Panuveitis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Definition
Panuveitis, also known as Diffuse uveitis, is the inflammation of all uveal components of the eye with no particular site of predominant inflammation.
Anatomy/Physiology
The uvea is a highly vascular layer that lines the sclera, and its principal function is to provide nutrition to the eye. The iris is responsible for the metabolism of the anterior segment by diffusion of metabolites through the aqueous. The ciliary body secretes aqueous which bathes the avascular structures of the anterior segment. The choroid provides nourishment for the outer layers of the retina. Although topographically separate, the iris, ciliary body, and choroid are closely related forming a continuous whole and diseases affecting one portion often affect the other regions as seen in panuveitis. [2]
Classification of Uveitis
The Standardization of Uveitis Nomenclature (SUN) Working group guidance on uveitis terminology categorizes uveitis anatomically as follows;
- Anterior uveitis; localized primarily to the anterior segment of the eye, involving iris and pars plicata.
- Intermediate uveitis; localized to the vitreous cavity and pars plana
- Posterior uveitis; localized to the choroid and retina.
- Panuveitis; inflammation involving anterior, intermediate and posterior uveal structures.[3]
Etiopathogenesis
Inflammatory causes
- Exogenous infections: due to the introduction of organisms into the eye through perforating wound or ulcer.
- Secondary infections: the inflammation of the uveal tract due to its spread from other ocular tissues- cornea, sclera or retina.
- Endogenous infections: organisms primarily lodged in another organ of the body reach the eye through the bloodstream. These include bacterial infections such as syphilis, tuberculosis; viral infections such as mumps, smallpox or influenza; and protozoal infections such as toxoplasmosis.
- Immune-related inflammation: sensitized ocular tissues excite an immune response on contact with the organisms such as in Behcet syndrome.
Neoplastic causes
Some intraocular malignancies such as retinoblastoma, iris melanoma, and systemic haematological malignancies such as leukemia, lymphoma and histiocytic cell sarcoma can present with features of panuveitis termed ‘masquerade syndromes’.
Traumatic causes
Blunt or penetrating ocular trauma can produce features of panuveitis. Surgical trauma from intraocular procedures such as cataract extraction, trabeculectomy, and vitreoretinal surgery can produce postoperative panuveitis.[2]
Clinical presentation
The clinical presentation of panuveitis involves the summation of symptoms and signs of anterior, intermediate, and posterior uveitis.
Symptoms
- Pain
- Photophobia
- Redness
- Watery discharge
- Blurring of vision
- Floaters
- Diminution of vision
- Flashes of light
Signs
- Reduced Visual acuity
- Lid Oedema
- Ciliary injection
- Chemosis
- Keratic Precipitates(KPs)- deposits on the corneal endothelium composed of inflammatory cells such as lymphocytes, plasma cells, and macrophages.
Anterior chamber
- Cells in the anterior chamber
- Hypopyon–whitish purulent exudate composed of myriad inflammatory cells in the inferior part of the anterior chamber forming a horizontal level under the influence of gravity.
- Aqueous flare: haziness of the normally clear fluid in the anterior chamber due to protein in the aqueous present as a result of the breakdown of the blood-aqueous barrier.
- Fibrinous exudates
Iris
- Iris nodules- including Koeppe nodules which are the site of posterior synechiae formation, Bussaca nodules which are a feature of granulomatous uveitis, and yellowish nodules seen in syphilitic uveitis.
- Iris pearls- seen in lepromatous uveitis
- Iris crystals
- Posterior synechiae
- Iris atrophy- seen in herpetic uveitis
- Heterochromia iridis
- Iris neovascularization
Other signs
- Intraocular pressure may be increased or reduced
- White snowball like exudates near the ora serrata
- Mild peripheral phlebitis
- Macular edema
- Papillitis or Disc edema
- Vitreous hemorrhage
- Vitritis
- Exudates in the choroid and retina
- Retinal hemorrhages
- Choroidal Neovascularization
- Retinal detachment[4]
Systemic Associations
Toxoplasmosis
Toxoplasmosis is caused by Toxoplasma gondii, an obligate intracellular protozoan. It is the most common cause of infectious retinitis in immunocompetent individuals and commonly occurs due to reactivation of prenatal infestation, but postnatal infestation may also occur. Reactivation commonly occurs between 10-35 years. Ocular findings include:
- Retinitis, retinochoroiditis,
- Vitritis
- Papillitis, optic neuritis
- Vasculitis (arteritis, phlebitis)
- Deep retinal infiltrates
- Subretinal neovascularization
- Vitreous strands and membranes
- Detachment (PVD) posterior hyaloid face covered with inflammatory precipitates.
