Basic Approach to Diplopia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Background
Diplopia is a common presentation to neurology, neuro-ophthalmology, ophthalmology, and general medicine. This article will outline an approach to understanding diplopia by highlighting key facts in the history and exam to guide further workup.
History
The initial stage of diplopia workup is to identify whether it is monocular or binocular diplopia.
Monocular diplopia persists when the unaffected eye is closed but will resolve when the affected eye is closed. Thus, the key and differentiating question between monocular and binocular diplopia is “Does the double vision resolve with closing EITHER eye?” It is important not to ask the more vague and potentially misleading question “Does the double vision go away with covering ONE eye?”: if the patient happens to close the affected (monocular diplopia) eye, then the response might lead the examiner to conclude that the diplopia is binocular when, in fact, it is monocular.
Binocular diplopia resolves with either eye being closed and indicates ocular misalignment as an underlying problem. Monocular diplopia can be bilateral or unilateral, and sometimes patients with monocular symptoms complain of triplopia or more images. Monocular diplopia is typically due to an ocular cause. Cortical lesions can produce bilateral monocular polyopia, but it is rare.[1]
In binocular diplopia, key details to ascertain include those described below.
Are the images separated horizontally, vertically, or obliquely/diagonally? How does distance affect diplopia?
Binocular horizontal diplopia (images displaced horizontally) is usually due to disease of the medial or lateral rectus muscle, the neuromuscular junction, or the nerves supplying these muscles (e.g., cranial nerves [CN] III or VI). Diplopia worse with distance is more typical of sixth nerve palsy because of difficulty with divergence at distance of the eyes while diplopia worse at near is more suggestive of medial rectus palsy because of the need for convergence of the eyes at near.
Vertical diplopia (images displaced vertically) can be due to involvement of extraocular muscles, the neuromuscular junction (e.g., myasthenia gravis), or cranial nerves (e.g., CN III, IV). Myogenic involvement can occur with disease of the superior rectus, inferior rectus, superior oblique, or inferior oblique muscles alone or in combination. The 3-step test (described under Examination) is utilized to isolate the vertically acting weak muscle.
Which field of gaze provokes/worsens diplopia? In which field(s) of gaze are images closest to each other?
The worst position of gaze will typically represent the field of action of the paretic muscle. However, if there is muscle restriction (e.g., thyroid eye disease, orbital fracture, orbital myositis), then the diplopia may be worse in the opposite field of action of the restricted muscle.
Are there any corrective head positions? Is there any history of congenital strabismus?
The clinician should inquire about prior strabismus, a ‘‘lazy” or amblyopic eye, patching as a child, childhood eye surgery, and any abnormal head positions. Examining previous photos of the patient may also assist in determining the duration of any head tilt or prior ptosis or strabismus.
Is there any pain?
Localized pain in or behind the eye or orbit may suggest intraorbital pathology and headache may suggest intracranial pathology. Sudden onset of severe headache (e.g., worst headache of my life) may suggest a subarachnoid hemorrhage. A pupil-involving third nerve palsy may occur with subarachnoid hemorrhage from a ruptured posterior communicating artery aneurysm. Pain in the V1 and V2 divisions of the trigeminal nerve can suggest an intracranial (e.g., cavernous sinus) or intraorbital lesion.
What is the clinical course?
Onset, offset, variability, and progression of symptoms can aid in diagnosis and direction of workup depending on etiology (e.g., infectious, inflammatory, neoplastic).
Are there any associated neurological symptoms?
These can also assist with narrowing the differential diagnosis and can help topographically localize the lesion.
Examination
General Inspection
The presence of ptosis or anisocoria should be noted. Ptosis and diplopia from ophthalmoplegia with an ipsilateral mydriatic pupil may suggest a third nerve palsy versus an ipsilateral miotic pupil and mild ptosis, which may suggest a concomitant Horner syndrome.
Pupil Reaction
The patient should be examined for direct and indirect pupil reaction as well as anisocoria in the light and the dark. Assess for pupil constriction during accommodation and for relative afferent pupillary defect (RAPD) to look for associated optic neuropathy.
