Management of Submacular Hemorrhage
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Submacular Hemorrhage: Management Options and Literature Review
Bozho Todorich, PhD, Harry W. Flynn, Jr., MD, Ingrid U. Scott, MD, MPH, Rodrigo Jorge, MD, PhD, Cathleen M. McCabe, MD
Abstract: The goal of the following outline is to define subretinal hemorrhage, provide differential diagnosis of its etiology, and provide a comprehensive review on the mechanistic, animal and clinical studies (including case reports, retrospective case series and prospective randomized clinical trials) involving management of submacular hemorrhage. Specifically, the evolution of the submacular surgery (with and without tissue plasminogen activator (tPA)), pneumatic displacement, macular translocation, photodynamic therapy and recently use of anti-VEGF inhibitors is reviewed. In addition, results of group B of submacular surgery trials are reviewed in detail. The document is intended to be an introduction into management of submacular hemorrhage for ophthalmology residents and vitreoretinal fellows, with an emphasis on appreciation of how developments over the years have shaped the current treatment recommendations today. The document will be periodically updated as new studies and evidence become available.
Abbreviations: CNV (choroidal neovascularization), RPE (retinal pigment epithelium), RAP (retinal angiomatous proliferation), nAMD (neovascular age related macular degeneration), POHS (presumed ocular histoplasmosis syndrome), VEGF (vascular endothelial growth factor), APMPPE (acute posterior multifocal placoid pigment epitheliopathy), ILM (internal limiting membrane), SRH (subretinal hemorrhage), SMH (submacular hemorrhage), PVR (proliferative vitreoretinopathy), tPA (tissue plasminogen activator), ERG (electroretinography), RDs (retinal detachments), BCVA (best corrected visual acuity), SST (submacular surgery trials), PDT (photodynamic therapy), PPV (pars plana vitrectomy), IV (intravitreal), BSS (balanced saline solution), HM (hand motion), CF (count fingers), LP (light perception), NLP (no light perception), PDR (proliferative diabetic retinopathy), NPDR (non-proliferative diabetic retinopathy), SO (silicon oil), RAMA (retinal artery macroaneurysm), DME (diabetic macular edema), IOP (intraocular pressure), FAZ (foveal avascular zone), ETDRS (early treatment diabetic retinopathy study), RZB (ranibizumab), BVZ (bevacizumab), VH (vitreous hemorrhage).
Submacular hemorrhage
Definition
Subretinal hemorrhage is an accumulation of blood between the neurosensory retina and the retinal pigment epithelium (RPE) arising from the choroidal or retinal circulation.
Etiology
There are several pathologies that can be associated with subretinal hemorrhage, including choroidal neovascularization (CNV, likely the most common cause), trauma (especially in the context of choroidal rupture), and infiltrative process. The differential diagnosis for subretinal hemorrhage is listed below:
1. Choroidal Neovascularization (CNV)
Associations:
- AMD (CNV type 1, under the RPE); (CNV type 2, under the neurosensory retina); (CNV type 3, RAP lesion)
- POHS (CNV type 2, under the neurosensory retina)
- High myopia
- Trauma (choroidal rupture)
- Angioid streaks
- Inflammation of the retina/choroid, including PIC.
- Idiopathic
2. Events during surgical procedures:
- Drainage of subretinal fluid in scleral buckle procedures
- Inadvertent scleral perforation (strabismus, SBP, Baerveldt)
- Associated with localization of melanoma margins during radioactive plaque placement
- Laser photocoagulation
3. Penetrating ocular trauma:
- Choroidal rupture
- Hemorrhagic retinal detachment
- Combined suprachoroidal hemorrhage and subretinal hemorrhage
4. Other:
- Ruptured retinal artery macroaneurysm (classically multi-layered hemorrhage including sub-ILM)
- Valsalva (usually sub-ILM)
- Sickle cell disease
- Necrotic tumors
- Optic disc drusen
- Coagulopathies
- Central retinal vein occlusion
- Diabetic retinopathy
Summary:
Experimental model, animal studies
- Irreversible photoreceptor damage in merangiotic and holangiotic animal models of subretinal hemorrhage after 1-3 days as a result of:
- Stripping of photoreceptor outer segments due to clot contraction
- Toxic effect of iron (Fenton-mediated oxidative stress to the photoreceptors with subsequent photoreceptor apoptosis)
- Establishment of diffusion barrier between RPE and neurosensory retina (blocks the bidirectional nutrient exchange and trophic relationship between RPE and photoreceptors).
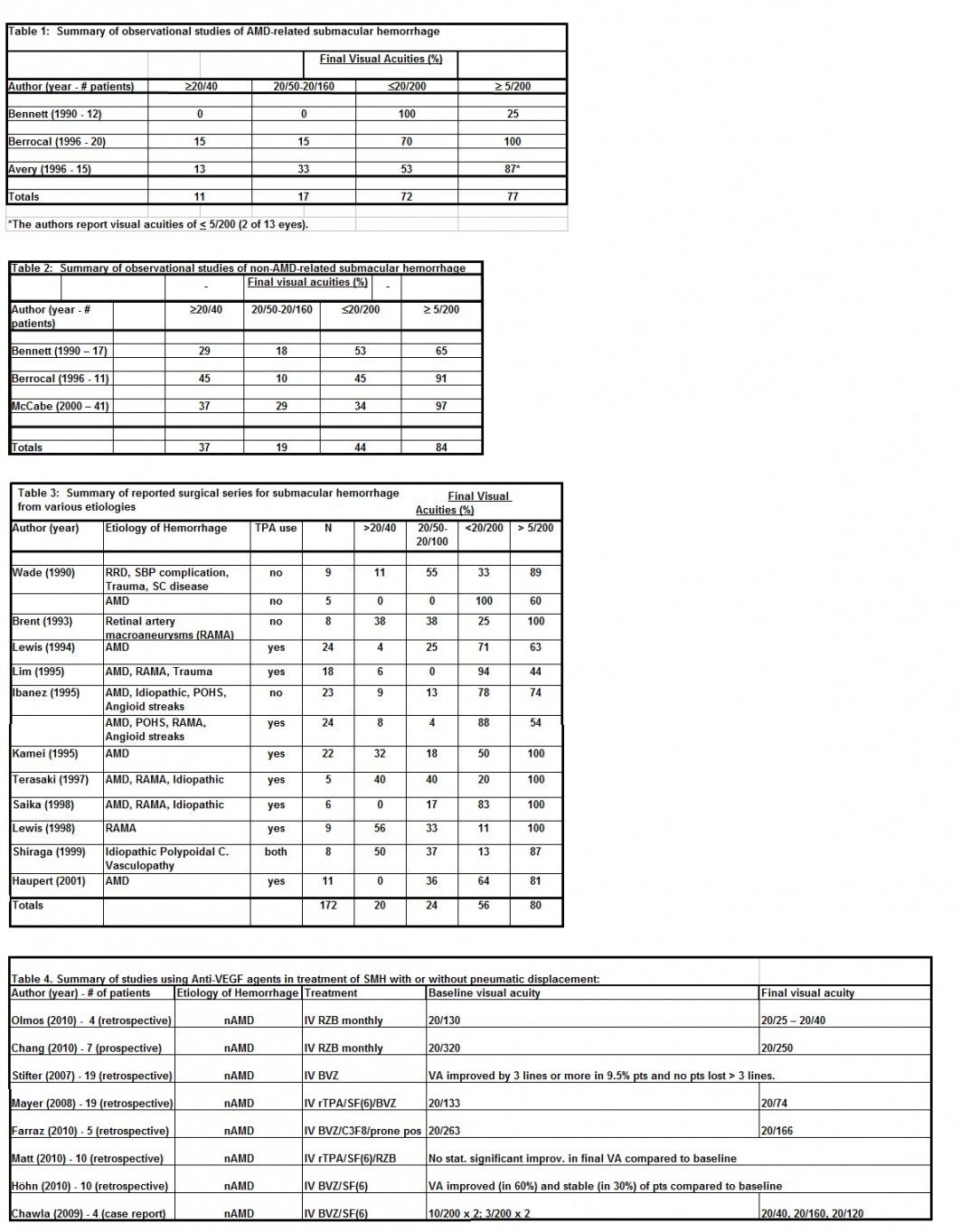
Non-surgical, observational studies
- Reported visual outcomes in eyes with SMH are variable
- Factors associated with a poorer visual prognosis may include:
- Presence of CNV
- Thicker SRH
- ARMD etiology
- Larger hemorrhage
- Good visual outcome is sometimes possible in select patients with SMH managed without surgical intervention.
Surgical removal of SMH without tPA
- Early intervention may show trend toward improved post-operative visual outcome
- Major post-operative events include persistent or recurrent CNV with disciform scarring and PVR with recurrent RD
- Extraction of SMH may be traumatic when large retinotomies are created and shearing forces during mechanical extraction of the clot.
Animals studies with tPA
- Tissue plasminogen activator (tPA) is a serine protease with fibrin-specific thrombolytic activity that forms a complex with fibrin to activate plasminogen to plasmin which then cleaves fibrin and dissolves the clot.
- Possible advantages include:
- decreased fibrin-mediated photoreceptor damage
- early lysis may allow earlier removal of hemorrhage and shorter duration of toxic and barrier effect of blood on retina.
- Toxic effect of vehicle in tPA, but apparent safety with doses 25-50 ug
- Faster clearance of hemorrhage, less photoreceptor damage histopathologically, but scotopic ERG remains decreased in one study
- Proposed but not proven benefit of intravitreal tPA to hasten clot lysis prior to surgical extraction of hemorrhage
- Some studies show that Intravitreal tissue plasminogen activator does not diffuse through the intact neural retina to reach a subretinal clot.
Surgical removal of SMH with tPA
- Advantages may include smaller retinotomy and less traumatic surgery (less trauma by the photoreceptors by dissolving fibrin clot with tPA).
- Variable VA outcomes with tPA. Poorer outcomes associated with longer duration of hemorrhage, AMD etiology, presence of CNV
- One study with no difference in outcome with or without tPA (Ibanez)
- Potential toxic effect of tPA must be kept in mind (safe dose is about 50 ug per injection in humans); toxicity may result in RPE changes and exudative RDs.
- Maybe of benefit in polypoidal choroidal vasculopathy
Submacular Surgery Trials
- Group B: NEI sponsored, randomized clinical trial comparing submacular surgery vs observation for treatment of large submacular hemorrhage secondary to subfoveal CNV related to nAMD.
- No benefit of submacular surgery for CNV-associated submacular hemorrhage in nAMD patients over observation alone
- No statistically significant difference in percentage of patients experiencing loss of BCVA in submacular surgery vs. observation arm.
- No statistically significant difference in percentage of patients experiencing improvement of BCVA in surgery vs. observation arm.
- No differences in changes of reading speed or threshold contrast sensitivity in surgery vs. observation arm.
- Subgroup analysis showed no benefit of use of tPA (used in approximately 38% of cases) over non-tPA surgical evacuation of SMH in the surgery arm.
- Secondary benefit of prevention of severe vision loss (21% of surgery eyes and 36% of observation eyes had lost more than 6 lines of BCVA from baseline).
- Complication rate (cataracts, rhegmatogenous retinal detachment, proliferative vitreoretinopathy) much higher in surgery arm relative to observation.
Macular translocation
- PPV followed by circumferential peripheral retinotomy, evacuation of SMH and macular rotation +/- RPE patch grafting.
- Results are variable with improvement in BCVA observed in patients with severe macular hemorrhage and vision loss.
- Bruch’s membrane-RPE patch grafts can improve visual outcome in select number of cases.
- Proliferative vitreoretinopathy, recurrence of choroidal neovascularization, cataracts and recurrent retinal detachment are main complications.
Photodynamic therapy
- In a small number of reports PDT successful in treatment of SMH
- Visual outcomes noted VA improvement or at least stabilization of visual acuity
- Further studies needed to define efficacy of PDT and its use with IV gas and/or anti-VEGF agents.
Pneumatic displacement:
- IV injection of expansile gas that requires prone positioning for several hours, followed by face down positioning for 3-4 days.
- May allow more rapid improvement in VA when used with intravitreal tPA or anti-VEGFs
- Controversial whether IV tPA can cross into subretinal space through intact retina (tPA does not cross the retina in rabbits after intravitreal injection).
- Efficacy in improving BCVA with pneumatic displacement in combination with IV tPA and/or anti-VEGFs encouraging; the positioning requirement limits usefulness in older patients.
Use of anti-VEGF agents in SMH
- Thin and extrafoveal SMH is best treated with intravitreal anti-VEGF agents alone
- Growing body of evidence suggests that intravitreal anti-VEGF therapy alone or in combination with pneumatic displacement strategies can preserve and improve visual acuity in patients with SMH due to CNV related to nAMD.
- The use of anti-VEGF compare favorably to surgical approaches to management of SMH in terms of efficacy, risk, complications and cost.
- There is a need for prospective randomized clinical studies to definitively establish the long-term efficacy of anti-VEGF therapies in CNV-related submacular hemorrhage in AMD.
Conclusions
- Natural history series of submacular hemorrhage show variable visual outcomes, largely dependent on etiology of SMH and its location with respect to the fovea.
- SMH related to CNV in nAMD has particularly poor prognosis if untreated, especially if large size and very thick submacular heme.
- Currently, there appears to be no or at most minimal relative benefit of submacular surgery vs. observation for submacular hemorrhage due to CNV in nAMD, as evidenced by Submacular Surgery Trials Group B.
