COVID-19 Associated Orbital Mucormycosis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Rhino-orbital cerebral mucormycosis (ROCM) has recently emerged as a serious long-term manifestation in patients affected by Covid-19. The diagnosis of COVID-19 associated mucormycosis remains challenging and requires a high degree of clinical suspicion.
Disease Entity
Disease
Rhino-orbital cerebral mucormycosis (ROCM) is an uncommon life-threatening invasive fungal infection caused by the angiotropic fungus belonging to the order Mucorales. It is a fulminant disease with high rates of morbidity and mortality despite treatment that mainly affects immunocompromised patients; it almost always occurs in patients with uncontrolled diabetes mellitus (70% of the cases present as a complication of a diabetic ketoacidosis (DKA) event), hematologic cancers, and solid organ or hematopoietic stem cell transplants. The condition originates in the nasal region and paranasal sinuses, but it is often suspected following orbital spread, explaining its poor prognosis. Depending on the location of the infection, the mucormycosis can be rhino-orbito-cerebral (most common), pulmonary, gastrointestinal, cutaneous, or disseminated, as the infiltrating fungus destroys the surrounding bone and soft tissue through vascular thrombosis and subsequent tissue infarction. It may reach the brain with fatal complications. Although it has a low incidence rate, varying from 0.005 to 1.7 per million population, an alarming rise in cases of rhino-orbital mucormycosis in patients with past or current COVID-19 infection has been observed during the height of the COVID-19 pandemic. The suspicion or diagnosis of rhino-orbital cerebral mucormycosis triggers a medical as well as surgical emergency, and delay in treatment increases morbidity and mortality.
Although the majority of reports on COVID-19-associated ocular manifestations describe self-limiting conjunctivitis and rare neuro-ophthalmic manifestations (e.g., optic neuritis, ocular motor cranial neuropathies), the overreaching health implications and long-term sequelae associated with the viral pandemic are still unknown. Separate case reports (10–14) have been emerging describing ROCM coinfection in COVID-19-positive patients. A number of hospitals mostly located in India, Pakistan and Egypt, have reported an increased rate of ROCM cases during the first wave of the COVID-19 pandemic. [1]
Etiology
Mucorales is the largest and best studied order of zygomycete fungi.
- Rhizopus oryzae
- Rhizopus microsporus
- Mucor racemosus
- Rhizomucor pusillus
Risk Factors
- Critically ill patients who have undergone invasive procedures
- Patients on mechanical ventilation / prolonged ICU stay
- Uncontrolled diabetes
- Long-term corticosteroid therapy
- Long-standing oxygen therapy
- Associated immunodeficiency conditions
- Immunomodulation treatments
- Comorbidities( i.e. malignancy / post-transplant)
- Voriconazole treatment
- Iron and/or aluminum overload
- Protein energy malnutrition
Pathophysiology
COVID-19 causes :
- Dysregulated immunological response
- Cytokine storm
- Thrombotic inflammatory phenomenon
- Microvascular coagulopathies
All of which lead to exhaustion of the immune system, rendering a patient more susceptible to developing opportunistic fungal infections.