- Posterior synechiae
- Cataract
Tuberculous uveitis
Intraocular TB can be due to direct infection of Mycobacterium tuberculosis or indirect immune-mediated hypersensitivity response to mycobacterial antigens when there is no defined active systemic lesion elsewhere, or the lesion is thought to be inactive. Ocular findings include:
- Mutton-fat keratic precipitates and posterior synechiae
- Vitritis
- Macular edema, retinal vasculitis, neuroretinitis, solitary or multiple choroidal tubercles, multifocal choroiditis, choroidal granulomas, subretinal abscess
- Choroiditis
- Serous retinal detachment
- Anterior optic neuritis, neuroretinitis, retrobulbar optic neuritis, optochiasmatic arachnoiditis, optic nerve tuberculoma or papilledema
Vogt-Koyangi-Harada (VKH) Syndrome
VKH Syndrome is an idiopathic multisystem autoimmune disease featuring inflammation of melanocyte containing tissues such as the uvea, skin, ear, and meninges. It predominantly affects Hispanic, Japanese and pigmented individuals. The following criteria are required to make a diagnosis of VKH syndrome.[4]
- The absence of a history of penetrating ocular trauma
- Absence of other ocular disease entities
- Bilateral panuveitis
- Neurological and auditory manifestations
- Integumentary findings, not preceding the onset of central nervous system or ocular disease such as alopecia, poliosis, and vitiligo
Behcet disease
Behcet disease is an idiopathic multisystem syndrome characterized by recurrent aphthous oral ulcers, genital ulcerations, and panuveitis. It typically affects patients from Turkey, Middle, and the Far East, with a lower prevalence in Europe and North America. Relapsing/remitting acute onset panuveitis with retinal vasculitis and often spontaneous resolution without treatment is the classical pattern of eye involvement. Retinal vascular disease (vasculitis and occlusion) is the main cause of visual impairment.
Sarcoidosis
Sarcoidosis is a chronic disorder of unknown cause, manifesting with noncaseating granulomatous inflammatory foci. It is one of the most common systemic associations of panuveitis. It is more common in colder climates but affects people of black ethnicity more than whites. The International Workshop on Ocular Sarcoidosis (IWOS) identified seven key signs in the diagnosis of intraocular sarcoidosis.[4]
- Mutton fat KPs and/or small granulomatous KPs and/or iris nodules.
- Trabecular meshwork nodules and/or tent shaped Peripheral Anterior Synechiae (PAS)
- Vitreous opacities; snowballs and/or ‘strings of pearls’
- Multiple chorioretinal peripheral lesions
- Nodular and/or segmental periphlebitis (with/without candlewax drippings) and/or retinal macroaneurysm in an inflamed eye.
- Optic disc nodules/granulomas and/or solitary choroidal nodule.
- Bilaterality
Syphilis
Syphilis is a great mimic of panuveitis due to infection with Treponema pallidum.
The ocular findings include:
- Iridocyclitis
- Multifocal chorioretinitis
- Focal areas of chorioretinal atrophy associated with pigmentation
- Optic neuritis
- Optic atrophy
Sympathetic Ophthalmitis
Sympathetic Ophthalmitis is a bilateral granulomatous panuveitis occurring after penetrating trauma; it may also occur following intraocular surgery especially multiple vitreoretinal procedures. It occurs due to immune sensitization to melanin or melanin associated proteins in uveal tissues. The findings include:
- Koeppe nodules
- Mutton fat KPs
- Retinal edema
- Disc edema[5]
Investigations
A careful history and detailed clinical examination are usually sufficient in making a diagnosis. However, investigations may be necessary especially in recurrent and bilateral cases of panuveitis.
Blood tests
- FBC – Eosinophilia - parasitic infections such as Toxoplasmosis
- Lymphocytosis – Chronic infections
- Erythrocyte Sedimentation Rate – a non-specific indication of systemic disease.
