Gonioscopy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
History
Gonioscopy was first described in the early 1900s. The Greek ophthalmologist, Alexios Trantas, used the word “gonioscopy”, with the Greek root “gonia” meaning “angle” and “skopein” to “observe.” He described the anterior chamber angle using a direct ophthalmoscope and simultaneous digital pressure on the limbal region. Years later Maximilian Salzmann was the first to use a contact lens and indirect gonioscopy for examination of the angle. Today, both are regarded as the “fathers of gonioscopy”.[1] [2]
Today, gonioscopy is a critical exam technique used for visualizing the anterior chamber angle. Due to total internal reflectivity at the tear-air interface, the angle cannot be seen without a gonioscopy lens. Use of a contact gonioscopy lens allows light to pass through the tear-air interface and bounce off a mirror to the examiners eye. Visualization of the anterior chamber angle provides the clinician with critical diagnostic exam findings.
There are many great resources available for learning gonioscopy. The website http://www.gonioscopy.org is a recommended starting point with excellent videos and narration.
Today, there are many applications for gonioscopy. With the advent of Micro-invasive Glaucoma Surgeries (MIGS), intraoperative gonioscopy is required to visualize the angle and preoperative gonioscopy in the clinic is critical to identifying appropriate candidates for these procedures. Further, it is the standard of care to perform gonioscopy on every new glaucoma patient or glaucoma suspect to establish the status of the angle. Due to the discomfort of the exam, gonioscopy often needs to be performed during exams under anesthesia in children.
How to Perform Gonioscopy
- Gonioscopy is usually performed at the slit lamp and requires application of a gonio lens to the surface of the eye. The eye should be numbed prior to beginning the examination.
- Prior to placing the lens on the eye, fill the concave aspect of the lens with a methylcellulose solution. Special care should be taken to avoid introducing bubbles into the fluid.
- To apply the lens to the eye, while the patient is looking up, the examiner should place the inferior aspect of the edge onto the inferior sclera. The patient should then be instructed to look forward, and the gonio lens should be tipped forward, making contact and a seal with the cornea.
- Gonioscopy should be performed in a relatively dark room. A brightly lit room will constrict the pupil, opening the angle, and possibly missing iridotrabecular contact (ITC) and apposition. Likewise, a shorter and less bright slit beam should also be used. Care should be taken to maintain only a light pressure on the lens as too much pressure versus slight pulling on the lens may cause artificial compression or expansion of the angle.
Lenses
- Gonioscopy is required to visualize the chamber angle because under normal conditions light from the angle structures undergoes total internal reflection at the tear-air interface. To overcome this, a lens must be placed against the eye.
- Depending on the type of lens used, the angle can be examined either directly or indirectly.
Direct gonioscopy
- Allows for direct visualization of the chamber angle. Examples of direct gonio lenses include Koeppe, Barkan, Wurst, Swan-Jacob, or Richardson lenses.
- During direct gonioscopy, the viewer has an erect view of the angle structures.
- Direct gonioscopy is most easily performed with the patient supine and in the operating room for an exam under anesthesia or a MIGS procedure.
Indirect gonioscopy
- Examples of indirect gonioscopy lenses include the Posner, Sussman, Zeiss, and Goldmann lenses. These are more commonly used in the clinic setting. The viewer in indirect gonioscopy will have an inverted and slightly foreshortened image of the opposite angle because the light from the angle is reflected off a mirror and directed towards the viewer.
- The Posner, Sussman, and Zeiss lenses have a smaller area of contact than the Goldmann-type lenses. This allows the examiner to apply pressure to the cornea, which may cause Descemet’s membrane folds, and falsely open the angle. The examiner can also deepen the angle, which is discussed more below in the dynamic gonioscopy section. The Goldmann lens does not allow for this indentation because of the size of the lens. [3]
Procedure
Indirect Gonioscopy
- As with any procedure, the patient and the examiner must be positioned in a comfortable fashion.
- A drop of topical anesthetic should be applied to the conjunctiva of both eyes.
- If using the Goldmann lens, contact gel is placed in the concave part of the lens.
- If using a Posner or similar type lens, a drop of artificial tears can be placed on the concave surface.
- The patient is then asked to open both eyes and look upwards.
- The examiner can then pull down slightly on the lower lid and places the lens on the surface of the eye.
- The patient is then asked to look straight ahead.
