVID-19: similarities and discriminators, a systematic literature review. The Journal of Rheumatology Oct 2020, jrheum.200766; DOI: 10.3899/jrheum.200766.
- ↑ 8.0 8.1 Cascella M, Rajnik M, Cuomo A, et al. Features, evaluation and treatment of coronavirus (COVID-19). NCBI Bookshelf. StatPearls Publishing: Treasure Island. 2020.
- ↑ Guo Y, Cao Q, Hong Z. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Military Medical Research. 2020;7(11).
- ↑ Hampton T. Bats may be SARS reservoir. JAMA. 2005;294(18):2291.
- ↑ Banerjee A, Kulcsar K, Misra V, Frieman M, Mossman K. Bats and coronaviruses. Viruses. 2019;11(1):E41.
- ↑ Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, et al. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310(5748):676–9.
- ↑ Chowell G, Abdirizak F, Lee S, Lee J, Jung E, Nishiura H, et al. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210
- ↑ Kang CK, Song KH, Choe PG, Park WB, Bang JH, Kim ES, et al. Clinical and epidemiologic characteristics of spreaders of middle east respiratory syndrome coronavirus during the 2015 outbreak in Korea. J Korean Med Sci. 2017;32(5):744–9.
- ↑ Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020.
- ↑ Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020,195(10229):1054-1062.
- ↑ Hui KPY, e. el. Tropism, replication competence, and innate immune responses of the coronavirus SARS-CoV-2 in human respiratory tract and conjunctiva: an analysis in ex-vivo and in-vitro cultures. Lancet Respiratory Med, published on line May 7, 2020. https://doi.org/10.1016/S2213-2600(20)30193-4. Accessed May 8, 2020
- ↑ Lei J, Kusov Y, Hilgenfeld R. Nsp3 of coronaviruses: Structures and functions of a large multi-domain protein. Antiviral Res. 2018 Jan;149:58-74.
- ↑ Perlman S, Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat. Rev. Microbiol. 2009 Jun;7(6):439-50.
- ↑ Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020.
- ↑ Cohn A, MBaeyi S. What Clinicians Need to Know About the Pfizer-BioNTech COVID-19 Vaccine. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/covid-19/downloads/pfizer-biontech-vaccine-what-Clinicians-need-to-know.pdf. Accessed on December 14, 2020.
- ↑ Pfizer and BioNTech conclude phase 3 study of covid-19 vaccine candidate, meeting all primary efficacy endpoints. Pfizer. https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-conclude-phase-3-study-covid-19-vaccine. Accessed on December 14, 2020.
- ↑ Moderna announces primary efficacy analysis in Phase 3 COVE Study for its COVID-19 vaccine candidate and filling today with U.S. FDA for emergency use authorization. MODERNA https//investors.moderna.com/news-release-details/moderna-announces-primary-efficacy-analysis-phase-3-cove-study. Accessed December 21, 2020.
- ↑ 24.0 24.1 Wu P, Duan F, Luo C, et al. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138(5):575–578. doi:10.1001/jamaophthalmol.2020.1291
- ↑ Zhou Y et al. Ocular findings and proportion with conjunctival SARS-COV-2 in COVID-19 patients. Ophthalmology , in press. https://doi.org/10.1016/j.ophtha.2020.04.028. Accessed May 19, 2020.
- ↑ Méndez Mangana, Carlos et al. “Episcleritis as an ocular manifestation in a patient with COVID-19.” Acta ophthalmologica vol. 98,8 (2020): e1056-e1057. doi:10.1111/aos.14484.
- ↑ 27.0 27.1 François J, Collery AS, Hayek G, et al. Coronavirus Disease 2019–Associated Ocular Neuropathy With Panuveitis: A Case Report. JAMA Ophthalmol. 2021;139(2):247–249.
- ↑ Romero-Sánchez C.M. Neurologic manifestations in hospitalized patients with COVID-19. Neurology. 2020;95(8):e1060.
- ↑ de Ruijter N.S., Kramer G., Gons R.A.R., Hengstman G.J.D. Neuromyelitis optica spectrum disorder after presumed coronavirus (COVID-19) infection: a case report. Mult. Scler. Relat. Disord. 2020;46:102474.
- ↑ Zhou S., Jones-Lopez E.C., Soneji D.J., Azevedo C.J., Patel V.R. Myelin oligodendrocyte glycoprotein antibody-associated optic neuritis and myelitis in COVID-19. J. Neuroophthalmol. 2020;40(3):398–402.