- Alternative surgical approaches with macular translocation and RPE patch grafting have mixed outcomes and are yet to be prospectively evaluated.
- Benefit of adjunctive use of tPA remains uncertain (vitrectomy and pneumatic displacement), although preliminary reports were promising.
- Adjunctive anti-VEGF agents with pneumatic displacement without vitrectomy shown to be effective in growing number of retrospective reports.
- In several mainly retrospective studies and one small prospective study with limited number of patients, IV anti-VEGF agents alone have shown promising results in treating submacular hemorrhage from neovascular AMD.
- Future prospective studies with greater number of patients are needed to help clarify the efficacy of anti-VEGF therapies for treatment of CNV-associated SMH.
Summary of clinical studies
Experimental studies in animal model
1. Glatt & Machemer, AJO, 1982[1]
- Injected autologous blood beneath retina in merangiotic rabbits
- Air, BSS, silicone oil controls; also adjacent areas of serous RD.
- 1 hour: few edematous photoreceptors
- 1 day: absent or edematous photoreceptors, pyknosis of outer nuclear layer, inner retina normal to cystoid space formation and pyknosis, some completely normal
- 3 days: onset of karyolysis (thinning of outer nuclear layer), inner retina with cystoid spaces and pyknosis, some areas normal.
- 7 days: photoreceptors few in number, macrophages with hemosiderin, outer nuclear layer severe karyolysis, inner nuclear layer normal to cystoid spaces and pyknosis.
- 2 weeks: blood and fibrin gone, macrophages with hemosiderin, outer nuclear layer absent, inner nuclear layer normal to severe karyolysis.
- Conclusions:
- Irreversible photoreceptor damage in as little as 24 hours.
- Non-vascularized retina more severely affected.
- Retinal changes secondary to:
- Toxic effect of iron (hemosiderin)
- Barrier effect between retina and RPE (supported by silicone oil control)
- Tractional forces by contraction of the clot
2. Toth et al., Arch Ophthalmol., 1991[2]
- Holangiotic cat model of subretinal hemorrhage (autologous blood)
- 25 minutes: fibrin in clot forms dense interdigitations with photoreceptor outer segments.
- 1 hour: sheets of photoreceptor outer and inner segments torn off, overlying retina appears normal.
- 1 day: retina with only minimal degenerative changes
- 2-3 days: increased organization of clot, degeneration of torn photoreceptor outer segments, hemosiderin-laden macrophages, intact photoreceptors with vacuolization and degeneration, inner layer minimally affected.
- 7 days: significant destruction of outer retinal elements, inner layer with increasing vacuolization.
- 14 days: severe destruction of outer retinal layers, increased number of phagocytic cells
- BSS and tPA blebs with intact photoreceptor outer segments, no significant morphological changes.
Observational studies
1. Bloome & Ruiz, AJO, 1978[3]
- 8 patients with massive spontaneous subretinal hemorrhage
- 1 patient without submacular hemorrhage recovered 20/20 vision
- Remaining 7 patients with 20/200 (1). HM (3), LP (1), NLP (1), enucleation (1)
- Conclusion: Recommended conservative management, possible PPV late in course to remove organized blood, early PPV dangerous unless melanoma completely ruled out.
2. Gillies & Lahav, Annals Ophthalmol, 1983[4]
- 3 cases subretinal hemorrhage
- myopia, trauma, ARMD/CNVM
- Initial VA CF, 20/400, CF
- Final VA 20/40, 20/25, 20/67
- Conclusion: SRH can clear without intervention with good visual outcome.
3. Nasrallah et al., AJO, 1989[5]
- 8 patients with atrophic ARMD and subretinal hemorrhage without identifiable CNV
- Initial VA 20/30 to CF
- Final VA same
- None with blood under fovea
- Conclusion: hemorrhages in areas of atrophy not always associated with CNV, good prognosis for resolution of hemorrhage.
4. Bennett et al., AJO, 1990 (retrospective chart review)[6]
- 29 patients with large (> 1 DD) submacular hemorrhages, no other cause for decreased vision
- Initial VA LP to 20/70
- Final VA LP to 20/30
- Follow-up of at least 6 months (6-144 months)
- Conclusion: risk factors for poorer VA outcome:
- ARMD (n=12)
- Diseased RPE and retina less tolerant of blood
- Blood more often located sub-RPE as well as subretinal
- “thicker” (obvious elevation on stereoscopic viewing)
- more complete barrier to diffusion
- ARMD (n=12)
- Patients with choroidal rupture (n=5) with best final VA (average 20/35)
5. Hayasaka et al., Graefe’s, 1990.[7]
- 24 eyes with high myopia (> - 8.00 D)
- 15 without CNVM
- Blood cleared by 3 months
- Final VA same or improved in all at 3 months and 1 year
- 9 with CNVM
- VA unchanged or worse at 1 year
- 15 without CNVM
- Conclusion: Poorer visual prognosis in patients with CNV.
6. Avery et al, Retina, 1996 (retrospective chart review)[8]
- 41 eyes from 40 patients with ARMD
- subfoveal hemorrhage making up > 50% of lesion
- follow-up at 3 (n=30),6,12,24,36 (n=15) months
- VA decreased over time (average 3.5 lines at 36 months)
- However, 33% with improved or stable VA at 36 months
- Conclusion: VA outcome correlated with initial size (MPS disc areas) and elevation (stereoscopic viewing of color fundus photos; graded none, minimal, moderate, or marked) of hemorrhage. Variable visual acuity outcomes, some patients with stable or improved vision.
7. Berrocal et al., AJO, 1996 (retrospective chart review)[9]
- 31 eyes with submacular hemorrhage from variety of causes
- 20 with ARMD etiology
- 11 with non-ARMD etiology
- Follow-up 3 months to 6 years (mean 29 months)
- Thickness and size of lesion not correlated with final VA
- Conclusion: Poorer VA associated with presence of SRNVM, good visual outcomes possible in eyes without SRNVM.
8. Morse et al., Retina, 1997[10]
- Retrospecive review of 49 patients with SRH and PDR treated with PPV but no removal of subretinal blood
- 14 patients with SMH
- 71% of these with stable or improved VA, 71% with > 5/200 VA
- Conclusion: SRH resolved spontaneously and did not prevent retinal reattachment. Visual prognosis guarded but may recover ambulatory vision.
9. Scupola et al., Ophthalmologica, 1999.[11]
- 60 eyes of 54 patients with ARMD and subfoveal hemorrhage > 1 DD
- Initial VA 20/70 to LP (average. 20/240)
- Mean F/U 24 months
- Final VA worse in 80% (20/100-LP)
- Anatomic outcome: fibrous tissue proliferation (38%), atrophic scar (25%), RPE tear (22%)
- Conclusion: The visual outcome in eyes with submacular hemorrhages due to AMD is very poor. Poorer visual prognosis correlates with increased size and thickness of the hemorrhage.
10. Uyama et al., Archives of Ophthalmology, 1999.[12]
- 35 eyes of 32 Japanese patients with idiopathic polypoidal choroidal vasculopathy, 6 eyes with submacular hemorrhage 2-3 DD in size
- On follow-up (average 20 months), serous fluid or blood resolved in all cases
- Subretinal hemorrhage recurred in 2 patients, one of these resulted in disciform scarring
- 17 eyes treated with laser photocoagulation, resulting in resorption of hemorrhage and fluid in 12 eyes, 4 eyes lesions increased in size and persisted for prolonged period
- Outcomes: favorable in 67% overall, improved VA in 71% of eyes treated with laser photocoagulation
- Conclusions: Visual acuity outcomes better in patients not treated with laser, overall favorable prognosis compared with AMD.
11. McCabe et al., Archives of Ophthalmology, 2000.[13]
- 41 patients with macular hemorrhage from ruptured retinal artery macroaneurysm managed with observation only
- Retrospective review from multiple centers
- Initial VA 20/200 or less in 37 eyes (90.3%), 20/70 in 3 (7.3%), and 20/80 in 1 (2.4%)
- Final VA 20/40 or better in 15 eyes (37%), between 20/50 and 20/100 in 12 (29%), and 20/200 or less in 14 (34%)
- Mean F/U 15.7 months
- Mean time for clearance of SRH was 4.6 months
- Late macular pigmentary changes observed in 23 eyes (56%) associated with poorer visual outcomes
- Conclusions: Management with observation alone can result in good visual acuity outcomes.
Surgical treatment of subretinal hemorrhage
1. Dellaporta, AJO, 1983.[14]
- Drainage of 10-week-old massive traumatic subretinal hemorrhage by endodiathermy needle puncture of retina, choroid, and sclera
- VA improved from 3/200 to 20/25.
2. Hanscom & Diddie, Arch Ophthalmol, 1987.[15]
- 2 patients with submacular hemorrhage (ARMD, RAMA)
- Drained with PPV, retinotomy, clot extraction (1st reported cases)
- Initial VA CF, HM
- Final VA 20/400, 20/80
- Conclusion: Drainage of subretinal hemorrhage may be beneficial.
3. de Juan & Machemer, AJO, 1988[16]
- 4 eyes with ARMD managed with PPV, drainage +/- irrigation of clot, scar removal
- Final VA improved in 3 eyes, none better than 5/200
- Conclusion: Improved visual acuity in ¾, PVR with recurrent RD (2 eyes) secondary to large retinotomies (major complication).
4. Han et al., Arch Ophthalmol, 1990.[17]
- 19 consecutive cases with traumatic hemorrhagic RD managed with PPV/SBP/FGX +/- internal drainage
- Anatomic reattachment 68%
- Final VA > 5/200 in 32%
- Removal of blood easier after 10 days when clot liquefied
- 37% needed repeat PPV for PVR, recurrent RD, or subretinal fibrosis
- Conclusion: Indications for removal of subretinal hemorrhage in traumatic posterior segment injury include: 1) hemorrhagically elevated retinal breaks, 2) massive hemorrhagic RD of posterior pole, 3) bullous detachment of the retina.
5. Wade et al., Arch Ophthalmol, 1990.[18]
- 14 eyes with submacular hemorrhage managed with PPV and internal drainage
- 5 eyes with ARMD etiology: all with < 5/200 final VA
- 9 eyes with non-ARMD etiology: 8 with > 20/400 final VA (5 with recurrent RD, of these, 1 with recurrent RD not reattached).
- Conclusion: Selected patients can achieve improved VA and anatomic reattachment with this procedure. Results in ARMD poorer and limited by underlying disease process.
6. Vander et al., Ophthalmology, 1991.[19]
- 11 patients with AMD and massive subretinal hemorrhage, VA < 20/400
- 6/11 patients with vision loss 4 days to 1 week, 1 for 12 weeks, 4/6 with vision loss for 1 year or more
- Blood aspirated, clot mechanically extracted, retinotomy enlarged (to 9 mm in one patient)
- Tamponade with SF6 (8), C3F8 (1), SO (2)
- Final VA (F/U 3-18 months) improved in 4 (36%) patients [20/400 (1), 20/200 (2)] all with symptoms <1 week, remainder with 20/800 - LP VA
- 4 (36%) developed RD secondary to PVR, 3 of these underwent re-op with SO
- Conclusion: Recommended surgical drainage only in desperate cases.
7. Mandelcorn & Menezes, Can J Ophthalmol, 1993.[20]
- 7 eyes with ARMD
- PPV/internal drainage
- 3 patients with removal of CNVM
- 4 without removal
- 5 patients with improved VA, none worsened.
- Conclusion: Best results in those with < 2 week h/o vision loss and those without removal of CNVM.
8. Machemer & Steinhorst, Graefe’s, 1993.[21]
- 3 cases ARMD with massive recent submacular hemorrhage
- Managed with PPV, retinotomy, macular translocation
- Cyclotorsional complaints (excyclotorsion 30 to 60 degrees)
- Final VA: 20/80, 20/400, 3.5/200
- Conclusion: Possible new procedure in cases with ARMD and massive hemorrhage.
9. Rubsamen et al., AJO, 1994.[22]
- 9 patients with massive subretinal hemorrhage from complications of SBP managed with PPV and internal drainage of SRF.
- Sources of SRH: deep suture (4), drainage of SRF (3), depressor entry into staphyloma (1)
- Final VA improved in all eyes; VA > 20/80 in 7/9 (78%)
- Conclusion: Subgroup of patients with massive SMH have good anatomic and visual prognosis with prompt PPV and internal drainage.
10. Ibanez et al., Arch Ophthalmol, 1995.[23]
- 47 consecutive cases
- Group 1
- 23 cases; ARMD (20), POHS (1), angioid streaks (1), idiopathic (1)
- managed with mechanical clot extraction
- mean final VA 20/200 for ARMD, 20/70 for non-ARMD
- Group 2
- 24 cases; ARMD (19), POHS (2), RAMA (2), angioid streaks (1)
- tPA-assisted (10-40 ug) drainage
- Mean final VA 20/480 ARMD, 20/60 non-ARMD
- Conclusion: No benefit with tPA, patients with ARMD have worse VA outcomes.
Animal studies using tPA
Tissue Plasminogen Activator (tPA) (defined): thrombolytic enzyme, when bound to fibrin markedly increased affinity for plasminogen, converts to plasmin which breaks down fibrin.
