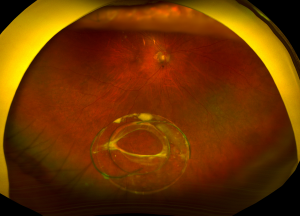
Dislocated Intraocular Lens
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Background
Dislocated intraocular lens (IOL) is a rare, yet serious ,complication whereby the IOL moves out of its normal position in the eye. Intraocular lens dislocation has been reported at a rate of 0.2%–3%.[1] [2] [3] [4] It may occur as a result of cataract surgery, prior vitreoretinal surgery, trauma, or an inherent pathologic process or connective tissue disorder contributing to lens zonular weakness.[5] Dislocation may present as phacodonesis, simple decentration within the bag or in the sulcus, partial subluxation, or complete dislocation of the lens within and outside of the bag. Decentration usually refers to loss of IOL centration without zonular or capsular instability. Subluxation refers to partial zonular or capsular instability. Dislocation is due to total zonular or capsular instability. However, all of these the terms are often used interchangeably. Once the dislocated IOL is identified, there are several possible management options.
Etiology/Risk Factors
IOL dislocation is typically related to the integrity of the capsular bag and its support system (zonules) and their ability to support the IOL. As noted in the previous section, there are many predisposing conditions that increase the risk of capsular bag instability and zonular weakness, including cataract surgery, prior vitreoretinal surgery,[6] [7] [8] aging,[7] axial myopia,[8][9] inflammation/uveitis,[8][10] trauma,[6][11] retinitis pigmentosa,[4] [8] diabetes mellitus,[12] atopic dermatitis,[11] mature cataract,[8] previous episodes of acute angle-closure attack,[13] connective tissue disorders (e.g., pseudoexfoliation syndrome, being the most common risk factor with more than 50% of cases), Marfan syndrome, homocystinuria, hyperlysinemia, Ehlers-Danlos Syndrome, scleroderma, Weill-Marchesani syndrome, and ectopia lentis et pupillae.[4] [6] [7][14] [15]
Dislocation of the IOL due to cataract surgery may be categorized based on the timing of its presentation—early if it occurs within 3 months of IOL placement, and late if it occurs ≥3 months after IOL placement. Early dislocation of the lens may occur with poor fixation of the IOL or capsular and/or zonular rupture during cataract surgery.[5] Zonular rupture usually occurs from posterior pressure on the lens and the capsule while performing "can-opener style" capsulotomy, phacoemulsification of the nucleus, or IOL implantation.[12] Late dislocation of the lens typically occurs due to progressive zonular insufficiency and contraction of the anterior capsule.[5] Progressive zonular weakness has been associated with previous vitreoretinal surgery, uveitis, trauma, high myopia, retinitis pigmentosa, aging, diabetes mellitus, atopic dermatitis (e.g., repeated eye rubbing), previous acute angle-closure attacks, and connective tissue disorders.[5] [6][16] [17]
Capsular opening contraction is commonly observed after cataract surgery and can be accompanied by continuous curvilinear capsulorrhexis. Trauma caused by capsulotomy of the anterior capsule leads to proliferation and metaplasia of the lens epithelial cells on the capsular margins into myofibroblasts, which subsequently creates a contraction force. This centripetal force overcomes the centrifugal zonal force and leads to constriction of the capsulotomy.[18] In patients with weaker zonules, as seen in pseudoexfoliation syndrome, retinitis pigmentosa, and diabetes mellitus, the constriction that occurs is more pronounced.[19] Increased epithelial cell proliferation seen in posterior capsular opacification (PCO) may contribute to the IOL and capsular bag weight, which leads to increased zonular stress.[20] The impact of neodymium:YAG laser treatment of PCO may be the trigger point for subluxation.[4] [6]
Diagnosis
History, Signs, and Symptoms
Given that there are many predisposing conditions that increase the risk of IOL dislocation, a thorough patient history is needed. Patients with a dislocated IOL may experience a decrease or change in vision, diplopia, and/or glare.[5] Additionally, they may report ocular pain or headaches from intermittent angle-closure and/or inflammation. Some patients also report seeing the edge of the IOL.
Diagnostic Procedures
A complete ophthalmologic exam is necessary for diagnosing a dislocated IOL, including an anterior and posterior segment exam. A detailed dilated retinal exam with scleral depression is important. If a detailed exam is not feasible, Bscan echography and/or an anterior segment OCT/ultrasound biomicroscopy may be helpful in evaluating a posteriorly dislocated lens behind the iris in the anterior aspect of the vitreous cavity.