Eye Movements
In addition to duction and version testing, a cover test should be performed to detect any underlying tropia. The alternate cover test is useful for detecting underlying deviations kept in check by fusion. Prism cover test measurements should be performed in primary position and the diagnostic positions of gaze to quantify the deviation.
For monocular diplopia: Check for improvement of vision with the pinhole test. Monocular diplopia is usually due to refractive abnormalities (e.g., astigmatism, keratoconus, tear-film abnormalities, cataract); these symptoms will often improve with the pinhole test. If there is no improvement, one could consider cerebral monocular diplopia or polyopia, which is bilateral and extremely rare.
For binocular diplopia:
Eye movement evaluation involves tests of both pursuit and saccades. Determine whether pursuit movements are conjugate. Look for lag in eye movements. If there is ocular misalignment, establish whether it is comitant (same magnitude regardless of gaze position) or incomitant (magnitude of misalignment changes in different gaze positions). Comitant misalignment is typically found in patients with congenital or early-onset strabismus. Patients typically do not report double vision because of cortical suppression of one of the images.
Measure the ductions and versions in each field of gaze. Ask where the image separation is the greatest in order to define which extraocular muscles are involved.
Test saccadic eye movements by instructing the patient to fixate in alternation at 2 points 30 cm apart in the horizontal and vertical planes. Paresis reduces saccadic velocity; however, restrictive conditions should not. Forced duction testing can also differentiate paretic from restrictive pathologies: restrictive disease causes mechanical limitation to eye movements. Restrictive ophthalmoplegia (e.g., thyroid eye disease) also can cause a transient rise in intraocular pressure when the patient attempts to gaze in the direction opposite from the field of action of the restricted muscle.
In tropia/phoria assessment, when the misalignment is present without breaking fusion, this manifest deviation is called a tropia. If the ocular misalignment manifests only when fusion is disrupted (e.g., with the alternate cover test), it is termed a heterophoria or phoria.[2] The cover-uncover test is used to demonstrate a tropia. Each eye is covered separately; look for movement of the uncovered eye to pick up fixation. The alternate cover test detects phorias by breaking fusion.
Further assessment can be done with a Maddox rod and prisms, a sensitive clinical test for obtaining a quantitative measurement of the pattern and degree of misalignment. The double Maddox rod test helps identify and quantify torsional misalignment when vertical diplopia is present.
The 3-step test is a useful tool to isolate the muscle causing the symptoms in vertical diplopia.
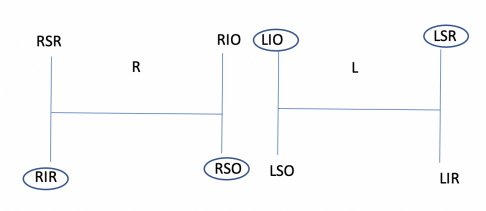
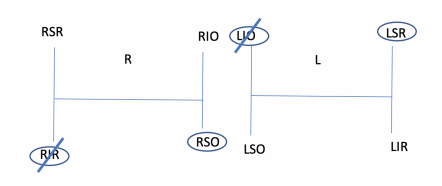
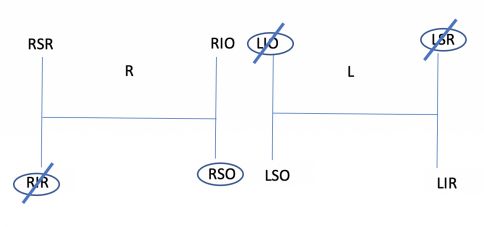
- Step 1: Determine which eye is higher in primary position: a right or left hypertropia (i.e., a higher right eye suggests either right hypertropia or left hypotropia). This suggests either weak right inferior rectus or right superior oblique or weak left superior rectus or left inferior oblique. Drawing two H diagrams representing the fields of gaze allows for easier conceptualization.