1. Johnson et al., Arch Ophthalmol, 1990.[24]
- Toxicity study of intravitreal tPA in albino rabbit (doses 25, 50, 75, 100ug in 100 ul)
- BSS control
- 25 ug: no toxic effects; 50 ug: 1 of 4 eyes with loss of photoreceptors; 75 ug: 3 of 4 eyes with severe retinal damage; 100 ug: all 4 eyes with severe retinal damage.
- Conclusion: Intravitreal tPA toxicity at doses of 50 ug or greater. Toxicity appears related to vehicle rather than enzyme, as 100 ug of vehicle caused similar damage.
2. Lewis et al., AJO, 1991.[25]
- Study of subretinal tPA in albino rabbits: toxicity and efficacy in facilitating removal of subretinal hemorrhage
- Group 1:
- a) 12 eyes with 25 ug/0.1ml
- b) 12 eyes with 50 ug/0.1 ml
- c) 12 eyes with BSS
- Group 2:
- a) 24 eyes injected with subretinal blood only
- b) 24 eyes subretinal blood followed by tPA 30 minutes later
- c) 24 eyes subretinal blood followed by BSS 30 minutes later
- Histopathology examined Days 1, 3, and 7
- Conclusions:
- No evidence of toxicity Group 1a-c
- Blood cleared faster in eyes with tPA or BSS than in eyes with blood alone (14, 19 vs. 28.5 d)
- Progressive degeneration with loss of photoreceptors in the area of subretinal blood in eyes with blood alone, less damage in eyes with tPA or BSS (? Dilutional effect).
3. Benner et al., Arch Ophthalmol, 1991.[26]
- Study of toxic effect of subretinal tPA on cat retina
- BSS controls (9)
- 32 eyes treated with 0.0125 to 10 ug (2.5 to 1000 mg/L) tPA
- Conclusion: Demonstrated toxic effect on retina of vehicle in human recombinant tPA; toxicity threshold between 1 and 10 ug in the cat.
4. Toth, et al., AJO, 1992.[27]
- Microsurgical technique for removal of subretinal hemorrhage with the use of tPA in the cat (n=3)
- 1 to 2 day-old clotted hemorrhage treated with stereotactic micromanipulator with controlled microinfusion of tPA for 60 seconds (total dose 0.5 to 5 ug). After 20 minutes, clot aspirated.
- 14 days after clearance of blood, histopathology with normal photoreceptor outer segments to few areas with shortening, vacuolization, and distortion.
- Conclusion: Advances in microsurgical instrumentation and use of subretinal tPA lavage may decrease retinal damage with SRH.
5. Johnson et al., Ophthalmology, 1992.[28]
- 19 rabbit eyes, 13 cat eyes; model of subretinal hemorrhage
- 24 hours after subretinal clot induction, animals treated with tPA (50 or 250 ug) in 10 rabbit eyes with vitrectomy 60 or 180 minutes later, or repetitive lavage and aspiration of tPA or BSS during vitrectomy in 9 eyes. Rabbits were sacrificed immediately after vitrectomy.
- Similar treatment with intra-operative tPA lavage was performed on 7 cat eyes, and 3 eyes were treated with 2.5 ug tPA 10 minutes after subretinal hemorrhage induction. Cats were sacrificed 14 days after treatment.
- Injection of tPA into the clot had minimal effect at 60 or 180 minutes.
- Subretinal tPA lavage decreased size of clot but retinotomy size became large secondary to friability of retina overlying clot.
- Lavage with BSS had no effect.
- After average 4 injection of tPA with lavage in the cat, small residual clot removed through small retinotomy.
- 4 cat eyes with severe outer retinal atrophy over clot, 2 with normal appearance -- ? reason for difference.
- Cat eyes treated with tPA at time of hemorrhage did not form clots, but developed loss of photoreceptors and outer nuclear layer over areas of nonclotted thick blood.
- Conclusion: tPA-assisted removal of SRH with intra-operative lavage can result in less retinal damage (2 eyes), future improvements in microsurgical instrumentation important.
6. Coll et al., Retina, 1995.[29]
- 34 albino rabbits with experimental subretinal hemorrhage
- 24 eyes with intravitreal tPA (50 ug in 0.1 ml) 1 day later
- 10 control eyes with intravitreal BSS
- Clots disappeared within 24 hours with tPA, present at 3 days in control group
- Scotopic ERG amplitudes markedly reduced for both groups at 7,14, and 14 days
- Conclusion: tPA results in faster resolution of hemorrhage but does not protect against retinal damage.
7. Benner et al., Ophthalmology, 1994.[30]
- 23 subretinal hemorrhages formed in cat model using Nd:YAG laser
- 14 observed, 6 treated with 0.3 to 1.4 ug tPA and aspiration (2-15 retinal punctures required), 3 mechanically removed through retinotomy without tPA
- 14 days after hemorrhage,12 eyes with SRH 3DD or greater had severe outer retinal atrophy and gliosis over center of clot, 2 eyes with smaller hemorrhage had only minimal changes
- 14 days after tPA-assisted removal of 7 day-old hemorrhage variable retinal atrophy present, from outer retinal thinning (in 2 eyes) to minimal changes
- Conclusion: Basal dimension a predictor of retinal damage, less damage to retina with use of tPA.
8. Morse et al., BJO, 1996.[31]
- tPA treatment of subretinal hemorrhage without removal of blood in the cat model (4 eyes)
- 0.5-1.0 ug tPA injected into 4 day old hemorrhages, histopathology evaluated at 21 days.
- 4 days after SRH induction, 0.5-1.0 ug tPA injected into hemorrhage
- hemorrhage migrated inferiorly in 48 hours
- 21 days after treatment, severe outer retinal degeneration in initial location of hemorrhage and area migrated to, but not intervening retina
- 1 small (< 2 DD) SRH with minimal retinal damage
- Conclusion: Removal of SRH important to prevent damage, small basal diameter of hemorrhage correlates with better prognosis.
9. Boone et al., Retina, 1996. [32]
- 18 pigs with SRH (holangiotic vasculature and pigmented RPE)
- 1 day later, treated with intravitreal 0.1 ml BSS (6 eyes) or tPA (25 ug) (12 eyes)
- Day 2 six eyes treated with tPA underwent removal of SRH with PPV
- Partial (~25%) liquefaction of blood at time of PPV, all eyes with moderate to severe photoreceptor damage
- Hemorrhages cleared at same rate in both tPA and BSS treated eyes
- All eyes (18) with moderate to severe photoreceptor damage by day 10
- Conclusion: Only partial clot lysis with intravitreal tPA, not sufficient to allow removal of clot with aspiration alone.
10. Kamei et al; Am J. Ophthalmol, 1999.[33]
- 36 pigs:18 with SRH and 18 controls
- 18 pigs injected with tPA labeled with fluorescein and rhodamine
- 18 pigs injected with labeled tPA 2 hours after induction of the subretinal clot
- Conclusion: Intravitreal tPA did not diffuse trough the intact neural retina to reach the subretinal clot
Surgical removal of SMH without tPA.
Surgical removal of subretinal blood using tPA
1. Peyman et al, Ophthalmic Surgery 1991.[34]
- 2 patients with RAMA, 3 with AMD and SRH treated with PPV, subretinal tPA (6.25 ug/0.05 mL x 1 or 2), and aspiration of clot through small retinotomy
- RAMA: CF to 20/50, CF to 20/70 (duration of hemorrhage 3-10d)
- AMD: CF to 20/400, 20/300 & 20/400 no change (duration of hemorrhage 2-14d)
- Conclusion: Use of tPA results in smaller retinotomy, less traumatic surgery.
2. Vander, Ophthalmic Surgery, 1992.[35]
- Case report: 1 patient with large SMH secondary to AMD x 1 week
- Treated with PPV/subretinal tPA (50 ug/0.2 ml x 3)/ perfluorocarbon/ aspiration of blood and perfluorocarbon in vitreous/ SF6
- VA 3/200 improved to 20/100 at 4 months post-op
- Conclusion: Large hemorrhage can be drained through small retinotomy with use of tPA.
3. Kimura et al., (letter), Retina, 1994.[36]
- 6 patients with moderate-size SRH (2-4 days old) treated with 6 ug/0.1 ml tPA intravitreally 12-36 hours prior to surgery
- PPV/aspiration +/- perfluorooctane
- All 6 cases, SRH completely liquefied, no forceps for clot removal required
- Conclusion: Surgery combined with tPA can mobilize SRH.
4. Lewis, AJO, 1994.[37]
- 24 eyes with < 14 day-old SMH secondary to AMD treated with PPV/subretinal tPA (12-48 ug in 0.1-0.5 mL)
- 17 eyes with 70-90% clot liquefied, 7 eyes with < 30% clot liquefied, clot mechanically extracted with forceps
- results: VA “improved” in 20 eyes (83%): 1 (4%) > 20/40, 6 (25%) 20/50-20/125, 17 (71%) < 20/200
- RRD in one eye, underwent repeat PPV, 1 macular hole 6 weeks post op, 1 SRH after tPA injected
- Conclusions: Worse prognosis in eyes with SMH > 7days, extending outside arcades, and with hemorrhagic PED; tPA important adjunct.
5. Millsap et al., Ophthalmic Surgery, 1994.[38]
- Case report: 2 day-old SRH secondary to AMD treated with PPV/multiple small retinotomies/subretinal tPA (25 ug in 0.1 mL) with suction and backflushing through retinotomies
- VA HM to CF @ 3 ft.
- Conclusion: Technically easier removal of hemorrhage rather than through one retinotomy.
6. Laatikainen & Mattila, Acta Ophthalmol Scandin, 1995.[39]
- Case report: 20 y/o with 14 day-old SMH secondary to traumatic choroidal rupture removed with PPV/subretinal tPA (25 ug)/ repeat PPV with SF6
- Six months later VA 20/30.
- Conclusion: PPV with subretinal tPA is a viable surgical option for treatment of SMH due to choroidal rupture.
7. Lim et al., Ophthalmology, 1995.[40]
- Retrospective review of 18 patients with < 14 day-old SMH > 4 MPS disc areas in size secondary to AMD (16), RAMA (1), penetrating trauma (1) treated with PPV/subretinal tPA (6-12 ug/0.1 ml X 1-3 applications)/ perfluorooctane/BSS lavage; no mechanical clot extraction
- Results: 6% > 20/40, 0% 20/50-20/100, 94% < 20/200
- Conclusions: Focused on improvement in VA > 2 lines in 11 (61%), final VA limited by underlying disease.
8. Moriarty et al., Eye, 1995.[41]
- 15 patients with 2 day to 8 week-old SMH (> 5 DD) secondary to AMD (14) or RAMA (1) treated with PPV/subretinal tPA (25 ug/0.1 ml x 1-2 applications)/aspiration/SF6
- VA improved in 13 (87%), RRD in 2 (13%)
- Conclusion: Smaller retinotomy with tPA, need for prospective study.
9. Kamei et al., AJO, 1996.[42]
- 22 eyes with (5-100 days old) SMH (at least 1 DD centered on fovea) secondary to AMD treated with PPV/subretinal tPA (25 ug/0.1 ml x 0.05 to 0.20 ml)/perfluorocarbon/aspiration/SF6
- Results: VA improved in 18 (82%); 32% > 20/40, 18% 20/50-20/100, 50% < 20/200
- 4 eyes with recurrent subretinal hemorrhage, 3 (14%) eyes with RD, 7 eyes with recurrent or persistent CNVM, 3 eyes with ERM
- Poorer prognosis in eyes with SMH > 30 days, CNVM
- 9/11 eyes with SMH 8-25 days with VA > 20/200 ~ 6/7 with SMH < 7 days with 20/200 VA
- Conclusion: Improved VA outcome in patients treated with tPA and perfluorocarbon, less traumatic to retina.
10. Terasaki et al., AJO, 1997.[43]
- 5 eyes with 3-14 day-old SMH (5-13 DA) secondary to RAMA (3), AMD (1), unknown etiology (1) treated with PPV, subretinal tPA (20 ug/ 0.2 ml x 1-3 applications)/perfluorocarbon/aspiration
- Measured pre- and post-operative macular ERG
- Results: ERG recovered somewhat from pre-op value; ERG reduced post-operatively in 4 eyes compared with normal fellow eye, 5th eye with abnormal fellow eye
- Abnormality consistent with photoreceptor +/- off-center bipolar cells
- Uncertain cause of decreased ERG (hemorrhage, tPA, or both)
- Conclusion: significant improvement of ERG response after evacuation of SRH (non-recordable pre-op, and recovered post-op).
11. Hesse et al., Ger J Ophthalmol, 1997.[44]
- 8 eyes with 2h to 14 day-old SRH (1-6 DD in size) secondary to AMD treated with PPV/6-75 ug subretinal tPA/aspiration/mechanical clot extraction/SF6
- Only partial clot liquefaction in all eyes, requiring additional mechanical extraction of clot
- VA improved in 4, stabilized in 3, worsened in1; VA > 20/200 in 4 (50%)
- Severe RPE loss all patients, RRD in 1 patient
- Conclusion: No clear benefit with tPA as only partial clot lysis.
12. Steinhorst et al., Ophthalmologica, 1997.[45]
- Case report: 12 y/o with 5 day-old traumatic SMH treated with PPV/subretinal tPA (12 ug/0.1 ml)/continuous lavage for 30 minutes/aspiration/SF6
- Continuous lavage preferable to multiple injections with syringe
- VA 20/300 improved to 20/30 (10 months after surgery)
- No additional hemorrhage observed and no fibrovascular proliferation from hemorrhage.