Types of IOL Dislocation
Dislocation may present as phacodonesis, simple lens decentration within an intact capsular bag or in the sulcus, partial lens subluxation out of the capsular bag, or complete dislocation of the lens within or outside of the bag into the anterior or posterior chamber. If there is a posterior capsule defect or tear, the IOL may slide out of the bag (out-of-the-bag dislocation). If there is a defect in the stability of the capsular bag support system (e.g., zonular weakness), the entire IOL with the capsular bag may dislocate (in-the-bag dislocation).
Treatment Options
Observation
Observation may be a possible management option in cases where IOL subluxation is minimal without a significant impact on vision and damage to surrounding ocular structures. Patients with pseudophacodonesis and without inferior dislocation are usually asymptomatic and tend to be good candidates for observation.[21] In such cases, refraction may help sharpen the patient’s vision with close monitoring thereafter; close follow-up is imperative to ensure that patients do not develop potential IOL dislocation sequelae that may necessitate surgical intervention.
In cases where vision is affected and/or there is damage to surrounding ocular structures, surgery plays a large role in IOL dislocation management. The most common indications for surgery are decreased visual acuity, monocular diplopia, and halos.[4] Less commonly, retinal detachment,[12] glaucoma,[15] and/or Uveitis-Glaucoma-Hyphema (UGH) syndrome[14] portend surgical intervention. Several surgical options exist and should be tailored to each individual. Surgery typically includes pars plana vitrectomy to remove the dislocated lens with either an IOL cutter or through a scleral tunnel or sclerocorneal incision; this is followed by secondary IOL implantation.
IOL Exchange
IOL exchange is the most common surgical option. The dislocated IOL is removed, and the decision whether to place a new IOL in either the anterior or posterior chamber becomes a matter of the integrity of the capsular bag. If there is adequate capsular support, an IOL may be placed in the posterior chamber (PCIOL) and repositioned in the ciliary sulcus. If there is not enough capsular support, an IOL can be placed in the anterior chamber (ACIOL) or sutured in place to either the sclera or iris. There seems to be insufficient evidence, in terms of relative safety or efficacy, to support ACIOL implantation vs scleral or iris-supported PCIOL implantation.[22] [23]
IOL Fixation Procedures
IOL fixation procedures provide surgical options in cases where there is not enough capsular bag support, and include transscleral suture fixation, transscleral haptic fixation, and iris fixation. Depending on the eye anatomy, including the status of the cornea, iris, and sclera, the ocular pathology, and the comfort of the surgeon, the fixation procedure can be tailored to the individual.
Transscleral Suture Fixation
Transscleral suture fixation is a possible option in patients without sufficient capsular bag support. This may be achieved either through an ab interno or ab externo approach, where the sutures are passed from inside to outside blindly or from outside to inside the eye, respectively. With both approaches, the lens is placed between the iris and the anterior vitreous cavity and is fixated by sutures from opposite sides. The sutures are then buried within the sclera. Different lenses and sutures are used depending on the surgeon's comfort level and experience.
CZ70BD (Alcon) is a nonfoldable, polymethyl methacrylate (PMMA) single-piece IOL with eyelets on each side, which facilitate secured suturing. The size of the lens is 12.0 mm in length with an optic diameter of 7.0 mm. Because of its nonfoldable nature , larger incisions are required.
Akreos AO60 (Bausch + Lomb) is a foldable acrylic single-piece IOL. As it is a foldable lens, the incision site can be made smaller, which facilitates better maintenance of the anterior chamber and globe structure during the surgery and leads to less wound leakage.[24] The lens has 2 eyelets on each opposite side, allowing for a 4-point fixation. It is theorized that the 4-point fixation provides improved stability to help decrease tilting, although there is no study that directly compares the CZ70BD and Akreos AO60 IOLs. Additionally, there have been reports that there is increased risk of calcification and opacification of the Akreos AO60 through calcium salt deposition with exposure to intraocular air or gas.[25]
MX60 enVista (Bausch + Lomb) is a foldable acrylic IOL. This IOL can be inserted with a smaller incision, and the eyelets are located on each side at the haptic-optic junction. Unlike the Akreos AO60 IOL, MX60 enVista is a hydrophobic lens, and there is less concern for opacification. Furthermore, with uniform center-to-edge power, decentration is thought to be less of a concern. This IOL comes in a toric form for patients with astigmatism.