- Most examiners choose to start with the inferior angle as it is usually a bit more open, and the pigmentation of the trabecular meshwork is slightly more prominent, allowing for easier identification of the angle structures.
- Continue identifying all angle structures in all 4 quadrants, and then repeat with the other eye.
Dynamic Gonioscopy
- In eyes with a closed angle, one must distinguish between an anatomically closed angle with iridotrabecular contact (ITC, apposition) and peripheral anterior synechiae (PAS).
- To perform dynamic or compression gonioscopy, you will need to be using either the Posner, Sussman, or Zeiss style lens.
- The patient is positioned as noted above. Gentle pressure is placed on the cornea, and aqueous humor is forced into the chamber angle.
- If there is ITC or apposition, the angle will open and the structures should become more visible.
- If PAS is present, the angle will stay the same in the affected areas. Examine all areas of the angle and repeat on the other eye.
Direct Gonioscopy
- Direct gonioscopy is most easily performed with the patient in a supine position. It is commonly used in the operating room for examination of the eyes of infants under anesthesia. It is essential for performing goniotomies or other angle-based surgeries, including MIGS.
- It can be performed using a direct goniolens and either a binocular microscope or a slit-pen light.
- Examples of direct goniolenses include Koeppe, Barkan, Wurst, Swan-Jacob, or Richardson lenses.
- The lens is positioned after saline or viscoelastic is placed on the eye, which can act as a coupling device.
- The lens provides direct visualization of the chamber angle (ie, light reflected directly from the chamber angle is visualized) in an erect position.
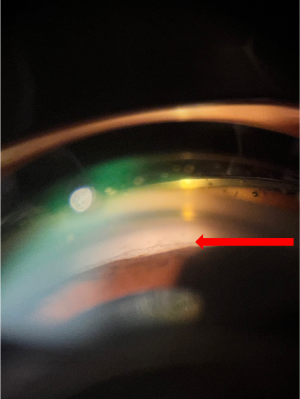
Anatomical Structures of the Normal Angle
The most important part of gonioscopy is identification of the anatomical landmarks. There are many normal variations that one must be aware of. We will discuss these below, moving from most anterior to posterior.
Schwalbe’s Line
- Schwalbe’s line is a condensation of collagen tissue and interfaces with the edge of Descemet’s membrane.
- Schwalbe’s line is an important landmark to identify because normal vessels and tissue will not cross it. Neovascularization or PAS may pass Schwalbe’s line anteriorly.
- A prominent Schwalbe’s line is also called a “posterior embryotoxon” and can be found in normal individuals. There is no increased risk of glaucoma in these eyes.
- A Sampaolesi line is a defined as an abundance of pigment at Schwalbe's line. This is commonly seen in pigment dispersion syndrome or pseudoexfoliation (Figure 1).
- An important technique in identifying Schwalbe’s line is the corneal light wedge, which allows the observer to determine the exact junction of the cornea and trabecular meshwork. To perform this technique, the examiner must use a narrow slit beam. They will see 2 reflections, one on the external surface of the cornea and the other on the internal surface indicating the corneal epithelium and endothelium, respectively. Schwalbe’s line can be found where the 2 reflections intersect.
Trabecular Meshwork
The trabecular meshwork is an important pigmented landmark for diagnostic purposes, incisional surgery, and laser surgery. The amount of pigmentation may vary from person to person, and even from quadrant to quadrant. The amount of pigmentation should be included in the grading of an angle.
Schlemm’s Canal
Schlemm’s canal drains the aqueous humor after passing through the trabecular meshwork. It is only visible when there is blood in the canal. It is an important structure as many surgical procedures target this area, especially many of the new MIGS devices.
Scleral Spur
The scleral spur is comprised of a ridge of collagen tissue and appears white on gonioscopy. Identifying this structure helps to differentiate open angles from closed angles. It is possible for the scleral spur to be covered by small sharp-ended iris processes that reach up to the trabecular meshwork. They do not cross the trabecular meshwork and have no pathologic consequence.
Ciliary Muscle Band
The anterior ciliary body band can be seen in eyes with deeper angles. It represents the longitudinal fibers of the ciliary muscle. This is the site of nonconventional or suprachoroidal outflow and is also a landmark for newer surgical procedures.
Iris Root and Iris
The insertion of the iris is an important part of the classification of angle anatomy. The configuration of the peripheral iris is also important to note when studying angle structures. Pathology that exists in this part of the angle includes ITC or apposition and PAS, which should be noted.