- Conclusion: PPV with submacular tPA followed by BSS lavage a viable option for SMH due to traumatic choroidal rupture.
13. Humayun et al., AJO, 1998.[46]
- 9 eyes with < 7day-old SMH (> 3 MPS DA) secondary to a ruptured RAMA treated with PPV/subretinal tPA (12.5-50 ug)/aspiration/SF6 or C3F8
- Results: 56% > 20/40, 33% 20/50-20/100, 11% < 20/200
- Conclusions: Improved VA outcomes in recent SMH from RAMA with tPA, prospective randomized study needed.
14. Chaudry et al., Ophthalmic Surg Lasers, 1999.[47]
- 5 eyes with recent (< 7 days) SMH secondary to AMD > 3 mm thick involving fovea and good (>20/70) prior VA treated with subretinal tPA (25 ug in 0.1 ml) 24 hours prior to PPV/drainage
- Pre-op VA HM (3) to CF (2)
- Post-op VA improved in 4/5 (20/400, 20/200, 20/60, 30/30), remained HM in one (had CNV with recurrent hemorrhage), with F/U of 3-24 months
- Conclusions: Pre-op tPA appears to be safe and may be helpful in clot removal in patients with thick SMH.
15. Shiraga et al. Am J Ophthalmol, 1999.[48]
- 8 eyes of eight consecutive patients with thick submacular hemorrhage associated with idiopathic polypoidal choroidal vasculopathy;
- Visual acuity improved or stabilized in 7 eyes; 4 eyes with VA> 20/40
- Conclusion: Surgical intervention may be of benefit in eyes with submacular hemorrhage associated with idiopathic polypoidal choroidal vasculopathy.
16. Haupert et al. Am J Ophthalmol, 2001.[49]
- 11 eyes with SRH related to ARMD
- PPV, subretinal injection of tPA, fluid gas exchange
- 8 eyes with improvement in final visual acuity
- 8 eyes with postoperative VA>20/200
- SRH recurred in 3 eyes; severe visual loss in 1 eye
- Conclusion: The efficacy of this treatment is controversial and a prospective clinical trial is necessary to compare it with other proposed treatments.
17. Fine, et al. RETINA, 2010. [50]
- 13 eyes, retrospective interventional case series, SRH due to nAMD
- PPV with subretinal tPA (25 ug in 0.1 ml), gas or oil tamponade, greater than 180o retinotomy and cataract extraction in subset of patients.
- Baseline median BCVA and BCVA at 1 month was HM, but improved with each subsequent f/u visits through 12 months post-op.
- 9/15 patients required subsequent procedures (hyphema, vitreous hemorrhage, retinal detachment, glaucoma, cataract and aphakia.
- Conclusion: Surgical intervention for SMH due to nAMD is associated with very modest improvement in BCVA.
SUBMACULAR SURGERY TRIALS
Submacular Surgery Trial: Group B
For complete references for the submacular surgery trials, refer to the reference list at the end of the document.
The SST Group B was designed to answer the question: Does submacular surgery of patients with subfoveal choroidal neovascularization with large areas of bleeding secondary to age-related macular degeneration significantly increase the likelihood of vision stabilization or improvement for two years or longer compared to no surgery?
Design: Randomized clinical trial
- March 1998: NEI agrees to expand to full-scale trial
- Recruitment initiated July 1998 (n=336); recruitment ended Sept 30, 2001.
- 168 patients randomized to surgery arm, 168 patients randomized to observation arm.
- Pilot study patients not included
- Results of the final outcome published in 2004
- Primary outcome: stabilization or improvement in visual acuity 2 years after enrollment (specifically either improvement in visual acuity, no change in visual acuity or a decline in visual acuity of no more than 1 line (7 letters) from baseline in the 24 month period)
- Secondary outcomes: patient perception of quality of life, adverse events, size of area affected by the lesion and treatment.
- Other outcomes: change in contrast threshold, central assessment of opacification and color changes of the lens of the affected.
- Patients followed for 4 years or until death.
Eligibility criteria:
- Age 50 or older.
- Evidence of AMD with CNV.
- Blood accounts for > 50% of the lesion so thick that it was limiting the ophthalmologist’s ability to determine whether the blood-occupied area also contained CNV.
- Blood or CNV (classic or occult) extends through geometric center of FAZ.
- Size of entire lesion (including blood) > 3.5 MPS disc areas.
- Size of all CNV (classic or occult CNV), whenever CNV is apparent, < 9 MPS disc areas.
- > 75% of lesion posterior to equator.
- In all cases, examining ophthalmologist had to be certain that the subretinal hemorrhage was not from other causes such as macroaneurysm.
- Study eye visual acuity 20/100 or worse, but LP or better. Visual acuity in the non-study eye had to be LP or better.
- Previous juxtafoveal or extrafoveal CNV treated with laser was not reason for exclusion in otherwise eligible eyes.
- Use of ASA, warfarin or other systemic medications was not subject for exclusion.
Exclusion Criteria:
- NLP in either eye.
- Previous submacular surgery in study eye.
- Previous vitrectomy in study eye.
- Severe NPDR, PDR, DME or other ocular condition that could affect visual acuity and its assessment in either eye.
- IOP > 30 in either eye.
- Myopic correction > 8 D in phakic eye, or evidence of retinal abnormalities consistent with pathologic myopia.
- CE within past month, or capsulotomy within 3 d.
- Any condition, other than CNV, that could limit visual recovery in the study eye.
- Contraindication to surgery or anesthesia.
- Media opacity limiting ability to judge eligibility.
- Unable to position face-down for 2 days post surgery.
- Inability to maintain follow-up.
- Current participation in another AMD study.
- Inability to undergo FA.
- Age < 50 for AMD arms, age < 18 for idiopathic and POHS arms.
Recruitment:
- Patients recruited to study by SST-certified ophthalmologist
- Only one eye (study eye) was eligible for participation in the trial.
- Random assignments stratified according to the visual acuity in the study eye (better than 20/200 or 20/200 or worse).
- Surgery scheduled as soon as possible, but not more than 8 days after enrollment.
- Baseline visual acuity measurements obtained before randomization, 24 months, at 36 and 48 months.
Surgical Treatment Protocol:
- Goal: To remove entire CNV lesion (classic and occult component, blood, and scar tissue).
- Performed only by the SST approved surgeons.
- Performed within 8 days of randomization.
- FA within 8 days prior to surgery.
- Informed consent.
- Peribulbar, retrobulbar or general anesthesia.
- Standard 3 port PPV.
- Detachment of posterior hyaloid at least beyond major vascular arcades and at the retinotomy site.
- tPA: At the discretion of the surgeon, 10 to 12.5ug of tPA in 0.1 ml may be injected prior to removal of the blood. If a very large clot, more than 0.1 ml may be used. Must wait 40 minutes after tPA for irrigation of liquefied blood. The clot and any associated fibrovascular tissue is mechanically extracted whenever possible based on the judgment of the surgeon. If blood under the RPE, additional 10 to 12.5ug can be used under the RPE and then irrigated 40 minutes after injection. If the mass of blood was to big to remove en- bloc, it was permit for surgeon to cut it into smaller pieces only after reasonable effort was made to remove it as single piece to use for histopathological examination. If more than a thin layer of blood persists, treatment may be repeated.
- If eye had previous laser treatment, removal of the laser scar with the CNV to be attempted. If removal of laser scar to difficult, CNV was dissected and removed from the interface of the scar.
- Use of perfluorocarbons permitted at discretion of the surgeon.
- Endolaser used only if retinotomy was large (ie. more than one disc diameter).
- Air/fluid exchange.
- Up to 50% air bubble in phakic patients, 100% bubble in pseudophakic patients. No perfluorocarbon liquids.
- Patient instructed to keep facedown position overnight and until the air bubble was less than 20%.
Follow-up:
- Eyes treated with surgery were examined as often as deemed necessary by the attending surgeon.
- Patients assigned to observation were scheduled for telephone interview regarding vision status and ocular history one month after enrollment.
- All patients (surgery and observation) had f/u exam for data collection at 3, 6, 12 and 24 months after enrollment w/ either 36 month or 48 month f/u.
- If CNV leakage after enrollment, laser, surgery or photodynamic therapy w/ vaterporfrin for surgery arm and laser and photodynamic therapy for patients in observation arm.
- Cataract surgery for either arms done when it resulted in loss of more than 2 lines of BCVA as judged by examining ophthalmologist.
- Adverse events reported to coordinating center.
Surgery variations/deviations:
- Recombinant tPA injected 38% of eyes, endolaser in 14% eyes, perfluorocarbon in 6% eyes, 15% leaving air bubble >50% and use of gas bubble instead of air bubble 30%.
- Subretinal or sub-RPE blood remained in 93% of eyes and in 9% significant to elevate the retina.
- Intra-op complications 22% eyes with retinal tears, 10% with area judged at risk for retinal tear peripherally, 7% with retinal tears at posterior pole and 1% scleral buckle placement. No intraoperative choroidal hemorrhage.
Results:
- 56 % of surgery eyes vs. 59 % of observation eyes had 2-lines or greater BCVA loss at 24 months f/u.
- 44% of surgery eyes vs.41% of observation eyes had improvement or stabilization of BCVA (p=0.63, Fisher’s exact).
- 18% of surgery eyes and 18% of observation eyes had visual acuity improvement of >2 lines since baseline at 24 months.
- 21% of surgery eyes and 36% of observation eyes had lost more than 6 lines of best corrected visual acuity from baseline (p=0.004, Fisher’s exact).
- No differences in changes of reading speed in surgery vs. observation arm.
- 54% vs. 45% surgery vs. observation in change of threshold contrast sensitivity with median improvement of 1 contrast segment in surgery and no change in observation arm (p=0.01, Wilcoxon rank sum test).
- 44% of eyes initially phakic underwent cataract surgery in surgery arm vs. 6% in the observation arm.
- 16% of eyes in the surgery arm had rhegmatogenous retinal detachment vs. 2% in the observation arm.
Conclusions:
- Submacular surgery as performed in SST group B trial did not confer advantage over observation alone with respect to achieving stable or improved BCVA in AMD patients with CNV and associated submacular hemorrhage.
- Submacular surgery as performed in SST group B trial did result in lesser incidence of severe vision loss (as defined by loss of more than 6 lines of BCVA) compared to observation alone. These findings however, were not accompanied by changes in VT health-related quality of life findings.
- Submacular surgery as performed in SST group B trial did result in significantly higher rate of rhegmatogenous retinal detachments and necessitated significantly higher rates of cataract surgery.
Macular translocation and RPE transplant surgery
1. Machemer R, Steinhorst UH, Graefes Arch Clin Exp Ophthalmol. 1993.[21]
- 3 patients with severe massive SRH related to ARMD
- PPV followed by subretinal fluid infusion to create RD, followed by circumferential retinotomy.
- Retina was rotated and fovea relocated with rotations between 30 and 80 degrees.
- One pt with VA improvement 1/200 to 20/80; other pts developed vitreoproliferative retinopathy.
- Conclusion: Macular translocation surgery may be an option for severe SRH.
2. Wong D, et al, Br J Ophthalmol. 2004.[51]
- 29 patients with severe SMH related to nAMD, prospective, non-comparative, interventional study.
- Phacoemulsification, vitrectomy, 360 degrees retinotomy, excision of choroidal neovascular membrane, and macular relocation using an infusion of 5-fluorouracil and low molecular weight heparin.
- Preoperative visual acuity (20/120 or worse) and lesion type (predominantly classic or submacular haemorrhage) were significantly associated with visual improvement (coefficient of regression B = 26.8, p<0.001 and B = 14.9 with p = 0.045 respectively).
- Conclusion: Macular translocation may achieve VA improvement in select cases with submacular hemorrhage.
3. Gibran SK, et al, Graefes Arch Clin Exp Ophthalmol. 2009. [52]
- 4 patients, retrospective case series, SMH related to nAMD.
- Patients underwent PPV, induced RD, peripheral temporal retinotomy, removal of SMH and CNV complex. Full thickness chorio-RPE patch was grafted on the site. Silicon oil endotamponade for 12 weeks followed by average 6 month follow-up.
- SMH removed in all cases; RPE patch graft sufficient to cover macular RPE defect in all cases; at last f/u mean VA improvement 3 +/- 0.9 to 55 +/- 9 ETDRS letters and recovery of central fixation observed in all patients.
- Conclusion: Surgical evacuation of SMH due to nAMD with RPE patch grafting may be a beneficial option in select group of patients.
4. Ma Z, et al. IOVS, 2009. [53]
- 21 patients, retrospective case series, SMH related to nAMD.
- PPV, semicircular temporal peripheral retinotomy, injection of saline into subretinal space, CNV debriedement and evacuation of subretinal blood, RPE-Bruch’s membrane graft performed from mid-peripheral retina followed by silicon oil tamponade.
- Mean f/u of 20 months. At last f/u mean ETDRS scores increased from 28.65 ± 23.99 before surgery to 47.76 ± 17.22 after surgery.
- Among 21 eyes, proliferative vitreoretinopathy (PVR) occurred in 3 (14.29%), and a recurrent neovascular membrane was observed in one eye (4.76%).
- Conclusion: Transplantation of the autologous RPE–Bruch’s membrane complex can increase the visual acuity of patients with hemorrhagic AMD.