- Antibody titre: Toxoplasmosis
- Angiotensin-converting enzyme: Sarcoidosis
Skin testing
- Tuberculin test- Tuberculosis
- Kveim test – Sarcoidosis
- Behcetin (pathergy) test– Behcet’s disease
HLA Testing
- Behcet’s disease: HLA-B51.
- Sympathetic Ophthalmia: HLA-A11.
- Vogt-Koyanagi-Harada disease: MT-3, BW22J/DR5, DW15.
Radiology
- Skull x-ray: Calcification in toxoplasmosis
- Chest x-ray: Tuberculosis, Sarcoidosis, Malignancies
- Gallium scans: Lungs, Salivary glands, Lacrimal glands for sarcoidosis.
- Ultrasound Scan
- CT scan: Chest CT in Sarcoidosis
Serology
Treatment
Non Specific Treatment
Cycloplegics
- Give comfort by relieving iris sphincter and ciliary muscle spasm,
- Prevent formation of posterior synechiae
- Break down synechiae
Corticosteroids
- Reduction of leukocytic and plasma exudation
- Maintenance of cellular membrane integrity with inhibition of tissue swelling
- Inhibition of phagocytosis and lysozymal release from granulocytes.
- Increased stabilization of intracellular lysosomal membranes.
- Suppression of circulating lymphocytes.
Systemic immunosuppressive agents
- Alkylating agents - Cyclophosphamide and Chlorambucil-These agents work by suppression of T – lymphocytes and to a lesser extent B – lymphocytes.
- Antimetabolites- Azathioprine (impairs purine metabolism inhibiting the synthesis of DNA, RNA and protein) and Methotrexate (impairs folate synthesis by inhibiting dihydrofolate reductase, an enzyme that participates in the synthesis of folic acid)
- T cell inhibitors - Cyclosporine A, Tacrolimus-Inhibits T-cell lymphocyte activation
Biological agents
- Infliximab, Adalimumab, Etanercept; Inhibit alphaTNF (Tumour Necrosis Factor)
Specific Treatment
Based on Underlying Disease.
- Syphilis: Penicillin. Penicillin-sensitive patients can be treated with oral Tetracycline or Erythromycin
- Tuberculosis: Standard antitubercular therapy (Isoniazid, Rifampicin, Ethambutol, Pyrazinamide)
- Toxoplasmosis: Clindamycin, Sulphadiazine, Pyrimethamine, Cotrimoxazole, Atovaquone, Azithromycin
Prognosis
Panuveitis is a major cause of blindness and visual morbidity. The prognosis for people with panuveitis varies depending on the underlying cause and severity. When the condition is unrecognized or inadequately treated, profound and irreversible vision loss can occur. Therefore early detection and proper management is a necessity in every case of panuveitis.
References
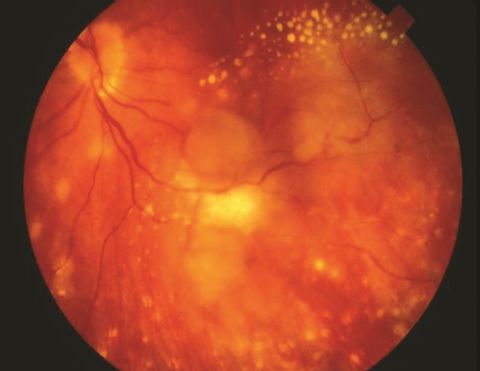
- ↑ Moorthy RS, Basic and Clinical Science Course, Section 9, 2013–2014. Courtesy of Albert T. Vitale, MD. © 2019 American Academy of Ophthalmology American Academy of Ophthalmology. Severe sarcoid panuveitis. https://www.aao.org/image/severe-sarcoid-panuveitis. Accessed July 08, 2019.
- ↑ Jump up to: 2.0 2.1 Sihota R, Tandon R. Parsons’ diseases of the eye. Elsevier India; 2015. 641 p.
- ↑ Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005 Sep;140(3):509–16.
- ↑ Jump up to: 4.0 4.1 4.2 Bowling B (Bradley). Kanski’s clinical ophthalmology : a systematic approach. Elsevier; 2016. 928 p.
- ↑ Friedman NJ, Kaiser PK, Trattler B. Review of Ophthalmology. Elsevier; 2017. 413 p.