There have been reports of single-piece toric IOLs that have been inserted with transscleral suture fixation.[26] [27] The IOLs that were used for transscleral suture fixation were Centerflex 570T (Rayner) and SN6AT5 (Alcon). The Centerflex 570T is a foldable IOL. It has 2 closed loops where the sutures were fixated.[26] The SN6AT5 IOL does not have loops or eyelets, so the sutures had to be secured in a "lasso-type" fashion.[27]
A variety of sutures are currently used for transscleral suture fixation, including 10-0 polypropylene, 9-0 polypropylene, and CV-8 Gore-Tex. 10-0 polypropylene has traditionally been the suture of choice; however, IOL dislocations secondary to suture erosions and breakages have been reported.[28] [29] [30] These suture breakages have been associated with how long the sutures had been in place. The mean time from surgery until breakage ranged from 4 to 6.5 years. These reports suggest that it would be better to utilize a thicker suture such as 9-0 polypropylene, which is reported to have higher tensile strength to withstand the biodegradation seen with 10-0 polypropylene.[28] However, there is another study that questions the superiority of 9-0 over 10-0 polypropylene and the potential increased risk of endophthalmitis owing to the larger suture size and erosion into the sclera.[31]
Recently, CV-8 Gore-Tex has also been selected as a suture of choice due to its high tensile strength and longevity and the decreased risk of suture breakage.[24][32] While the long-term complications and outcomes of scleral fixation with Gore-Tex sutures have not been evaluated, several studies have shown success in utilizing Gore-Tex sutures for scleral fixation with minimal suture complications.[32] However, longer-term studies are needed for better comparison.
Transscleral Haptic Fixation
Transscleral haptic fixation is a possible option in patients without sufficient capsular bag support. It is a modification of sutureless intrascleral 3-piece IOL fixation. The double-needle flanged IOL fixation, also known as the Yamane technique, is carried out via the conjunctiva with small incisions made by 30-gauge needles. The needles are inserted through the sclera, 2 mm posterior to the limbus, and the 3-piece IOL haptics are fed into the lumen of the needles and are pulled out of the scleral tunnels. This fixates the haptics to the sclera without suture or glue by means of a flange at the end of the haptic for firm fixation in the scleral tunnel (the protruding ends of the haptics are cauterized to prevent slippage into the eye). A peripheral iridotomy is then placed after miosis to avoid iris capture of the IOL. This double-needle technique minimizes the sclerotomy and decreases the risk of postoperative hypotony.[33]
IOL selection for the Yamane technique is crucial, given that conventional PMMA haptics are reportedly prone to kinking, breaking, or disinserting from the optic during intraoperative manipulation. AR40E (AMO Sensar) is a hydrophobic acrylic 3-piece IOL with PMMA-angulated haptics. MA60AC (AcrySof) is an acrylic foldable 3-piece lens with PMMA haptics that may be folded prior to insertion. CT Lucia 602 (Carl Zeiss Meditec) is a hydrophobic acrylic lens typically recommended with the Yamane technique due to the durability of its haptics, which are composed of polyvinylidene fluoride.[34] [35]
Currently, there is no IOL specifically designed for the Yamane technique. One study compared the use of NX-70 and PN6A IOLs in the flanged IOL fixation technique and revealed no statistically significant differences between the two. While fewer intra- and postoperative complications were noted with the NX-70 IOLs, PN6A IOLs were easier to maneuver in the anterior chamber with shorter operating times. The authors of this study recommended the use of strong-jointed IOLs (e.g., NX-70) to avoid detachment of the haptic from the optic.[36]
Fibrin glue–assisted sutureless posterior chamber IOL implantation is also an option in patients with deficient posterior capsules. This surgical technique places 2 partial-thickness, limbal-based scleral flaps 180 degrees apart, and the lens haptics are externalized with the use of forceps to place them inside the scleral tunnels beneath the scleral flaps. Fibrin glue is used to attach the haptics to the scleral bed beneath the flap.[37] This technique, like the Yamane technique, does not require sutures.