5. MacLaren RE, et al. Ophthalmology. 2007. [54]
- 12 patients, interventional prospective cohort study, SMH related to nAMD
- Submacular removal of CNV through a single retinotomy followed by a full-thickness patch graft of RPE, Bruch's membrane, and choroid harvested from the superior equatorial retina and transplanted into the subfoveal space. Graft flattened with heavy liquid followed by silicone oil exchange.
- Removal of silicone oil and cataract surgery at 3 months.
- Successful viable grafts observed in 11/12 patients; The mean visual acuity over the whole cohort fell from logMAR 0.82 to 1.16.
- Operative complications occurred in 8 patients, including retinal detachment in 5 patients and hemorrhage affecting the graft in 4 patients.
- Conclusion: RPE transplantation may be effective in restoring vision in nAMD, but operative complications remain high.
6. Tezel, TH, et al, Am. J. Ophthal. 2007. [55]
- 12 patients, interventional case series, CNV related to nAMD
- Pts underwent subfoveal membranectomy with transplantation of a sheet of adult human allogeneic RPE cells with mean f/u of 1 year.
- Eligibility criteria: age >60, BCVA < or =20/63 and subfoveal neovascularization < or =9 disk areas on preoperative fluorescein angiography. All patients on triple immunosuppression post-op.
- BCVA (P = .085), contrast sensitivity (P = .204), and the reading speed (P = .077) not changed significantly at one year compared with pre- values. Transplants no signs of rejection.
- Post-op complications: cataract progression requiring surgery (three of eight phakic eyes), retinal detachment (three eyes), intraoperative retinal breaks (two eyes), and macular pucker (two eyes); no CSME observed.
- Conclusion: Adult human allogeneic RPE transplant into the subretinal space in AMD patients is possible at the time of subfoveal membranectomy. Systemic immune suppression prevents rejection, but does not lead to an improvement in BCVA.
7. Stanga PE, et al. Ophthalmology. 2002. [56]
- 9 patients, Retrospective, noncomparative, interventional case series, CNV related to nAMD.
- Pts underwent surgical excision of the subfoveal CNV with RPE translocation and were observed for 12 to 32 months. Surgery involved standard three-port pars plana vitrectomy, excision of the CNV, and RPE translocation.
- RPE translocated successfully at the time of CNV removal from the edge of the RPE defect to a subfoveal location in seven of nine patients. One patient experienced proliferative vitreoretinopathy, Confocal laser scanning ophthalmoscopy showed autofluorescence of the translocated RPE.
- Conclusion: RPE translocation from the edge of the lesion at the time of CNV removal has a role in surgical management of nAMD.
8. Binder S, et al. IOVS. 2004. [57]
- 53 eyes, prospective consecutive case series, CNV related to nAMD.
- Pts with fCNV who were not eligible for laser or photodynamic therapy underwent subretinal membrane excision with simultaneous transplantation of autologous RPE cells.
- Grp 1—pts underwent subfoveal membranectomy and RPE transplantation. Grp 2—pts underwent subfoveal membranectomy alone.
- In Grp 1, the BCVA improved by at least two lines in 53.8% of patients, compared to 21.1% pts in Grp 2. Reading acuity was significantly higher in Grp 1 related to Grp 2. mfERG response density changes were significantly different between groups 1 and 2.
- Conclusion: Pts undergoing fCNV removal with autologous transplantation of RPE achieved significantly better reading acuity and higher mfERG-response density than control pts. Autologous RPE transplantation should be considered in pts undergoing fCNV excision.
Photodynamic therapy
1. Rouvas, et al. Retina. 2010. [58]
- 30 eyes of 30 patients, retrospective comparative study, SMH related to polypoidal choroidal vasculopathy.
- Patients either received 1 session of PDT or 3 monthly intravitreal injections of 0.5 mg ranibizumab or 1 session of PDT and 3 injections of 0.5 mg ranibizumab.
- Retreatment in each group done in case of leaking polyps on the indocyanine green angiography or persistence or recurrence of subretinal fluid, intraretinal fluid, and/or hemorrhages.
- BCVA improvement noted in PDT alone group, whereas VA stabilized in RZB alone or PDT plus RZB groups.
- 45.45% of the patients treated with PDT alone gained more than 3 lines, whereas no patient in RZB alone or PDT plus RZB groups.
- Conclusion: PDT resulted in a significantly better outcome at the end of the follow-up, whereas pts receiving RZB or PDT plus RZB had stabilization of the disease.
2. Ahmad, S, et al. Am J Ophthalmol. 2008.[59]
- 21 patients with nAMD with predominately hemorrhagic CNV.
- Mean pretreatment VA was 20/210, and mean SRH size was 16 disk areas.
- All patients treated with photodynamic therapy (PDT)
- Thirteen (62%) of 21 eyes exhibited stable or improved VA; SRH resolved in 18 eyes (86%) after a mean of six months.
- VA one year after PDT inversely correlated with patient age (P = .045) and initial SRH size (P = .04) and positively correlated with pretreatment VA (P = .01).
- Conclusion: PDT may be effective for SMH related to nAMD in select group of patients; further studies needed to clarify efficacy of PDT compared to other treatment approaches.
3. Chan, et al, Clin. Experiment. Ophthalmol. 2005. [60]
- Six eyes of six patients, prospective, non-comparative, interventional case series; thick SMH secondary to polypoidal choroidal vasculopathy. which was displaced pneumatically with intravitreal pure 0.4 ml C(3)F(8) and subsequently with PDT for any persistent active leaking polypoidal lesions
- The mean improvement in logMAR BCVA after the sequential treatments was seven lines (range +3 to +19 lines) All patients had at least moderate visual gains.
- No patient suffered serious complications from PDT.
- Conclusion: Intravitreal gas injection and sequential PDT for PCV seems to be a well-tolerated option; further studies needed.
Pneumatic Displacement
1. Heriot, Pre-AAO meeting, Chicago, IL, 1996.[61]
- 10 patients with SMH secondary to AMD (8), RAMA (2)
- Treated with 100ug/0.1ml intravitreal tPA
- 0.3 ml C3F8 gas bubble, face down positioning to displace blood from fovea.
- Displacement of blood from fovea.
- Final VA not reported for all cases.
- Complications: RRD in 1 of 16 patients treated this way.
- Conclusion: Treatment with intravitreal tPA and pneumatic displacement may result in better VA.
2. Ohji et al., Arch Ophthalmol, 1998.[62]
- 5 patients with SMH secondary to AMD (4), RAMA (1)
- Treated with 0.4-0.5 ml pure perfluoropropane gas bubble, face down positioning to displace hemorrhage from fovea.
- No TPA used
- 3 patients with dramatic displacement of blood, 2 with thinning
- Final VA 20/15 to 20/200; > 20/50 in 3 eyes
- Complications VH (1), RD (1)
- Conclusion: Gas bubble displaces blood from macula without TPA, may have improved VA.
3. Hassan et al., Ophthalmology, 1999. [63]
- 15 patients with acute (< 3 wk) thick SMH secondary to ARMD (13), RAMA (1), trauma (1) treated with intravitreal tPA (25-100 ug/ 0.1-0.2 ml) and gas tamponade (C3F8 or SF6) with face-down positioning for 1-5 days.
- All had complete displacement of blood from fovea
- Post-op VA improved by > 2 lines in 14 (93%), final VA improved in 10 (67%) and was > 20/80 in 40%
- Complications: VH in 3, endophthalmitis in 1, recurrent SRH in 4
- Conclusion: This technique effective in displacing SRH and improving VA in most patients, final VA limited by progression of underlying disease.
4. Handwerger et al., Arch Ophthalmol, 2001.[64]
- 14 patients, retrospective, SRH secondary to ARMD
- SRH was completely displaced from the fovea in 10 patients
- 8 patients with improvement of 2 lines in postoperative VA (57%)
- Conclusion: Safe and effective in displacing submacular hemorrhage.
5. Holland D, et al, Ophthalmologica, 2004. [65]
- 2 patients, case report, SMH due to traumatic choroidal rupture
- IV injection of 0.4 ml of sulfur hexafluoride; in 1 patient gas injection combined with 50 mcg of rtPA.
- Vision improved from 20/125 and 20/100 to 20/32 in both eyes.
- Conclusion: IV r-TPA and gas efficient therapy for patients with SMH due to choroidal rupture.
6. Wu TT, et al, J. Ocul Pharmacol Ther. 2005. [66]
- 6 patients, retrospective case series, SMH related to retinal arterial macroaneurysm
- IV tPA 50 mcg/0.1 ml injected through pars plana into vitreous cavity with 0.3-0.5 ml perfluoropropane gas following the tPA injection.
- Post-op visual acuity improved in 83% of eyes and unchanged in 17 % of eyes; in 83% of eyes SMH was either completely or partially displaced.
- Conclusion: IV tPA and gas followed by prone positioning is effective treatment for SMH due to retinal arterial aneurysm.
7. Yang PM, et al Chang Gung Med J. 2005. [67]
- 24 patients, retrospective case series, dense SMH
- Pts w/ SMH treated with IV expansile gas with or without IV tPA injection to displace submacular blood.
- Total or partial blood displacement achieved in all eyes. With mean f/u of 15.5 months, final VA improved by 2 or more lines in 45.8% of patients and measured 20/100 or better in 41.7% of eyes.
- Conclusion: Pneumatic displacement, with or without IV tPA useful in displacing dense SMH and facilitating visual improvement, although the visual outcome often limited by the progression of the underlying macular disease.
8. Gopalakrishan M, Retina 2007. [68]
- 20 patients, prospective, consecutive, single-center, noncomparative, interventional case series, SMH due to various etiologies.
- Pts tx w/ IV perfluoropropane followed by prone position for 5 days to 7 days. Pts f/u 1d, 7d, 1 month, 3 months, 6 months and 1 year.
- Submacular blood completely or partially displaced from fovea in 16/20 eyes within 7 days of IV injection.
- Mean BCVA improved from 1.6 to 0.72 logarithm of minimum angle of resolution; Final visual acuity was 20/63 or better in 10 eyes (50%); four pts developed non-resolving VH, rx. by PPV.
- Conclusion: IV perfluoropropane gas is effective at pneumatic resolution of SMH without tPA.
9. Ron Y, Ophthalmologica. 2007. [69]
- 24 patients, retrospective chart review, SMH secondary to AMD
- IV injections of perfluoropropane gas (11 patients) or sulfurhexafluoride (13 patients) reviewed for VA at baseline and after IV injection.
- Overall improvement in VA statistically significant for SF(6) group (p=0.034), but not for C(3)F(8) group (p=0.245).
- Conclusion: Use of gas for pneumatic displacement of SMH can improve VA.
10. Fang IM, Eye, 2009. [70]
- 53 eyes from 53 patients, retrospective chart review, thick subfoveal hemorrhage due to nAMD.
- 0.84+/-0.03 (n=112); at 3 months was 0.69+/-0.05 (P<0.0001, n=84); at 6 months was 0.74+/-0.06 (P<0.05, n=51); and at 9 months was 0.69+/-0.08 (n=29, P=0.09).
- 28 eyes received IV t-PA and gas injection and 25 eyes received IV gas injection alone. BCVA outcome compared between t-PA+gas vs. gas alone.
- Best post-op visual acuity improvement significantly higher in the t-PA + gas group than in the gas-alone (60.7 vs 32.0%; P=0.037); difference significant only in eyes with hemorrhage duration >14 days (46.2 vs 8.3%; P=0.035). Incidence of final visual acuity improvement was not significantly different between the two groups (42.9 vs 28.0%; P=0.39).
- Complications of vitreous hemorrhage and endophthalmitis were the same between the two groups.
- Conclusions: IV t-PA valuable only in eyes with old hemorrhage; for recent onset hemorrhage, tPA recommended only if IV gas failed to displace SMH.
11. Nourinia R et al. J Ophthalmic Vis Res. 2010
- Intravitreal expansile gas injection + rtPA vs Intravitreal expansil gas alone followed by intravitreal Bevacizumab injection for treatment of SMH secondary to AMD.
- 5 eyes of 5 patients. 3 eyes with gas (0.3 ml pure SF6) vs 2 eyes with pure SF6 + 50 µg/0.05ml) rtPA. Face-down positionning. After 24 hours: 1.25 mg/0.05ml Bevacizumab intravitreous injection.
- duration of symptoms (mean 6.4+3.2 , range 3-10) days. Mean number of Bevacizumab injection:1.8 (range 1-3). BCVA improved significantly at 12 months. SMH displacement in all eyes.
- Conclusion Expansible SF6 with or without rtPA followed by bevacizumab injections seems to result in improved BCVA in SMH secondary to AMD.
13. Kitahashi M,Clin Ophthalmol. 2014
- Pneumatic displacement (PD) + IVT bevacizumab (IVB) vs pneumatic displacement alone for massive submacular hemorraghe (SMH) in polyoidal choroidal vasculopathy(PCV).
- 32 eyes from 32 patients. 22 eyes in the PD+IVB 1.25mg group and 10 eyes in the PD alone group.
- Complete displacement from under the fovea: 86.4% in the PD+IVB group vs 50% in the PD alone group.
- Best Corrected VA at 0, 3, 6 months significantly better in PD+IVB group.
- Improvement in Best Corrected VA >0.3logMAR in 81.8% for PD+IVB group and 20% in PD group.
- Fewer additionnal treatment in PD+IVB group vs PD alone group. Significant.