- Step 2: Determine the direction of gaze that worsens the double vision (e.g., right hypertropia worse on left gaze). From the 4 muscles in step 1, the left superior rectus and right superior oblique function in that field of gaze. In this example, horizontal gaze to the left increases the right hypertropia. The right eye in left gaze is in the adducted position and the left eye is in the abducted position. In the adducted position, the oblique muscles have better vertical action and thus this second step of the test implicates the right superior oblique muscle. In the abducted position, the vertical rectus muscles have better vertical action and thus this second step also implicates the left superior rectus muscle as a possible cause of the right hypertropia.
- Step 3: The final step is to determine the direction of head tilt that worsens diplopia (e.g., a right hypertropia worse on head tilt to the right). In this example, when the head tilts to the right side, the right eye must intort and the left eye must extort in order to maintain vertical orientation of the eyes relative to the environment. Diplopia (and the hypertropia) worse with head tilt to the right in this example suggests disease of either the right intorting muscle or left extorting muscle. From steps 1 and 2 of the test, only the left superior rectus and right superior oblique remain. Both of these extraocular muscles, however, intort the eye. Thus, this 3-step test implicates paresis of the right superior oblique muscle.
- Step 4 (additional): Measure the torsion with a double Maddox rod. For instance, in a weak right superior oblique muscle, the expected finding would be a right excyclotorsion. If the double Maddox rod findings are not consistent with what is expected, consider other diagnoses, most commonly skew deviation.[3]
- Step 5 (additional): If skew is suspected, have the patient lie down in a supine position and recheck the vertical deviation. In skew deviation, which is related to otolith dysfunction, supine positioning may reduce the vertical deviation due to decrease in firing of the vestibulo-ocular reflex.
Globe Examination
Exophthalmos is assessed clinically by looking down and from below the patient (“worm’s eye view”). The use of a Hertel or other exophthalmometer can also quantify proptosis further.
Other Cranial Nerves
This particularly involves nerves near the third, fourth, and sixth cranial nerves. These include the optic nerve (test for visual acuity, color vision, pupillary reaction [RAPD], and visual fields), trigeminal nerve (check sensation to the face and afferent arm of corneal sensation), facial nerve (test facial movements), and vestibulocochlear nerve (ask about hearing loss, vertigo, or dizziness). Assessing afferent visual function is essential. Retrobulbar optic neuropathy associated with CN III, IV, or VI dysfunction suggests an orbital apex syndrome.
Ophthalmoscopy
Optic disc edema, papilledema, or optic atrophy may be present and might assist with localization.
Diagnostic Approach
As mentioned, monocular diplopia is usually attributable to refractive or media abnormalities. Common causes include uncorrected astigmatism, corneal irregularities, tear-film abnormalities, and cataract. The hallmark of monocular diplopia from refractive abnormalities is improvement with pinhole. Cerebral monocular diplopia is bilateral and rare.[4]
Binocular diplopia indicates ocular misalignment as an underlying problem. The efferent ocular motor pathway is divided into supranuclear, nuclear, and internuclear segments. The infranuclear pathway is further subdivided into the peripheral nerve, the neuromuscular junction (NMJ), and extraocular muscular components.
Supranuclear Causes of Diplopia
In a vertical or horizontal gaze palsy, the first question to determine is whether the lesion is supranuclear or inter/infranuclear. An intact vestibulo-ocular reflex (VOR) using the doll’s head maneuver suggests a supranuclear etiology to ophthalmoplegia. A gaze palsy that is overcome with the doll’s head maneuver suggests a supranuclear etiology, as the brainstem and VOR pathway is intact. A gaze palsy that is not overcome by the doll’s head maneuver suggests an internuclear or infranuclear lesion.
Progressive Supranuclear Palsy
Progressive supranuclear palsy (PSP) is a neurodegenerative disease characterized by parkinsonism, ocular dysmotility, and cognitive decline. PSP should be suspected in patients with progressive neurodegenerative symptoms characterized by prominent postural instability with falls (early in presentation), vertical supranuclear palsy (especially downgaze) or slowing in saccades, and proximal more than distal dyskinesias, where the movement disorder responds poorly to levodopa.[5]
Parkinson Disease
Idiopathic Parkinson disease (PD) is characterized by resting tremor, bradykinesia, and lead-pipe rigidity. Ocular manifestations of PD include convergence insufficiency and binocular horizontal diplopia with an exotropia worse at near. Reduced blink rate, square-wave jerks, and impaired pursuits can also be seen; however, a supranuclear downgaze palsy as noted above is more characteristic of PSP.