Iris Suture Fixation
Iris-fixated IOLs were previously used in the form of claw-shaped haptic devices; however, high complication rates and suboptimal visual outcomes led to vault modifications from the original design, whereby iris clip or iridocapsular lenses were used.[38] [39] Iris-claw IOLs are currently used for both the phakic correction of myopia and correction of aphakia in the absence of capsular support.[40]
An iris-claw IOL may be placed either in the anterior or the posterior chamber (retropupillary) to reduce the potential for complications that are seen with ACIOLs; the chamber placement will depend on the surgeon's experience and the characteristics of the procedure.[41] For anterior chamber placement, the IOL is placed into the anterior chamber with the iris enclavated at its mid-peripheral region between claw haptics. For retropupillary fixation, one haptic of the IOL is introduced behind the iris and enclavated, followed by enclavation of the other haptic.[41] A peripheral iridectomy is performed for anterior implantation.
Out-of-the-bag dislocated IOLs may also be sutured to the iris, assuming that the IOL is not damaged and is of the appropriate power. Iris suturing techniques have included the optic of a dislocated 3-piece IOL prolapsed into the anterior chamber above the iris while the haptics are in the ciliary sulcus, emulating an optic capture. After miosis, 4 paracentesis wounds help to fixate each of the haptics to the peripheral iris. A modified McCannel iris suturing technique, using a Siepser sliding knot technique, has shown success in suturing the haptics with McCannel polypropylene suture on a curved needle to the iris. The optic is then moved behind the iris.[42] [43]
ACIOL Placement
In the absence of adequate capsular support, implantation of a flexible open-loop ACIOL is an option.[44] [45] However, anterior chamber depth and anterior chamber angle support assessment is imperative. Currently, modern flexible open-loop haptics and anteriorly vaulted optics compose ACIOLs, which have been modified from previous designs to result in lower rate of complications.[46] [47] Footplates are incorporated into each haptic to provide stability, while decreasing the amount of contact with the angle.[48] Additionally, ACIOLs have an anterior vault to reduce the risk of iris chafe and corneal touch.[49]
ACIOL placement typically involves placing the lens into the anterior chamber through a temporal scleral tunnel incision with assistance from a lens glide to rest footplates against the scleral spur. Avoiding incarceration of iris tissue or rubbing against the corneal endothelium during the process is key.[38] The scleral tunnel incision is usually closed with 10-0 nylon sutures.
It is important to choose the appropriate ACIOL power, since these lenses require less power than a more posterior IOL. Additionally, horizontal white-to-white measurement of the corneal width aids in ensuring that the lens is the proper size and fit for the patient. A peripheral iridectomy should also be performed to prevent pupillary block.
Complications
IOL dislocation may lead to several complications, such as recurrent IOL dislocation,[8] [12] [50] [51] retinal detachment,[2][8][12][51][52] infection/hypopyon,[2] inflammation, bleeding, corneal damage,[2] macular edema,[2][8][12][53] and elevated intraocular pressure.[2][53] Sight-threatening complications such as hyphema, secondary glaucoma, macular edema, and pupillary block tend to develop in ACIOL and iris-fixation IOL cases, with iris fixation lenses having a higher incidence of lens dislocation and subsequent corneal decompensation.[2]
Transscleral suture–fixated lenses run the risk of retinal detachment and intraocular hemorrhage, given the passage of sutures through the uveal tissue.[21] Additionally, exposed suture tracks may lead to suture knot and tissue erosion and an increased risk of endophthalmitis,[21][45] with late IOL dislocation or tilt a potential existing concern as a result of suture loosening or rupture.[21][38]
Transscleral haptic–fixated lenses may cause intraocular hemorrhage as well, given that they involve fixation of IOL haptics through the uveal tissue and partial-thickness scleral flaps or tunnels.[54]
ACIOLs are in close proximity to the cornea and anterior chamber angle, and thus could damage the cornea, iris, and angle. There exists an increased risk of pseudophakic bullous keratopathy, glaucoma, UGH syndrome, pupillary block and peripheral anterior synechiae, cystoid macular edema.[21] [38] [47] Given the concern for such complications, some studies have recommended avoiding ACIOL implantation in patients aged <50 years.[55] Newer ACIOL models have flexible loops and highly polished surfaces, and thus are less likely to cause problems.[38]
Similar to ACIOLs, iris-sutured fixation lenses rest in close proximity to the cornea, increasing the risk of corneal decompensation.[56] Also, their proximity to the iris may disrupt the integrity of the iris, leading to iris chaffing, pigment dispersion, chronic inflammation, peripheral synechiae, bleeding from the iris, pupillary distortion, and limited pupillary dilation.[38][42] [57]
Prognosis
Most patients with IOL dislocation do quite well with management, as long as visual acuity and postsurgical outcomes are considered.[4][45] Visual acuity study results have demonstrated that at least 85% of IOL cases overall achieve 20/40 or better acuity.[1] [2] Increasing age, preoperative corneal disease, glaucoma, iritis, iris neovascularization, diabetic retinopathy, history of retinal detachment, macular degeneration, amblyopia, surgical problems, and complications such as corneal and/or macular edema portend unfavorable visual outcomes.[2] Nonetheless, close follow-up and management may allow for avoidance of complications. Cautious pre-, intra-, and postoperative assessments are imperative for achieving good outcomes.