- Better procedure for massive SMH due to PCV
Treatement of SMH by pneumatic displacement + rtPA with or without Anti-VEGF
1. Chang W, Am J Ophthalmol. 2014
101 eyes of 101 patients with AMD and SMH. PPV +gas + AntiVEGF vs PPV+gas alone. Greater visual acuity improvement in the group with anti-VEGF at 6 months.
Complication: Vitreous haemorrhage (2 eyes). rhegmatogenous retinal detachment (4 eyes), recurrent hemorrhage (6 eyes).
Conclusions: PPV+Gas+rtPA effective for retinal displacement. There is a loss of acuity over time. Anti-VEGF injection help maintain visual acuity.
Anti-VEGF Agents in treatment of SMH with or without pneumatic displacement
1. Olmos, et al. Ophthalmology Management. 2010. [71]
- 4 patients, retrospective case series, SRH related to nAMD.
- Patients treated with serial intravitreal injections of ranibizumab.
- SRH hemorrhage resolved over the course of 4 to 8 months.
- Baseline BCVA was 20/60 or worse (20/60 to 20/400), final BCVA between 20/25 and 20/40.
- Conclusion: SMH of varying size and thickness can be successfully treated with intravitreal lucentis monotherapy.
2. Chang, et al. Retina. 2010. [72]
- 7 patients, prospective one year case series, SRH secondary to nAMD.
- SRHs due to CNV treated w/ IV injections of ranibizumab (RZB) at baseline, 1 month and 2 months. Subsequent monthly injections through month 11 given at the discretion of attending ophthalmologist with maximal 12 injections given.
- At 12 months median visual acuity was 20/250 with median change in +7 letters; 3/7 pts improved more than 2 lines of vision and no patient lost more than 2 lines. Median change in subfield thickness in OCT from baseline was -109 microns.
- No ocular or systemic adverse effects observed.
- Conclusion: Hemorrhagic CNV in nAMD treated with IV injections of RZB alone have better VA outcome than natural history of controls in SST trials.
3. Sandhu, et al, Clin Ophthalmol. 2010. [73]
- 16 patients, retrospective, SRH secondary to neovascular AMD (nAMD).
- SRH treated by 25G vitrectomy, submacular tPA injection (12.5 ug/o.1 mL), pneumatic displacement with fluid air exchange followed by post-op IV ranibizumab (RZB)
- 68.7% patients with complete displacement of SMH.
- All pts had improvement of at least 1 line VA at 6 months; with 63% of patients improving by more than two lines and 83% of patients treated with RZB improving by 83%.
- Conclusion: Vitrectomy/tPA/pneumatic displacement of SRH followed by RZB injection can stabilize/improve vision in patients with nAMD.
4. Ferraz, et al, Arq Bras Oftalmol. 2010. [74]
- 5 study eyes, retrospective case series, SRH secondary to AMD.
- SRH treated with concurrent intravitreal injection of bevacizumab and C3F8 followed by prone positioning of patients.
- The full displacement achieved in 4/5 patients.
- Mean pre-op VA 1.12 +/- 0.34 logMAR and the mean postoperative VA was 0.92 +/- 0.4 logMAR.
- No post-op complications of retinal detachment, endophthalmitis, vitreous hemorrhage, uveitis, cataracts and increased intraocular pressure during f/u.
- Conclusion: IV bevacizumab and C3F8 may be a viable strategy for tx. SMH in AMD pts.
5. Matt, et al, Klin Monbl Augenheilkd. 2010 (German).[75]
- 10 study eyes, retrospective clinical study, SRH secondary to nAMD.
- Extensive subfoveal hemorrhages treated with IV rtPA (0.05 mL; 0.025 mg/0.1 mL in 0.9% NaCl), 100% sulphur hexafluoride (SF(6)) gas (0.5 mL) and lucentis (0.05 mL, 10 mg/mL) within two weeks after the onset of the subretinal hemorrhage. Re-injections with lucentis done q 4 week if persistent subfoveal hemorrhage or CNV.
- After 3-13 months of f/u, VA increased in 7/10, stable in 1/10 and decreased 2/10 patients.
- Complications CRAO (1/10 pts), corneal erosion (1/10 pts) and increased IOP (1/10).
- Conclusion: Combination of rtPA, gas and lucentis effective therapy for extensive subfoveal hemorrhage in nAMD.
6. Arias, et al., Clinical Ophthalmol. 2010. [76]
- 15 study eyes, retrospective consecutive case series, SRH due to nAMD
- Acute hemorrhagic nAMD presenting with central scotoma and/or VA loss treated with 25- or 23-gauge TSV, subretinal or intravitreal tPA, fluid-air-SF6 exchange and intravitreal injection of bevacizumab
- Successful displacement of SMH in all cases. Average age close to 80, baseline average VA of 20/640 increased to 20/250. Complications: VH, RPE tear.
- Conclusion: Surgical approach with 25- or 23-gauge TSV, subretinal or intravitreal tPA, fluid-air-SF6 exchange and intravitreal injection of bevacizumab is safe and effective for early treatment of hemorrhagic AMD.
7. Auriol, et al, J. Fr. Ophthalmol. 2010. [77]
- 18 study eyes in 16 patients, retrospective clinical case series, SRH due to nAMD.
- Thick SMH treated with vitrectomy, subretinal injection of rtPA (0.5mg), and fluid-gas exchange.
- Thick SRH displaced in all cases, CNV causing bleed identified in 10/18 eyes, all of which received adjuvant photodynamic therapy or intravitreal injections. Complications- one case of RD and one case of hyphema.
- Conclusion: Submacular surgery with adjuvant interventions useful in treatment of thick SMH.
8. Treumer, et al, Br. J. Ophthalmol. 2009. [78]
- 12 patients, retrospective case series, SMH in nAMD.
- All patients underwent PPV with subretinal co-application of rtPA and bevacizumab, and fluid-gas (20% SF6) exchange. All phakic pts underwent cataract surgery; additional IV injections of bevacizumab at 4 and 8 weeks post-op.
- Complete SMH displacement in 9/12 pts. BCVA improved from baseline logMAR 1.9 to logMAR 1.2 (4 weeks) and logMAR 0.9 (12 weeks post-op). Improvement observed in 10 pts, stable VA in one and decreased VA in one patient.
- Conclusion: PPV with co-application of tPA and bevacizumab with fluid gas exchange effectively displaces SMH and improves VA.
9. Höhn F, et al. Ophthalmologe, 2010. [79]
- 10 patients, retrospective case series, subfoveal hemorrhage in nAMD.
- Pts received IV injections of 1.25 mg bevacizumab and 0.3 ml SF(6) with a 4 week f/u at which additional anti-VEGF IV injections were performed.
- Displacement of SFH in 80%; VA improved by 3 or more lines in 60% of pts, remained stable in 30% of pts and worsened in 10% of pts.
- Conclusion: Combined IV injections of bevacizumab and SF(6) have potential efficacy to improve VA in patients with SRH due to nAMD.
10. Shah, SP. Ophthalmic Surg Lasers Imaging. 2009. [80]
- Two patients, case report, massive SMH due to nAMD.
- Pts underwent combination PPV, submacular anti-VEGF and r-TPA injection with pneumatic displacement of the hemorrhage. VA at 7 and 8 month post-op visits were 20/80 and 20/70(-1), respectively.
- Conclusion: PPV with submacular anti-VEGF and r-TPA injection with pneumatic displacement viable option for tx SMH.
11. Chawla, Ind. J. Ophthalmol. 2009.[81]
- Four patients, case report, SMH due to choroidal neovascular membrane (? Due to AMD)
- 4 patients underwent IV injection of 0.05 ml bevacizumab w/ 0.5 ml of SF6 for pneumatic displacement.
- Complete or partial displacement of SMH observed in all 4 cases
In three patients, VA improved at 3 months to (20/120, 20/40 and 20/60; one patient lost to follow-up).
- Conclusion: Pneumatic displacement with IV bevacizumab effective for treatment of SMH.
12. Stifter E. Am. J. Ophthalmol. 2007. [82]
- 21 eyes of 19 patients, retrospective clinical study, nAMD.
- Patients with SMH involving fovea and more than 50% of the lesion injected with IV bevacizumab.
- At 4 months, VA stable or improved in 100% of patients, and in 9.5% improved by at least 3 lines. Similar results at 12 months f/u.
- Significant improvements in central foveal thickness, maximum retinal thickness, minimum retinal thickness and foveal volume with mean size of hemorrhage significantly decreased.
- Conclusion: IV bevacizumab good option for patients w/ nAMD and large SMH with good anatomic and VA outcomes.
13. Cleary CA, et al. Eye. 2008. [83]
- 112 eyes of 111 patients, Interventional consecutive retrospective case series, CNV membranes, PEDs, and SMHs related to nAMD.
- Pts received IV bevacizumab w/ f/u including VA, ophthalmic exams, OCT and FA. Repeat injections for persistent leakage and retinal edema.
- Mean f/u of 5 months with VA of 0.84+/-0.03 (n=112) at baseline; 0.69+/-0.05 (P<0.0001, n=84) at 3 months; 0.74+/-0.06 (P<0.05, n=51) at 6 months; 0.69+/-0.08 (n=29, P=0.09) at 9 months. Only 17 patients received single injection, and 13/17 maintained or improved VA at 6 months. There was steady decrease in mean foveal thickness from baseline through 6 months f/u
- Conclusion: IV bevacizumab is effective treatment for nAMD.
14. Meyer CH, et al, Acta Ophthalmol. 2008. [84]
- 19 patients, retrospective pilot study, SRH related to nAMD.
- Each patient underwent triple procedure with intravitreal injection 0.05 ml rtPA (50 microg), 0.3 ml of sulphur hexafluoride (SF6) gas and 0.05 ml bevacizumab.
- Lesion size, SRH location and ETDRS visual acuity at baseline, 1 and 3 months after the injection.
- Baseline VA of 20/133 improved to 20/86 at 1 month and to 20/74 at 3 months. Successful inferior displacement of the SRH in 17/19 pts.
- Conclusion: IV rtPA, gas and bevacizumab appears to be beneficial and well tolerated in the treatment of SRH in the short term.
Table Summary
References
- ↑ Glatt H, Machemer R. Experimental subretinal hemorrhage in rabbits. Am J Ophthalmol. 1982 Dec;94(6):762-73.
- ↑ Toth CA, Morse LS, Hjelmeland LM, Landers MB 3rd. Fibrin Directs Early Retinal Damage After Experimental Subretinal Hemorrhage. Arch Ophthalmol. 1991 May;109(5):723-9.
- ↑ Bloome MA, Ruiz RS. Massive spontaneous subretinal hemorrhage. Am J Ophthalmol. 1978 Nov;86(5):630-7. PubMed PMID: 717519.
- ↑ Gillies A, Lahav M. Absorption of retinal and subretinal hemorrhages. Ann Ophthalmol. 1983 Nov;15(11):1068-74.
- ↑ Nasrallah F, Jalkh AE, Trempe CL, McMeel JW, Schepens CL. Subretinal hemorrhage in atrophic age-related macular degeneration. Am J Ophthalmol. 1989 Jan 15;107(1):38-41.
- ↑ Bennett SR, Folk JC, Blodi CF, Klugman M. Factors prognostic of visual outcome in patients with subretinal hemorrhage. Am J Ophthalmol. 1990 Jan 15;109(1):33-7.
- ↑ Hayasaka S, Uchida M, Setogawa T. Subretinal hemorrhages with or without choroidal neovascularization in the maculas of patients with pathologic myopia. Graefes Arch Clin Exp Ophthalmol. 1990;228(4):277-80.
- ↑ Avery RL, Fekrat S, Hawkins BS, Bressler NM. Natural history of subfoveal subretinal hemorrhage in age-related macular degeneration. Retina. 1996;16(3):183-9.
- ↑ Berrocal MH, Lewis ML, Flynn HW Jr. Variations in the clinical course of submacular hemorrhage. Am J Ophthalmol. 1996 Oct;122(4):486-93. Erratum in: Am J Ophthalmol 1996 Dec;122(6):920.
- ↑ Morse LS, Chapman CB, Eliott D, Benner JD, Blumenkranz MS, McCuen BW 2nd. Subretinal hemorrhages in proliferative diabetic retinopathy. Retina. 1997;17(2):87-93.
- ↑ Scupola A, Coscas G, Soubrane G, Balestrazzi E. Natural history of macular subretinal hemorrhage in age-related macular degeneration. Ophthalmologica. 1999;213(2):97-102.
- ↑ Uyama M, Matsubara T, Fukushima I, Matsunaga H, Iwashita K, Nagai Y, Takahashi K. Idiopathic polypoidal choroidal vasculopathy in Japanese patients. Arch Ophthalmol. 1999 Aug;117(8):1035-42.
- ↑ McCabe CM, Flynn HW Jr, McLean WC, Brod RD, McDonald HR, Johnson MW, Williams GA, Mieler WF. Nonsurgical management of macular hemorrhage secondary to retinal artery macroaneurysms. Arch Ophthalmol. 2000 Jun;118(6):780-5.
- ↑ Dellaporta A. Endodiathermy for retinal detachment with macular hole. Am J Ophthalmol. 1983 Mar;95(3):405-7.
- ↑ Hanscom TA, Diddie KR. Early surgical drainage of macular subretinal hemorrhage. Arch Ophthalmol. 1987 Dec;105(12):1722-3.