- ↑ Novi G. Acute disseminated encephalomyelitis after SARS-CoV-2 infection," (in eng) Neurol. Neuroimmunol. Neuroinflamm. 2020;7(5):e797.
- ↑ Sawalha K, Adeodokun S, Kamoga GR. COVID-19-Induced Acute Bilateral Optic Neuritis. J Investig Med High Impact Case Rep. 2020 Jan-Dec;8:2324709620976018.
- ↑ Silva, Marcus Tulius T et al. “Isolated intracranial hypertension associated with COVID-19.” Cephalalgia : an international journal of headache vol. 40,13 (2020): 1452-1458.
- ↑ Ramesh SV, Ramesh PV, Ramesh MK, Padmanabhan V, Rajasekaran R. COVID-19-associated papilledema secondary to cerebral venous thrombosis in a young patient. Indian J Ophthalmol. 2021 Mar;69(3):770-772.
- ↑ Belghmaidi, Sarah et al. “Third Cranial Nerve Palsy Presenting with Unilateral Diplopia and Strabismus in a 24-Year-Old Woman with COVID-19.” The American journal of case reports vol. 21 e925897. 15 Oct. 2020, doi:10.12659/AJCR.925897.
- ↑ Ordás, Carlos M et al. “Concurrent tonic pupil and trochlear nerve palsy in COVID-19.” Journal of neurovirology vol. 26,6 (2020): 970-972. doi:10.1007/s13365-020-00909-1.
- ↑ Greer C., Bhatt J.M., Oliveira C.A., Dinkin M.J. Isolated Cranial Nerve 6 Palsy in 6 patients with COVID-19 infection. J. Neuroophthalmol. 2020;40(4):520–522.
- ↑ 38.0 38.1 Belghmaidi, Sarah et al. “Third Cranial Nerve Palsy Presenting with Unilateral Diplopia and Strabismus in a 24-Year-Old Woman with COVID-19.” The American journal of case reports vol. 21 e925897. 15 Oct. 2020, doi:10.12659/AJCR.925897.
- ↑ Acharya S, Diamond M, Anwar S, Glaser A, Tyagi P. Unique case of central retinal artery occlusion secondary to COVID-19 disease. IDCases. 2020;21:e00867.
- ↑ Montesel A, Bucolo C, Mouvet V, Moret E, Eandi CM. Case Report: Central Retinal Artery Occlusion in a COVID-19 Patient. Front Pharmacol. 2020 Dec 23;11:588384. doi: 10.3389/fphar.2020.588384. PMID: 33424598; PMCID: PMC7785811.
- ↑ Yahalomi T, Pikkel J, Arnon R, Pessach Y. Central retinal vein occlusion in a young healthy COVID-19 patient: a case report. Am J Ophthalmol Case Rep. 2020;20:100992.
- ↑ Gaba WH, Ahmed D, Al Nuaimi RK, Dhanhani AA, Eatamadi H. Bilateral Central Retinal Vein Occlusion in a 40-Year-Old Man with Severe Coronavirus Disease 2019 (COVID-19) Pneumonia. Am J Case Rep. 2020;21:e927691.
- ↑ Ray A. Miller Fisher syndrome and COVID-19: is there a link?. BMJ Case Rep. 2020;13(8):e236419. Published 2020 Aug 11. doi:10.1136/bcr-2020-236419
- ↑ 44.0 44.1 Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92(6):589-594. doi:10.1002/jmv.25725
- ↑ U.S. Food and Drug Administration (FDA). Emergency Use Authorizations. FDA https://www.fda.gov/medical-devices/emergency-situations-medical-devices/emergency-use-authorizations#coronavirus2019. Accessed May 9, 2020.
- ↑ U.S. Food and Drug Administration (FDA). EUA Authorized Serology Test Performance. FDA https://www.fda.gov/medical-devices/emergency-situations-medical-devices/eua-authorized-serology-test-performance, Accessed May 9, 2020.
- ↑ Dearen J, Stobbe M. Associated Press. Trump administration buries detailed CDC advice on reopening. Yahoo News https://news.yahoo.com/ap-exclusive-admin-shelves-cdc-041502978.html. Accessed May 9, 2020.
- ↑ National Institutes of Health. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health https://covid19treatmentguidelines.nih.gov/, Accessed May 10, 2020.