References
- ↑ Jump up to: 1.0 1.1 Stark WJ Jr., Maumenee AE, Datiles M, et al. Intraocular lenses: complications and visual results. Trans Am Ophthalmol Soc. 1983;81:280-309.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Stark WJ, Worthen DM, Holladay JT, et al. The FDA report on intraocular lenses. Ophthalmology. 1983;90:311-317.
- ↑ Kratz RP, Mazzocco TR, Davidson B, et al. The Shearing intraocular lens: a report of 1,000 cases. J Am Intraocul Implant Soc. 1981:7(1):55-57.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 Gimbel HV, Condon GV, Kohnen T, et al. Late in-the-bag intraocular lens dislocation: incidence, prevention, and management. J Cataract Refract Surg. 2005;31(11):2193-2204.
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 Ascaso FJ, Huerva V, Grzybowski A. Epidemiology, etiology, and prevention of late IOL-capsular bag complex dislocation: review of the literature. J Ophthalmol. 2015;2015:805706.
- ↑ Jump up to: 6.0 6.1 6.2 6.3 6.4 Davis D, Brubaker J, Espandar L, et al. Late in-the-bag spontaneous intraocular lens dislocation: evaluation of 86 consecutive cases. Ophthalmology. 2009;116(4):664-670.
- ↑ Jump up to: 7.0 7.1 7.2 Matsumoto M, Yamada K, Uematsu M, et al. Spontaneous dislocation of in-the-bag intraocular lens primarily in cases with prior vitrectomy. Eur J Ophthalmol. 2012;22(3):363-367.
- ↑ Jump up to: 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Hayashi K, Hirata A, Hayashi H. Possible predisposing factors for in-the-bag and out-of-the-bag intraocular lens dislocation and outcomes of intraocular lens exchange surgery. Ophthalmology. 2007;114(5):969-975.
- ↑ Shigeeda T, Nagahara M, Kato S, et al. Spontaneous posterior dislocation of intraocular lenses fixated in the capsular bag. J Cataract Refract Surg. 2002;28(9):1689-1693.
- ↑ Brilakis HS, Lustbader JM. Bilateral dislocation of in-the-bag posterior chamber intraocular lenses in a patient with intermediate uveitis. J Cataract Refract Surg. 2003;29(10):2013-2014.
- ↑ Jump up to: 11.0 11.1 Yamazaki S, Nakamura K, Kurosaka D. Intraocular lens subluxation in a patient with facial atopic dermatitis. J Cataract Refract Surg. 2001;27(2):337-338.
- ↑ Jump up to: 12.0 12.1 12.2 12.3 12.4 12.5 Gross JG, Kokame GT, Weinberg DV; Dislocated In-The-Bag Intraocular Lens Study Group. In-the-bag intraocular lens dislocation. Am J Ophthalmol. 2004;137:630-635.
- ↑ Su WW, Chang SH. Spontaneous, late, in-the-bag intraocular lens subluxation in a patient with a previous acute angle-closure glaucoma attack. J Cataract Refract Surg. 2004;30(8):1805-1807.
- ↑ Jump up to: 14.0 14.1 Masket S, Osher SH. Late complications with intraocular lens dislocation after capsulorhexis in pseudoexfoliation syndrome. J Cataract Refract Surg. 2002;28(8):1481-1484.