- ↑ de Juan E Jr, Machemer R. Vitreous surgery for hemorrhagic and fibrous complications of age-related macular degeneration. Am J Ophthalmol. 1988 Jan 15;105(1):25-9.
- ↑ Han DP, Mieler WF, Schwartz DM, Abrams GW. Management of traumatic hemorrhagic retinal detachment with pars plana vitrectomy. Arch Ophthalmol. 1990 Sep;108(9):1281-6.
- ↑ Wade EC, Flynn HW Jr, Olsen KR, Blumenkranz MS, Nicholson DH. Subretinal hemorrhage management by pars plana vitrectomy and internal drainage. Arch Ophthalmol. 1990 Jul;108(7):973-8.
- ↑ Vander JF, Federman JL, Greven C, Slusher MM, Gabel VP. Surgical removal of massive subretinal hemorrhage associated with age-related macular degeneration. Ophthalmology. 1991 Jan;98(1):23-7.
- ↑ Mandelcorn MS, Menezes AV. Surgical removal of subretinal hemorrhage and choroidal neovascular membranes in acute hemorrhagic age-related macular degeneration. Can J Ophthalmol. 1993 Feb;28(1):19-23.
- ↑ Jump up to: 21.0 21.1 Machemer R, Steinhorst UH. Retinal separation, retinotomy, and macular relocation: II. A surgical approach for age-related macular degeneration? Graefes Arch Clin Exp Ophthalmol. 1993 Nov;231(11):635-41.
- ↑ Rubsamen PE, Flynn HW Jr, Civantos JM, Smiddy WE, Murray TG, Nicholson DH, Blumenkranz MS. Treatment of massive subretinal hemorrhage from complications of scleral buckling procedures. Am J Ophthalmol. 1994 Sep 15;118(3):299-303.
- ↑ Ibanez HE, Williams DF, Thomas MA, Ruby AJ, Meredith TA, Boniuk I, Grand MG. Surgical management of submacular hemorrhage. A series of 47 consecutive cases. Arch Ophthalmol. 1995 Jan;113(1):62-9.
- ↑ Johnson MW, Olsen KR, Hernandez E, Irvine WD, Johnson RN. Retinal toxicity of recombinant tissue plasminogen activator in the rabbit. Arch Ophthalmol. 1990 Feb;108(2):259-63.
- ↑ Lewis H, Resnick SC, Flannery JG, Straatsma BR. Tissue plasminogen activator treatment of experimental subretinal hemorrhage. Am J Ophthalmol. 1991 Feb 15;111(2):197-204.
- ↑ Benner JD, Morse LS, Toth CA, Landers MB 3rd, Hjelmeland LM. Evaluation of a commercial recombinant tissue-type plasminogen activator preparation in the subretinal space of the cat. Arch Ophthalmol. 1991 Dec;109(12):1731-6.
- ↑ Toth CA, Benner JD, Hjelmeland LM, Landers MB 3rd, Morse LS. Ultramicrosurgical removal of subretinal hemorrhage in cats. Am J Ophthalmol. 1992 Feb 15;113(2):175-82.
- ↑ Johnson MW, Olsen KR, Hernandez E. Tissue plasminogen activator thrombolysis during surgical evacuation of experimental subretinal hemorrhage. Ophthalmology. 1992 Apr;99(4):515-21.
- ↑ Coll GE, Sparrow JR, Marinovic A, Chang S. Effect of intravitreal tissue plasminogen activator on experimental subretinal hemorrhage. Retina. 1995;15(4):319-26.
- ↑ Benner JD, Hay A, Landers MB 3rd, Hjelmeland LM, Morse LS. Fibrinolytic-assisted removal of experimental subretinal hemorrhage within seven days reduces outer retinal degeneration. Ophthalmology. 1994 Apr;101(4):672-81.
- ↑ Morse LS, Benner JD, Hjelmeland LM, Landers MB 3rd. Fibrinolysis of experimental subretinal haemorrhage without removal using tissue plasminogen activator. Br J Ophthalmol. 1996 Jul;80(7):658-62.
- ↑ Boone DE, Boldt HC, Ross RD, Folk JC, Kimura AE. The use of intravitreal tissue plasminogen activator in the treatment of experimental subretinal hemorrhage in the pig model. Retina. 1996;16(6):518-24.
- ↑ Kamei M, Misono K, Lewis H. A study of the ability of tissue plasminogen activator to diffuse into the subretinal space after intravitreal injection in rabbits. Am J Ophthalmol. 1999 Dec;128(6):739-46.
- ↑ Peyman GA, Nelson NC Jr, Alturki W, Blinder KJ, Paris CL, Desai UR, Harper CA 3rd. Tissue plasminogen activating factor assisted removal of subretinal hemorrhage. Ophthalmic Surg. 1991 Oct;22(10):575-82.
- ↑ Vander JF. Tissue plasminogen activator irrigation to facilitate removal of subretinal hemorrhage during vitrectomy. Ophthalmic Surg. 1992 May;23(5):361-3.
- ↑ Kimura AE, Reddy CV, Folk JC, Farmer SG. Removal of subretinal hemorrhage facilitated by preoperative intravitreal tissue plasminogen activator. Retina. 1994;14(1):83-4.
- ↑ Lewis H. Intraoperative fibrinolysis of submacular hemorrhage with tissue plasminogen activator and surgical drainage. Am J Ophthalmol. 1994 Nov 15;118(5):559-68.
- ↑ Millsap CM, Peyman GA, Greve MD. Subretinal hemorrhage removal with multiple retinotomy sites in age-related macular degeneration. Ophthalmic Surg. 1994 Nov-Dec;25(10):723-5.
- ↑ Laatikainen L, Mattila J. Tissue plasminogen activator (tPA) to facilitate removal of post-traumatic submacular haemorrhage. Acta Ophthalmol Scand. 1995 Aug;73(4):361-2.
- ↑ Lim JI, Drews-Botsch C, Sternberg P Jr, Capone A Jr, Aaberg TM Sr. Submacular hemorrhage removal. Ophthalmology. 1995 Sep;102(9):1393-9.
- ↑ Moriarty AP, McAllister IL, Constable IJ. Initial clinical experience with tissue plasminogen activator (tPA) assisted removal of submacular haemorrhage. Eye (Lond). 1995;9 (Pt 5):582-8.
- ↑ Kamei M, Tano Y, Maeno T, Ikuno Y, Mitsuda H, Yuasa T. Surgical removal of submacular hemorrhage using tissue plasminogen activator and perfluorocarbon liquid. Am J Ophthalmol. 1996 Mar;121(3):267-75.
- ↑ Terasaki H, Miyake Y, Kondo M, Tanikawa A. Focal macular electroretinogram before and after drainage of macular subretinal hemorrhage. Am J Ophthalmol. 1997 Feb;123(2):207-11.
- ↑ Hesse et al. Ger J. Ophthalmol, 1997.
- ↑ Steinhorst UH, Theischen M, Winter R. Subretinal lavage: a technique of continuous subretinal irrigation for removal of traumatic submacular hemorrhage. Ophthalmologica. 1997;211(6):399-401.
- ↑ Humayun M, Lewis H, Flynn HW Jr, Sternberg P Jr, Blumenkranz MS. Management of submacular hemorrhage associated with retinal arterial macroaneurysms. Am J Ophthalmol. 1998 Sep;126(3):358-61.
- ↑ Chaudhry NA, Mieler WF, Han DP, Alfaro VD 3rd, Liggett PE. Preoperative use of tissue plasminogen activator for large submacular hemorrhage. Ophthalmic Surg Lasers. 1999 Mar;30(3):176-80.
- ↑ Shiraga F, Matsuo T, Yokoe S, Takasu I, Okanouchi T, Ohtsuki H, Grossniklaus HE. Surgical treatment of submacular hemorrhage associated with idiopathic polypoidal choroidal vasculopathy. Am J Ophthalmol. 1999 Aug;128(2):147-54.
- ↑ Haupert CL, McCuen BW 2nd, Jaffe GJ, Steuer ER, Cox TA, Toth CA, Fekrat S, Postel EA. Pars plana vitrectomy, subretinal injection of tissue plasminogen activator, and fluid-gas exchange for displacement of thick submacular hemorrhage in age-related macular degeneration. Am J Ophthalmol. 2001 Feb;131(2):208-15.
- ↑ Fine HF, Iranmanesh R, Del Priore LV, Barile GR, Chang LK, Chang S, Schiff WM. Surgical outcomes after massive subretinal hemorrhage secondary to age-related macular degeneration. Retina. 2010 Nov-Dec;30(10):1588-94.
- ↑ Wong D, Stanga P, Briggs M, Lenfestey P, Lancaster E, Li KK, Lim KS and Groenewald C. Case selection in macular relocation surgery for age related macular degeneration. Br. J. Ophthalmol. 2004: 88: 186-90.
- ↑ Gibran SK, Romano MR, Wong D. Perfluorocarbon liquid assisted large retinal epithelium patching in sub-macular hemorrhage secondary to age related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2009 Feb;247(2):187-91. Epub 2008 Oct 17.
- ↑ Ma Z, Han L, Wang C, Dou H, Hu Y, Feng X, Xu Y, Wang Z, Yin Z, Liu Y. Autologous transplantation of retinal pigment epithelium-Bruch's membrane complex for hemorrhagic age-related macular degeneration. Invest Ophthalmol Vis Sci. 2009 Jun;50(6):2975-81. Epub 2008 Dec 30.
- ↑ MacLaren RE, Uppal GS, Balaggan KS, Tufail A, Munro PM, Milliken AB, Ali RR, Rubin GS, Aylward GW, da Cruz L. Autologous transplantation of the retinal pigment epithelium and choroid in the treatment of neovascular age-related macular degeneration. Ophthalmology. 2007 Mar;114(3):561-70.
- ↑ Tezel TH, Del Priore LV, Berger AS, Kaplan HJ. Adult retinal pigment epithelial transplantation in exudative age-related macular degeneration. Am J Ophthalmol. 2007 Apr;143(4):584-95. Epub 2007 Feb 14.
- ↑ Stanga PE, Kychenthal A, Fitzke FW, Halfyard AS, Chan R, Bird AC, Aylward GW. Retinal pigment epithelium translocation after choroidal neovascular membrane removal in age-related macular degeneration. Ophthalmology. 2002 Aug;109(8):1492-8.
- ↑ Binder S, Krebs I, Hilgers RD, Abri A, Stolba U, Assadoulina A, Kellner L, Stanzel BV, Jahn C, Feichtinger H. Outcome of transplantation of autologous retinal pigment epithelium in age-related macular degeneration: a prospective trial. Invest Ophthalmol Vis Sci. 2004 Nov;45(11):4151-60.
- ↑ Rouvas AA, Papakostas TD, Ntouraki A, Douvali M, Vergados I, Ladas ID. PHOTODYNAMIC THERAPY, RANIBIZUMAB, AND RANIBIZUMAB WITH PHOTODYNAMIC THERAPY FOR THE TREATMENT OF POLYPOIDAL CHOROIDAL VASCULOPATHY. Retina. 2010 Oct 13. [Epub ahead of print] PubMed PMID: 20948458.
- ↑ Ahmad S, Bearelly S, Stinnett SS, Cooney MJ, Fekrat S. Photodynamic therapy for predominantly hemorrhagic lesions in neovascular age-related macular degeneration. Am J Ophthalmol. 2008 Jun;145(6):1052-1057. Epub 2008 Apr 9. PubMed PMID: 18400198.
- ↑ Chan WM, Liu DT, Lai TY, Li H, Tong JP, Lam DS. Extensive submacular haemorrhage in polypoidal choroidal vasculopathy managed by sequential gas displacement and photodynamic therapy: a pilot study of one-year follow up. Clin Experiment Ophthalmol. 2005 Dec;33(6):611-8. PubMed PMID: 16402954.
- ↑ Heriot, Pre-AAO meeting, Chicago, IL 1996.
- ↑ Ohji M, Saito Y, Hayashi A, Lewis JM, Tano Y. Pneumatic displacement of subretinal hemorrhage without tissue plasminogen activator. Arch Ophthalmol. 1998 Oct;116(10):1326-32.
- ↑ Hassan AS, Johnson MW, Schneiderman TE, Regillo CD, Tornambe PE, Poliner LS, Blodi BA, Elner SG. Management of submacular hemorrhage with intravitreous tissue plasminogen activator injection and pneumatic displacement. Ophthalmology. 1999 Oct;106(10):1900-6; discussion 1906-7.
- ↑ Handwerger BA, Blodi BA, Chandra SR, Olsen TW, Stevens TS. Treatment of submacular hemorrhage with low-dose intravitreal tissue plasminogen activator injection and pneumatic displacement. Arch Ophthalmol. 2001 Jan;119(1):28-32.
- ↑ Holland D, Wiechens B. Intravitreal r-TPA and gas injection in traumatic submacular hemorrhage. Ophthalmologica. 2004 Jan-Feb;218(1):64-9.
- ↑ Wu TT, Sheu SJ. Intravitreal tissue plasminogen activator and pneumatic displacement of submacular hemorrhage secondary to retinal artery macroaneurysm. J Ocul Pharmacol Ther. 2005 Feb;21(1):62-7.
- ↑ Yang PM, Kuo HK, Kao ML, Chen YJ, Tsai HH. Pneumatic displacement of a dense submacular hemorrhage with or without tissue plasminogen activator. Chang Gung Med J. 2005 Dec;28(12):852-9.