Parinaud Syndrome (Dorsal Midbrain Syndrome)
Parinaud syndrome is a distinct supranuclear cause of ocular motor dysfunction. The dorsal midbrain contains the pretectal nuclei, Edinger-Westphal nuclei, posterior commissure, and tegmentum. Lesions of the dorsal midbrain vary from ischemic insults to neoplasms (especially pineal), hydrocephalus, or demyelination.
Skew
Skew deviation is a vertical deviation that does not localize to any one muscle or muscle group or single nerve or nerve pattern. In the vertical plane, there is misalignment of the eyes resulting from inappropriate utricular-vestibular-ocular output, which mimics the physiologic vertical deviations that normally compensate for head or body tilt. Multiple causes of skew deviation exist.
Vergence Dysfunction
Unlike other supranuclear disorders, vergence disorders usually result in diplopia. Convergence insufficiency relates to exodeviation greater at near than at distance fixation. Divergence insufficiency refers to esodeviation greater at distance than at near fixation.
Nuclear Causes of Diplopia
Oculomotor Nuclear Lesion
At the level of the superior colliculus, nuclear lesions of the third nerve result in bilateral ptosis or no ptosis due to involvement or lack of the single subnucleus controlling levator palpebrae superioris muscle. One or both pupils will be involved or spared due to the anterior and close location of the paired Edinger-Westphal nuclei to each other.[6] Most characteristic of nuclear involvement is unilateral palsy of the third cranial nerve in conjunction with weakness of bilateral superior recti muscle and bilateral ptosis.
Trochlear Nuclear Lesion
At the level of the inferior colliculus, isolated nuclear lesions of the fourth nerve are rare and give rise to contralateral palsies caused by the decussation.[6]
Abducens Nuclear Lesion
Horizontal gaze palsy refers to a lesion in the abducens nucleus (or parapontine reticular formation) within the pons that results in an ipsilateral gaze palsy and cannot be overcome by supranuclear activation such as the oculocephalic maneuver (the patient looks away from the brainstem).
Internuclear Causes of Diplopia
Internuclear ophthalmoplegia (INO) is characterized by a slowed adducting saccadic velocity in one eye with abducting nystagmus in the fellow eye on horizontal gaze. Patients may complain of binocular horizontal diplopia worse on horizontal gaze. INO localizes pathology to the medial longitudinal fasciculus (MLF) and may be associated with an exodeviation (e.g., exotropic monocular [EMINO] or bilateral INO [EBINO]).
Pontine lesions can also produce other ocular motor syndromes:
- One-and-a-half syndrome: This pontine pathology involves the MLF and the parapontine reticular formation (PPRF) or CN VI on the same side of the brainstem. This results in the only preserved movement of the eye in the horizontal plane being abduction of the contralateral eye (i.e., horizontal eye movements are lost in one eye and “half” lost in the fellow eye, hence the name).
- Eight-and-a-half syndrome: This condition involves the facial nerve nucleus in addition to the lesions in one-and-a-half syndrome (7 + 1.5 = 8.5). Stroke is the most common cause of this disorder.
Infranuclear Causes of Diplopia
Cranial Neuropathies
Cranial nerve palsy can be a result of compression, ischemia, infiltration, infection, or inflammation. Multiple neuropathies are worrisome as they can be suggestive of brainstem, subarachnoid, or cavernous sinus disease, or if involving the optic nerve, they can reflect orbital apex disease. When they occur in the brainstem, they can involve other nearby structures as described below.
Third Nerve Palsy
Fascicular lesions of the third nerve can be associated with hemiparesis, tremors, or ataxia if ventral midbrain structures like the corticospinal tracts, red nucleus, and cerebellar peduncles are compromised.[6] Ocular symptoms involve ptosis, mydriasis, and extraocular muscle paralysis including superior rectus, inferior rectus, medial rectus, and inferior oblique muscles.