Primary Prevention
Preventative measures against rhino-orbito-cerebral mucormycosis in the setting of COVID-19 include:
- Judicious and supervised use of systemic corticosteroids in compliance with the current preferred practice guidelines
- Judicious and supervised use of tocilizumab in compliance with the current preferred practice guidelines
- Aggressive monitoring and control of diabetes mellitus
- Strict aseptic precautions during oxygen administration (sterile water for the humidifier, daily change of the sterilized humidifier and the tubes)
- High personal and environmental hygiene
- Betadine mouth gargle (not nasal drops)
- Barrier mask covering nose and mouth
- Consider oral prophylactic oral Posaconazole in high-risk patients (>3 weeks of mechanical ventilation, >3 weeks of supplemental oxygen, >3 weeks of systematic corticosteroids, uncontrolled diabetes mellitus with or without ketoacidosis. prior history of chronic sinusitis, and co-morbidities with immunosuppression)
Diagnosis
Signs & Symptoms
The most common warning signs and symptoms of rhino-orbito-cerebral mucormycosis include :
- Eyelid, periocular/and facial edema swelling
- Rapidly progressive eyelid drooping
- Ocular motility restriction
- Diplopia
- Sudden ptosis
- Sudden vision loss
- Regional facial, orbit, paranasal sinus or dental pain
- Facial palsy / paresthesia / anesthesia
- Nasal stuffiness
- Nasal mucosal erythema, inflammation, purple or blue discoloration, white ulcer, ischemia, or eschar
- Epistaxis
- Mucoid, purulent, blood-tinged or black nasal discharge
- Foul odor
- Palatal eschar
- Eyelid, periocular, facial skin discoloration
- Fever, altered sensorium, paralysis, focal seizures
Diagnostic Procedures
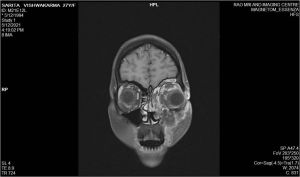
- Magnetic Resonance Imaging of the orbit and brain (with gadolinium contrast)
- Diagnostic nasal endoscopic evaluation: Revealed inflamed and edematous nasal mucosa. Necrotic middle turbinate with eschar. Biopsy from the nasal specimen confirmed the presence of aseptate fungi on the KOH mount. Mucor was seen growing on Sabouraud dextrose agar medium on day 3.
Differential Diagnosis
- Allergic fungal sinusitis manifesting due to allergic reaction to dematiaceous fungi can produce a clinical picture of sinusitis with proptosis and rhino-cerebral mass in immunocompetent hosts. However, it does not invade the tissue and often lingers for months to years. Many patients could have underlying asthma, allergy, mucosal polyps, and elevated IgE levels. The eosinophil-rich fungal mucin can erode into adjacent orbit and intracranial space. Bony erosions have been reported due to the pressure effect of thick mucin.
- Invasive aspergillosis in the form of rhino-orbital cerebral aspergillosis can produce a sinusitis-like picture with orbit and brain involvement and is increasingly reported in immunocompromised patients, and the outcome is extremely poor.
- Painful eyes could be due to inflamed lids, conjunctivitis, or preseptal and orbital cellulitis.
- Subperiosteal hematomas, inflammatory pseudotumors, cavernous sinus thrombosis, and orbital neoplasms can produce protrusion of the eyeball
- Bacterial orbital cellulitis
- Cavernous sinus thrombosis
- Orbital apex syndrome
Management
IV amphotericin, along with surgical debridement, is the key management strategy.
General treatment
Early recognition and identification are the most important factors for proper management, so that timely intervention can be achieved.
Management of predisposing factor
- Control of diabetes and/or diabetic ketoacidosis
- Steroid reduction aiming to discontinue rapidly
- Discontinuation of immunomodulating treatment
- No antifungal prophylaxis treatment needed
Medical Therapy
- Installation of peripherally inserted central catheter (PICC line)
- Maintain adequate levels of system hydration
- IV normal saline infusion before Amphotericin B infusion
- Antifungal therapy for at least 4-6 weeks
- Iron chelation therapy
- Clinical monitoring of patient with radio-imaging for response and to detect disease progression
Surgery
Surgical debridement may be required for extensive resection of all infected and necrotic tissues as an attempt to control the source and reduce fungal load. Debridement also provides adequate tissue biopsy specimens for definite histopathologic confirmation. Dissection is usually continued until normal, well-perfused bleeding tissue is reached since mucormycotic tissues are less likely to bleed due to extensive thrombosis of vessels. Removal of the palate, nose cartilage, and orbit would cause significant disfigurement. The orbital involvement may need orbital decompression or exenteration. The role of routine orbital exenteration or the timing of exenteration is currently unclear, and cases with orbital involvement have also been successfully managed without exenteration.
References
- ↑ Fouad Yousef A., Abdelaziz Tougan Taha, Askoura Anas, Saleh Mohamed Ibrahim, Mahmoud Mohammad S., Ashour Doaa Maamoun, Ashour Manar Maamoun. Spike in Rhino-Orbital-Cerebral Mucormycosis Cases Presenting to a Tertiary Care Center During the COVID-19 Pandemic. Frontiers in Medicine , Vol.8, 2021,pg 716. DOI:10.3389/fmed.2021.645270. ISSN 2296-858X