Grading Systems
Gonioscopy grading systems were established to provide a standardized description of the anatomy of the anterior chamber angle. There are many grading systems used today.
Scheie
The Scheie system is based upon visibility of the anatomical structures of the angle. They are graded Wide followed by I through IV, with Wide being open with all structures visible, and IV being closed with no visible structures. See Table 1 for an in-depth description of the Scheie system.
| Grade | Visibility | Interpretation |
|---|---|---|
| Wide | Wide | Open, all structures visible |
| I | Slightly Narrowed | Ciliary body visible, but recess obscured by the last roll of the iris |
| II | Apex not visible | Ciliary body not visible |
| III | Posterior half of trabecular meshwork not visible | Ciliary body, scleral spur, and posterior half of the trabecular meshwork not visible |
| IV | None of the angle structures visible | Cliary body, scleral spur, and trabecular meshwok not visible |
Shaffer
The Shaffer system is based on angularity. It follows a numbers-based grading system using degrees of angularity. See Table 2 for detailed description of the Shaffer classification system.
| Angular Grade | Width (in degrees) | Grade | Clinical Interpretation |
|---|---|---|---|
| Wide Open Angle | 45-35 | 4 | Angle closure impossible in both Grades 3 and 4 |
| 35-20 | 3 | ||
| Narrow Angle | 20 | 2 | Angle closure possible |
| Narrow Angle, extreme | 10 or less | 1 | Angle closure probable, eventually |
| Narrow Angle, slit | Critically narrowed angle, quite possibly against the trabecular meshwork beyond Schwalbe’s line | - | - |
| Narrow angle, partial or complete closure | 0 | 0 | Angle closed in part or all of circumference |
Spaeth
The Spaeth system is much more complex and describes each detail of the anatomic angle. This system describes the iris insertion, angularity, configuration, and pigmentation of the posterior trabecular meshwork. We will illustrate this detailed description below.
Iris Insertion
Designated by letter A-E. A is anterior to Schwalbe’s line, B is between Schwalbe’s and the scleral spur, C is at the scleral spur, D is deep, E is extremely deep.
Iris Angularity
The angle of the iris is defined as the angle between two lines. The first line is parallel to the trabecular meshwork and the second a tangent to the anterior iris surface approximately 1/3 of the distance from the most peripheral portion of the iris. It is usually noted between 10 and 40 degrees.
Iris Configuration
This is named for the configuration or shape of the iris as it runs from the papillary margin to the insertion. S is for steep, B for bowing anteriorly, P for plateau, R or F for regular or flat, respectively, and C for concave posteriorly.
Pigmentation
This is graded on a 0 to 4 scale noting the amount of pigmentation in the posterior trabecular meshwork.
The Spaeth system also considers dynamic or compressive gonioscopy. If a letter is in parentheses, this means it is the originally viewed insertion prior to compression. It is then followed by a letter without parentheses, which denotes the insertion after compression. An example is (B)D30P1. This is an angle that is thought to have an iris insertion between Schwalbe’s line and the scleral spur. After compression, it is noted that the insertion is deep, with an angle of 30 degrees and a plateau configuration with grade 1 pigmentation of the trabecular meshwork.
Becker
The Becker classification focuses on the amount of trabecular meshwork present and the distance between the scleral spur and the insertion of the iris. Numbers (0-3) are used to describe how much trabecular meshwork is present. Letters (A-C) are used to describe the level of iris insertion. Table 3 shows the details of this system.
| 0 | 1 | 2 | 3 | |
| 0 | Angle closed | Small trabecular zone, iris insertion not visible | Average width of trabecular zone, iris insertion not visible | Broad trabecular zone, iris insertion not visible |
| 1 | Small trabecular zone, iris insertion anteriorly | Average width of trabecular zone, iris insertion anteriorly | Broad trabecular zone, iris insertion anteriorly | |
| 2 | Small trabecular zone, iris insertion in the middle | Average width of trabecular zone, iris insertion in the middle | Broad trabecular zone, iris insertion in the middle | |
| 3 | Small trabecular zone, iris insertion posteriorly | Average width of trabecular zone, iris insertion posteriorly | Broad trabecular zone, iris insertion posteriorly |
Shaffer-Kanski
This system is based on the width of the angle as previously described in the Shaffer system and the risk of angle closure. [4] See Table 4.