Fourth Nerve Palsy
Trauma, small vessel ischemia, and decompensated congenital fourth nerve palsies are common. Compressive, infiltrative, infectious, and neoplastic etiologies may also occur.
Sixth Nerve Palsy
Fascicular lesions of the abducens nerve produce an isolated abduction deficit, but they can be accompanied by other neurological deficits like facial nerve palsy, hemiparesis, or sensory loss from involvement of the facial nerve fascicle, corticospinal tract, or medial lemniscus, respectively.
Cavernous Sinus and Superior Orbital Fissure Involvement
Ipsilateral cranial nerve dysfunction involving any one or combination of CN III, IV, V1, V2, and VI, along with sympathetic fibers (i.e., Horner syndrome), suggests a cavernous sinus lesion; in particular, CN V and sympathetic fiber involvement localizes specifically to the cavernous sinus. Additionally, the offending lesion can also involve the optic canal or the orbital apex compromising the optic nerve (orbital apex syndrome).
Muscular and Neuromuscular Junction
Orbital Disease
Diplopia can be the first, and sometimes only, sign of diseases affecting the orbit, which include thyroid eye disease, inflammatory diseases, neoplasm, trauma, and congenital myopathies. The red flags for orbital disease are proptosis, periorbital edema, resistance to retropulsion, and lid retraction. Neuroimaging of the orbit (e.g., MRI or CT orbit) is recommended for orbital signs and symptoms.
Myasthenia Gravis
Myasthenia gravis (MG) can mimic any pattern of painless, pupil-spared, nonproptotic ophthalmoplegia. MG is characterized by postsynaptic acetylcholine receptor antibodies affecting the neuromuscular junction. It has a predilection for highly metabolic and fatigable extraocular muscles. Red flags for generalized (rather than ocular) MG include trouble swallowing/breathing or generalized weakness. Ocular MG findings include ptosis, fatigability of muscles, and orbicularis weakness. Orbicularis ‘‘peek’’ sign (scleral show after short period of lid opposition to gentle closing pressure), Cogan lid-twitch sign (twitching of eyelid after downgaze and return to primary position), or enhancement of ptosis may suggest MG.
Summary
Diplopia is a common symptom in neuro-ophthalmology. The history and exam should establish if the diplopia is monocular (typically ocular in origin) or binocular (misalignment). The examination should localize to supranuclear, nuclear, or infranuclear pathways. The most common supranuclear causes of diplopia include convergence insufficiency and neurodegenerative disease. The most common internuclear ophthalmoplegia is an INO and involves the medial longitudinal fasciculus. The infranuclear pathway includes the peripheral ocular motor cranial nerves (CN III, IV, VI), the neuromuscular junction (e.g., MG), and the extraocular muscles themselves (e.g., thyroid eye disease). Clinicians should be aware of the various etiologies for diplopia.
Additional Resources
- Patient information brochure: Double vision. North American Neuro-Ophthalmology Society (NANOS). Accessed March 3, 2025. https://www.nanosweb.org/Diplopia_information_brochure
References
- ↑ Keane JR. Triplopia: thirteen patients from a neurology inpatient service. Arch Neurol. 2006;63(3):388-389.
- ↑ Dinkin M. Diagnostic approach to diplopia. Continuum (Minneap Minn). 2014;20:942-965. doi:10.1212/01.con.0000453310.52390.58
- ↑ Spierer A. Measurement of cyclotorsion. Am J Ophthalmol. 1996;122(6):911-912.
- ↑ Coffeen P, Guyton DL. Monocular diplopia accompanying ordinary refractive errors. Am J Ophthalmol. 1988;105(5):451-459.
- ↑ Eggenberger ER. Supranuclear eye movement abnormalities. Continuum (Minneap Minn). 2014;20(4 Neuro-ophthalmology):981-992. doi:10.1212/01.CON.0000453308.50604.52
- ↑ Jump up to: 6.0 6.1 6.2 Cornblath WT. Diplopia due to ocular motor cranial neuropathies. Continuum (Minneap Minn). 2014;20(4 Neuro-ophthalmology):966-980. doi:10.1212/01.CON.0000453309.44766.b4