- ↑ Jump up to: 15.0 15.1 Lim MC, Doe EA, Vroman DT, et al. Late onset lens particle glaucoma as a consequence of spontaneous dislocation of an intraocular lens in pseudoexfoliation syndrome. Am J Ophthalmol. 2001;132(2):261-263.
- ↑ Lee GI, Lim DH, Chi SA, et al. Risk factors for intraocular lens dislocation after phacoemulsification: a nationwide population-based cohort study. Am J Ophthalmol. 2020;214:86-96.
- ↑ Fernández-Buenaga R, Alio JL, Pérez-Ardoy AL, et al. Late in-the-bag intraocular lens dislocation requiring explantation: risk factors and outcomes. Eye (Lond). 2013;27(7):795-801.
- ↑ Joo CK, Shin JA, Kim JH. Capsular opening contraction after continuous curvilinear capsulorhexis and intraocular lens implantation. J Cataract Refract Surg. 1996;22(5):585-590.
- ↑ Hayashi H, Hayashi K, Nakao F, et al. Anterior capsule contraction and intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Br J Ophthalmol. 1998;82:1429-1432.
- ↑ Jehan FS, Mamalis N, Crandall AS. Spontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology. 2001;108:1727-1731.
- ↑ Jump up to: 21.0 21.1 21.2 21.3 21.4 Lorente R, de Rojas V, Vazquez de Parga P, et al. Management of late spontaneous in-the-bag intraocular lens dislocation: retrospective analysis of 45 cases. J Cataract Refract Surg. 2010;36(8):1270-1282.
- ↑ Wagoner MD, Cox TA, Ariyasu RG, et al. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology. 2003;110(4):840-859.
- ↑ Chan TC, Lam JK, Jhanji V, et al. Comparison of outcomes of primary anterior chamber versus secondary scleral-fixated intraocular lens implantation in complicated cataract surgeries. Am J Ophthalmol. 2015;159(2):221-226.e2.
- ↑ Jump up to: 24.0 24.1 Chang DF. Disruptive innovation and refractive IOLs: how the game will change with adjustable IOLs. Asia Pac J Ophthalmol (Phila). 2019;8(6):432-435.
- ↑ Morgan-Warren PJ, Andreatta W, Patel AK. Opacification of hydrophilic intraocular lenses after Descemet stripping automated endothelial keratoplasty. Clin Ophthalmol. 2015;9:277-283.
- ↑ Jump up to: 26.0 26.1 Borkenstein AF, Reuland A, Limberger IJ, et al. Transscleral fixation of a toric intraocular lens to correct aphakic keratoplasty with high astigmatism. J Cataract Refract Surg. 2009;35(5):934-938.
- ↑ Jump up to: 27.0 27.1 Emanuel ME, Randleman JB, Masket S. Scleral fixation of a one-piece toric intraocular lens. J Refract Surg. 2013;29(2):140-142.
- ↑ Jump up to: 28.0 28.1 Price MO, Price FW Jr, Werner L, et al. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31(7):1320-1326.
- ↑ Assia EI, Nemet A, Sachs D. Bilateral spontaneous subluxation of scleral-fixated intraocular lenses. J Cataract Refract Surg. 2002;28(12):2214-2216.
- ↑ Asadi R, Kheirkhah A. Long-term results of scleral fixation of posterior chamber intraocular lenses in children. Ophthalmology. 2008;115(1):67-72.
- ↑ Wasiluk E, Krasnicki P, Dmuchowska DA, et al. The implantation of the scleral-fixated posterior chamber intraocular lens with 9/0 polypropylene sutures — long-term visual outcomes and complications. Adv Med Sci. 2019;64(1):100-103.
- ↑ Jump up to: 32.0 32.1 Khan MA, Gupta OP, Smith RG, et al. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100(5):638-643.
- ↑ Yamane S, Sato S, Maruyama-Inoue M, et al. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
- ↑ Roach L. Intrascleral haptic fixation as an alternative to sutures. EyeNet Magazine. Published May 1, 2018. Accessed March 19, 2025. https://www.aao.org/eyenet/article/haptic-fixation-as-alternative-to-sutures
- ↑ Ayres B, Al-Mohtaseb Z, Safran S, et al. Pearls for the Yamane technique. Retina Today. Accessed March 19, 2025. https://retinatoday.com/articles/2020-mar/pearls-for-the-yamane-technique
- ↑ Miura Y, Harada Y, and Kiuchi Y. Comparison of different IOL types in the flanged IOL fixation technique. J Ophthalmol. 2020;2020:8534028.