| Grade Angle (°) | Visiblity of structures | Risk of angle closure |
|---|---|---|
| 0 | 0 No structures visible | Closed angle |
| 1 | 10 Schwalbe’s line, possibly anterior trabecular meshwork visible | Closure possible |
| 2 | 20 Schwalbe’s line and trabecular meshwork visible | Narrow, closure unlikely |
| 3 | 20-35 Schwalbe’s line, trabecular meshwork and scleral spur visible | Closure impossible |
| 4 | 35-45 All structures visible from Schwalbe’s line to ciliary band | Closure impossible |
Van Herick
This is a non-gonioscopic grading system. It uses an estimation of the peripheral anterior chamber depth. It is done at the slit lamp and is most helpful before dilation. A thin slit beam is angled approximately 60 degrees and aimed at the cornea peripherally near the limbus. The corneal thickness is compared to the anterior chamber depth. The ratio is then used to provide information on the width of the chamber angle. Because it is done without gonioscopy, no angle structures can be identified. As such, this should not replace gonioscopy. See Table 5.
| Grade Cornea: | Peripheral anterior chamber ratio | Risk of angle closure Angle (°) |
|---|---|---|
| 4 | 1:1 or higher | Very unlikely or impossible 35-40 |
| 3 | 1:1/2 | Unlikely or improbable 20-35 |
| 2 | 1:1/4 | Possible 20 |
| 1 | 1:<1/4 | Likely or probably 10 |
| 0 | No anterior chamber slit visible | Closed 0 |
Documentation
Proper documentation is important to monitor patients over time. Both written documentation and drawings are acceptable ways of communicating findings. One can use any of the above mentioned classification systems or any drawing tool that is available in your charting system.
Other Uses of Gonioscopy
As discussed above, gonioscopy is extremely useful in determining how open or narrow an angle is and the possibility of it becoming closed. There are also many other indications and uses for gonioscopy. Knowing the anatomy described above will help with identifying any pathology that may be present.
- Peripheral anterior synechiae (PAS) can be confused with iris processes, however, PAS are pathologic and represent adhesions between the iris and the trabecular meshwork. Indentation or dynamic gonioscopy can be used to differentiate the two; with PAS, the angle will not open when pressure is applied to the lens where with iris processes, the angle opens. The formation of peripheral anterior synechiae and the identification of this is extremely important. Depending on the severity, this can decide a treatment approach or indication for a peripheral laser iridotomy.
- Plateau iris occurs in the setting of an anteriorly placed ciliary body resulting in the iris blocking, or partially blocking, the trabecular meshwork. On gonioscopy, two “humps” are typically seen. The outer hump represents the ciliary body pushing up against the iris while the inner hump represents the lens pushing against the iris. On slit lamp exam, the patient will often have a normal angle as well as a flat iris. Plateau iris configuration and plateau iris syndrome are further explained in the eyewiki plateau iris article.
- Blood in Schlemm’s canal can be seen in patients with increased episcleral venous pressure such as carotid cavernous fistulas. It can also be present with hypotony.
- Neovascularization may be noted in patients with uncontrolled diabetes or a history of retinal vein occlusions or ocular ischemic syndrome. There are other conditions that may cause neovascularization as well.
- Other findings that can be visible with gonioscopy include hyphemas, microhyphemas, foreign bodies, iris or uveal tumors, and iridodialysis or other damage to angle structures.
The importance of gonioscopy cannot be understated and should be used routinely for evaluation and diagnosis of many different ophthalmologic conditions. It is a valuable skill that should be used by all ophthalmologists, not just glaucoma specialists.
References
- ↑ Faschinger C, Hommer A. Gonioscopy. Springer-Verlag Berlin Heidelberg; 2012.
- ↑ Wallace L M Alward MD RALM. A Brief History of Gonioscopy. https://www.aao.org/education/disease-review/brief-history-of-gonioscopy. Published 2017. Accessed2022.
- ↑ Wallace L M Alward MD RALM. Techniques of Slit-Lamp Gonioscopy. https://www.aao.org/disease-review/techniques-of-slit-lamp-gonioscopy. Published 2017. Accessed2022.
- ↑ Alward, WLM, Longmuir, RA. American Academy of Ophthalmology. Gonioscopic Grading Systems. Color Atlas of Gonioscopy. https://www.aao.org/disease-review/gonioscopic-grading-systems Accessed October 07, 2021.