- ↑ Gopalakrishan M, Giridhar A, Bhat S, Saikumar SJ, Elias A, N S. Pneumatic displacement of submacular hemorrhage: safety, efficacy, and patient selection. Retina. 2007 Mar;27(3):329-34.
- ↑ Ron Y, Ehrlich R, Axer-Siegel R, Rosenblatt I, Weinberger D. Pneumatic displacement of submacular hemorrhage due to age-related macular degeneration. Ophthalmologica. 2007;221(1):57-61.
- ↑ Fang IM, Lin YC, Yang CH, Yang CM, Chen MS. Effects of intravitreal gas with or without tissue plasminogen activator on submacular haemorrhage in age-related macular degeneration. Eye (Lond). 2009 Feb;23(2):397-406. Epub 2007 Nov 2.
- ↑ Olmos L, Flynn, HW, Leung E. Submacular hemorrhage associated with age-related macular degeneration: favorable response to treatment with intravitreal ranibizumab alone. 2010. Ophthalmology Management; 46: October 2010.
- ↑ Chang MA, Do DV, Bressler SB, Cassard SD, Gower EW, Bressler NM. Prospective one-year study of ranibizumab for predominantly hemorrhagic choroidal neovascular lesions in age-related macular degeneration. Retina. 2010 Sep;30(8):1171-6.
- ↑ Sandhu SS, Manvikar S, Steel DH. Displacement of submacular hemorrhage associated with age-related macular degeneration using vitrectomy and submacular tPA injection followed by intravitreal ranibizumab. Clin Ophthalmol. 2010 Jul 21;4:637-42.
- ↑ Ferraz DA, Bressanim GL, Morita C, Takahashi WY. [Intravitreous injection of bevacizumab and C3F8 gas for the treatment of submacular hemorrhage due to age-related macular degeneration: case reports]. Arq Bras Oftalmol. 2010 Feb;73(1):77-80.
- ↑ Matt G, Sacu S, Stifter E, Prünte C, Schmidt-Erfurth U. [Combination of Intravitreal rTPA, gas and ranibizumab for extensive subfoveal haemorrhages secondary to neovascular age-related macular degeneration]. Klin Monbl Epub 2010 Mar 16. German. Augenheilkd. 2010 Mar;227(3):221-5.
- ↑ Arias L, Monés J. Transconjunctival sutureless vitrectomy with tissue plasminogen activator, gas and intravitreal bevacizumab in the management of predominantly hemorrhagic age-related macular degeneration. Clin Ophthalmol. 2010 Feb 18;4:67-72.
- ↑ Auriol S, Mahieu L, Lequeux L, Quintyn JC, Pagot-Mathis V. [Pars plana vitrectomy, subretinal injection of recombinant tissue plasminogen activator and fluid-gas exchange in the management of massive submacular hemorrhages secondary to age-related macular degeneration]. J Fr Ophtalmol. 2010 Feb;33(2):84-91. Epub 2010 Jan 25. French.
- ↑ Treumer F, Klatt C, Roider J, Hillenkamp J. Subretinal coapplication of recombinant tissue plasminogen activator and bevacizumab for neovascular age-related macular degeneration with submacular haemorrhage. Br J Ophthalmol. 2010 Jan;94(1):48-53. Epub 2009 Nov 27. PubMed PMID: 19946027.
- ↑ Höhn F, Mirshahi A, Hattenbach LO. [Combined intravitreal injection of bevacizumab and SF6 gas for treatment of submacular hemorrhage secondary to age-related macular degeneration]. Ophthalmologe. 2010 Apr;107(4):328-32.
- ↑ Shah SP, Hubschman JP, Gonzales CR, Schwartz SD. Submacular combination treatment for management of acute, massive submacular hemorrhage in age-related macular degeneration. Ophthalmic Surg Lasers Imaging. 2009 May-Jun;40(3):308-15.
- ↑ Chawla S, Misra V, Khemchandani M. Pneumatic displacement and intravitreal bevacizumab: a new approach for management of submacular hemorrhage in choroidal neovascular membrane. Indian J Ophthalmol. 2009 Mar-Apr;57(2):155-7.
- ↑ Stifter E, Michels S, Prager F, Georgopoulos M, Polak K, Hirn C, Schmidt-Erfurth U. Intravitreal bevacizumab therapy for neovascular age-related macular degeneration with large submacular hemorrhage. Am J Ophthalmol. 2007 Dec;144(6):886-892. Epub 2007 Oct 4.
- ↑ Cleary CA, Jungkim S, Ravikumar K, Kelliher C, Acheson RW, Hickey-Dwyer M. Intravitreal bevacizumab in the treatment of neovascular age-related macular degeneration, 6- and 9-month results. Eye (Lond). 2008 Jan;22(1):82-6. Epub 2007 Sep 21.
- ↑ Meyer CH, Scholl HP, Eter N, Helb HM, Holz FG. Combined treatment of acute subretinal haemorrhages with intravitreal recombined tissue plasminogen activator, expansile gas and bevacizumab: a retrospective pilot study. Acta Ophthalmol. 2008.
References: Submacular Surgery Trials Reports
- Solomon SD, Dong LM, Haller JA, Gilson MM, Hawkins BS, Bressler NM; SST research group and the SST adverse event review committee. Risk factors for rhegmatogenous retinal detachment in the submacular surgery trials: SST report No. 22. Retina. 2009 Jun;29(6):819-24.
- Submacular Surgery Trials Research Group, Solomon SD, Jefferys JL, Hawkins BS, Bressler NM, Bressler SB. Risk factors for second eye progression to advanced age-related macular degeneration: SST report No. 21 Submacular Surgery Trials Research Group. Retina. 2009 Sep;29(8):1080-90.
- Submacular Surgery Trials Research Group, Solomon SD, Jefferys JL, Hawkins BS, Bressler NM. Incident choroidal neovascularization in fellow eyes of patients with unilateral subfoveal choroidal neovascularization secondary to age-related macular degeneration: SST report No. 20 from the Submacular Surgery Trials Research Group. Arch Ophthalmol. 2007 Oct;125(10):1323-30.
- Submacular Surgery Trials Research Group. Evaluation of minimum clinically meaningful changes in scores on the National Eye Institute Visual Function Questionnaire (NEI-VFQ) SST Report Number 19. Ophthalmic Epidemiol. 2007 Jul-Aug;14(4):205-15.
- Submacular Surgery Trials Research Group, Mann AL, Bressler SB, Hawkins BS, Holekamp N, Bressler NM. Comparison of methods to identify incident cataract in eyes of patients with neovascular maculopathy: Submacular Surgery Trials Report No. 18. Ophthalmology. 2008 Jan;115(1):127-33.
- Bass EB, Gilson MM, Mangione CM, Hawkins BS, Miskala PH, Mann AL, Bressler NM.Surgical removal vs observation for idiopathic or ocular histoplasmosis syndrome-associated subfoveal choroidal neovascularization: Vision Preference Value Scale findings from the randomized SST Group H Trial: SST Report No. 17. Arch Ophthalmol. 2008 Dec;126(12):1626-32
- Grossniklaus HE, Wilson DJ, Bressler SB, Bressler NM, Toth CA, Green WR, Miskala P. Clinicopathologic studies of eyes that were obtained postmortem from four patients who were enrolled in the submacular surgery trials: SST Report No. 16. Am J Ophthalmol. 2006 Jan;141(1):93-104.
- Submacular Surgery Trials Research Group. Comparison of 2D reconstructions of surgically excised subfoveal choroidal neovascularization with fluorescein angiographic features: SST report No. 15. Ophthalmology. 2006 Feb;113(2):279.e1-279.e5. Epub 2006 Jan 10.
- Childs AL, Bressler NM, Bass EB, Hawkins BS, Mangione CM, Marsh MJ, Miskala PH; Submacular Surgery Trials (SST) Research Group. Surgery for hemorrhagic choroidal neovascular lesions of age-related macular degeneration: quality-of-life findings: SST report no. 14. Ophthalmology. 2004 Nov;111(11):2007-14.
- Bressler NM, Bressler SB, Childs AL, Haller JA, Hawkins BS, Lewis H, MacCumber MW, Marsh MJ, Redford M, Sternberg P Jr, Thomas MA, Williams GA; Submacular Surgery Trials (SST) Research Group. Surgery for hemorrhagic choroidal neovascular lesions of age-related macular degeneration: ophthalmic findings: SST report no. 13. Ophthalmology. 2004 Nov;111(11):1993-2006.
- Miskala PH, Bass EB, Bressler NM, Childs AL, Hawkins BS, Mangione CM, Marsh MJ; Submacular Surgery Trials (SST) Research Group. Surgery for subfoveal choroidal neovascularization in age-related macular degeneration: quality-of-life findings: SST report no. 12. Ophthalmology. 2004 Nov;111(11):1981-92.
- Hawkins BS, Bressler NM, Miskala PH, Bressler SB, Holekamp NM, Marsh MJ, Redford M, Schwartz SD, Sternberg P Jr, Thomas MA, Wilson DJ; Submacular Surgery Trials (SST) Research Group. Surgery for subfoveal choroidal neovascularization in age-related macular degeneration: ophthalmic findings: SST report no. 11. Ophthalmology. 2004 Nov;111(11):1967-80.
- Hawkins BS, Miskala PH, Bass EB, Bressler NM, Childs AL, Mangione CM, Marsh MJ; Submacular Surgery Trials Research Group. Surgical removal vs observation for subfoveal choroidal neovascularization, either associated with the ocular histoplasmosis syndrome or idiopathic: II. Quality-of-life findings from a randomized clinical trial: SST Group H Trial: SST Report No. 10. Arch Ophthalmol. 2004 Nov;122(11):1616-28.
- Hawkins BS, Bressler NM, Bressler SB, Davidorf FH, Hoskins JC, Marsh MJ, Miskala PH, Redford M, Sternberg P Jr, Thomas MA, Toth CA; Submacular Surgery Trials Research Group. Surgical removal vs observation for subfoveal choroidal neovascularization, either associated with the ocular histoplasmosis syndrome or idiopathic: I. Ophthalmic findings from a randomized clinical trial: Submacular Surgery Trials (SST) Group H Trial: SST Report No. 9. Arch Ophthalmol. 2004 Nov;122(11):1597-611. Erratum in: Arch Ophthalmol. 2005 Jan;123(1):28.
- Solomon SD, Bressler SB, Hawkins BS, Marsh MJ, Bressler NM; Submacular Surgery Trials Research Group. Guidelines for interpreting retinal photographs and coding findings in the Submacular Surgery Trials (SST): SST report no. 8. Retina. 2005 Apr-May;25(3):253-68.
- Grossniklaus HE, Miskala PH, Green WR, Bressler SB, Hawkins BS, Toth C, Wilson DJ, Bressler NM. Histopathologic and ultrastructural features of surgically excised subfoveal choroidal neovascular lesions: submacular surgery trials report no. 7. Arch Ophthalmol. 2005 Jul;123(7):914-21.
- Bass EB, Marsh MJ, Mangione CM, Bressler NM, Childs AL, Dong LM, Hawkins BS, Jaffee HA, Miskala P; Submacular Surgery Trials Research Group. Patients' perceptions of the value of current vision: assessment of preference values among patients with subfoveal choroidal neovascularization--The Submacular Surgery Trials Vision Preference Value Scale: SST Report No. 6. Arch Ophthalmol. 2004 Dec;122(12):1856-67.
- Submacular Surgery Trials Research Group. Health- and vision-related quality of life among patients with ocular histoplasmosis or idiopathic choroidal neovascularization at enrollment in a randomized trial of submacular surgery: Submacular Surgery Trials Report No. 5. Arch Ophthalmol. 2005 Jan;123(1):78-88.
- Dong LM, Childs AL, Mangione CM, Bass EB, Bressler NM, Hawkins BS, Marsh MJ, Miskala P, Jaffee HA, McCaffrey LA; Submacular Surgery Trials Research Group. Health- and vision-related quality of life among patients with choroidal neovascularization secondary to age-related macular degeneration at enrollment in randomized trials of submacular surgery: SST report no. 4. Am J Ophthalmol. 2004 Jul;138(1):91-108.
- Submacular Surgery Trials Research Group. Effect of order of administration of health-related quality of life instruments on responses. SST report no. 3. QOL Research 2005;14:493-500.
- Bressler NM, Hawkins BS, Bressler SB, Miskala PH, Marsh MJ; Submacular Surgery Trials Research Group. Clinical trial performance of community- vs university-based practices in the submacular surgery trials (SST): SST report no. 2. Arch Ophthalmol. 2004 Jun;122(6):857-63.
- Miskala PH, Hawkins BS, Mangione CM, Bass EB, Bressler NM, Dong LM, Marsh MJ, McCaffrey LD; Submacular Surgery Trials Research Group. Responsiveness of the National Eye Institute Visual Function Questionnaire to changes in visual acuity: findings in patients with subfoveal choroidal neovascularization--SST Report No. 1. Arch Ophthalmol. 2003 Apr;121(4):531-9. Erratum in: Arch Ophthalmol. 2003 Oct;121(10):1513.
- Gopalakrishan M, Giridhar A, Bhat S, Saikumar SJ, Elias A, N S. Pneumatic displacement of submacular hemorrhage: safety, efficacy, and patient selection. Retina. 2007 Mar;27(3):329-34. PubMed PMID: 17460588. 08 Aug;86(5):490-4. Epub 2008 Jan 24.