- ↑ Agarwal A, Kumar DA, Jacob S, et al. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34(9):1433-1438.
- ↑ Jump up to: 38.0 38.1 38.2 38.3 38.4 38.5 Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol. 2005;50(5):429-462.
- ↑ Binkhorst CD. Results of implantation of intraocular lenses in unilateral aphakia. With special reference to the pupillary or iris clip lens--a new method of fixation. Am J Ophthalmol. 1960;49:703-710.
- ↑ De Silva, S.R., et al., Iris-claw intraocular lenses to correct aphakia in the absence of capsule support. J Cataract Refract Surg, 2011. 37(9): p. 1667-72.
- ↑ Jump up to: 41.0 41.1 Mora P, Calzetti G, Favilla S, et al. Comparative analysis of the safety and functional outcomes of anterior versus retropupillary iris-claw IOL fixation. J Ophthalmol. 2018;2018:8463569.
- ↑ Jump up to: 42.0 42.1 Armonaite L, Lofgren S, Behndig A. Iris suture fixation of out-of-the-bag dislocated three-piece intraocular lenses. Acta Ophthalmol. 2019;97(6):583-588.
- ↑ Chang DF. Siepser slipknot for McCannel iris-suture fixation of subluxated intraocular lenses. J Cataract Refract Surg. 2004;30(6):1170-1176.
- ↑ Kwong YY, Yuen HK, Lam RF, et al. Comparison of outcomes of primary scleral-fixated versus primary anterior chamber intraocular lens implantation in complicated cataract surgeries. Ophthalmology. 2007;114(1):80-85.
- ↑ Jump up to: 45.0 45.1 45.2 Holt DG, Young J, Stagg B, et al. Anterior chamber intraocular lens, sutured posterior chamber intraocular lens, or glued intraocular lens: where do we stand? Curr Opin Ophthalmol. 2012;23(1):62-67.
- ↑ Sawada T, Kimura W, Kimura T, et al. Long-term follow-up of primary anterior chamber intraocular lens implantation. J Cataract Refract Surg. 1998;24(11):1515-1520.
- ↑ Jump up to: 47.0 47.1 Drolsum L. Long-term follow-up of secondary flexible, open-loop, anterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29(3):498-503.
- ↑ Dick HB, Augustin AJ. Lens implant selection with absence of capsular support. Curr Opin Ophthalmol. 2001;12(1):47-57.
- ↑ Apple DJ, Brems RN, Park RB, et al. Anterior chamber lenses. Part I: Complications and pathology and a review of designs. J Cataract Refract Surg. 1987;13(2):157-174.
- ↑ Kim SS, Smiddy WE, Feuer W, et al. Management of dislocated intraocular lenses. Ophthalmology. 2008;115(10):1699-1704.
- ↑ Jump up to: 51.0 51.1 Jakobsson G, Zetterberg M, Sundelin K, et al. Surgical repositioning of intraocular lenses after late dislocation: complications, effect on intraocular pressure, and visual outcomes. J Cataract Refract Surg. 2013;39(12):1879-1885.
- ↑ Mello MO Jr, Scott IU, Smiddy WE, et al. Surgical management and outcomes of dislocated intraocular lenses. Ophthalmology. 2000;107(1):62-67.
- ↑ Jump up to: 53.0 53.1 Kristianslund O, Råen M, Østern AE, et al. Late in-the-bag intraocular lens dislocation: a randomized clinical trial comparing lens repositioning and lens exchange. Ophthalmology. 2017;124(2):151-159.
- ↑ Scharioth GB, Prasad S, Georgalas I, et al. Intermediate results of sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2010;36(2):254-259.
- ↑ Elderkin S, Tu E, Sugar J, et al., Outcome of Descemet stripping automated endothelial keratoplasty in patients with an anterior chamber intraocular lens. Cornea. 2010;29(11):1273-1277.
- ↑ Fechner PU. Late loss of corneal endothelial density with refractive iris-claw IOLs. J Cataract Refract Surg. 2010;36(2):352-353.
- ↑ Hirashima DE, Soriano ES, Meirelles RL, et al. Outcomes of iris-claw anterior chamber versus iris-fixated foldable intraocular lens in subluxated lens secondary to Marfan syndrome. Ophthalmology. 2010;117(8):1479-1485.