- ↑ Hung IF-N, et al. Triple combination of interferon beta-1b, lopinavir–ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Published on line May 8, 2020. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31042-4/fulltext. Accessed May 10, 2020.
- ↑ NIH clinical trial shows Remdesivir accelerates recovery from advanced COVID-19. https://www.nih.gov/news-events/news-releases/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19, Published on line April 29, 2020. Accessed May 10, 2020.
- ↑ Wang Y, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31022-9/fulltext. Published on line April 29, 2020. Accessed May 10, 2020.
- ↑ Massachusetts General Hospital. The Massachusetts General Hospital. COVID-19 Treatment Guide. Massachusetts General Hospital. https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/mass-general-COVID-19-treatment-guidance.pdf, accessed 5/10/2020.
- ↑ National Institutes of Health. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health https://covid19treatmentguidelines.nih.gov/whats-new/. Accessed May 26, 2020.
- ↑ Massachusetts General Hospital. The Massachusetts General Hospital. COVID-19 Treatment Guide. Massachusetts General Hospital. https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/mass-general-COVID-19-treatment-guidance.pdf, accessed 5/10/2020.
- ↑ Magagnoli J, et al. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19. https://www.medrxiv.org/content/10.1101/2020.04.16.20065920v1.article-info. Accessed 4/22/2020
- ↑ Geleris, J. et al. Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19. https://www.nejm.org/doi/full/10.1056/NEJMoa2012410, accessed May 8, 2020
- ↑ Rosenberg, ES , et al. Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State https://jamanetwork.com/journals/jama/fullarticle/2766117?guestAccessKey=81833699-7750-4082-8270-331dc4809144&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=05112. Published on line May 11, 2020. Accessed May 12, 2020.
- ↑ Massachusetts General Hospital. The Massachusetts General Hospital COVID-19 Treatment Guide. Massachusetts General Hospital. https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/mass-general-COVID-19-treatment-guidance.pdf, accessed 4/22/2020.
- ↑ Boulware D. et al. University of Minnesota. Post-exposure Prophylaxis / Preemptive Therapy for SARS-Coronavirus-2 (COVID-19 PEP). U.S. National Library of Medicine clinicaltrials.gov. https://www.clinicaltrials.gov/ct2/show/NCT04308668, accessed 4/22/2020.
- ↑ Kampf G, et al. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hospital Infection2020;104: 246-251
- ↑ Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. ePub: 18 March 2020. DOI: http://dx.doi.org/10.15585/mmwr.mm6912e2
- ↑ Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. March 19, 2020.
- ↑ 63.0 63.1 Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID-19. The Lancet. March 2020. doi:10.1016/s0140-6736(20)30633-4
- ↑ Bromage E. The Risks - Know Them - Avoid Them. Erin Bromage PhD: Disease musings. https://erinbromage.wixsite.com/covid19/post/the-risks-know-them-avoid-them. Accessed May 9, 2020
- ↑ Coronavirus Preparedness and. Response Supplemental Appropriations Act. https://www.congress.gov/116/bills/hr6074/BILLS-116hr6074enr.pdf. Congress. 2020
- ↑ Carl Zeiss Meditec AG. MED Support - Now Disinfecting ophthalmic devices. ZEISS International, optical and optoelectronic technology https://www.zeiss.com/meditec/int/med-support-now/disinfecting-ophthalmic-devices.html#faq Accessed May 26, 2020.
- ↑ AP Staff, Associated Press. Guidance for Opening Up America Again Framework. DocumentCloud. https://www.documentcloud.org/documents/6889330-Guidance-for-Opening-Up-America-Again-Framework.html, Accessed May 13, 2020.
- ↑ American Academy of Ophthalmology. Alert: Important coronavirus updates for ophthalmologists. American Academy of Ophthalmology https://www.aao.org/headline/alert-important-coronavirus-context. Last updated May 6, 2020. Accessed May 10, 2020.
- ↑ American College of Surgeons. COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. American College of Surgeons. https://www.facs.org/covid-19/clinical-guidance/triage. Dated March 17, 2020. Accessed May 10, 2020.
- ↑ American Academy of Ophthalmology. List of urgent and emergent ophthalmic procedures https://www.aao.org/headline/list-of-urgent-emergent-ophthalmic-procedures March 27, 2020. Accessed May 10, 2020.

