Anterior Chamber Intraocular Lenses
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Surgical Therapy
Background
There are various techniques for intraocular lens (IOL) placement in patients without adequate zonular or capsular support. Some of these include anterior chamber IOL (ACIOL) with flexible open-looped haptics, anterior or posterior iris claw lenses, posterior iris sutured intraocular lenses, and sclerally-fixated posterior chamber IOLs (PCIOLs). ACIOLs with flexible open-looped haptics are one of the most frequently utilized lenses for this clinical situation.
Patient Selection
Indications
When capsular or zonular support is absent, an ACIOL can be placed if there is normal iris anatomy and a deep anterior chamber.
Contraindications
Some contraindications to ACIOL include pre-existing corneal endothelial damage, iridocorneal angle damage, shallow anterior chamber, or lack of sufficient iris support.
Surgical Technique
Sizing
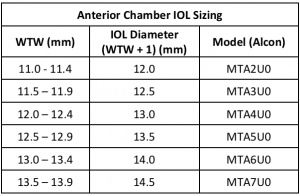
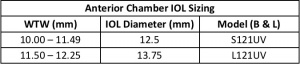
Earlier models of ACIOL were rigid and closed-loop. Modern ACIOL, with less frequent complications, are typically flexible and open loop with a supporting base at the end of each haptics. These haptics are inserted in the anterior chamber angle against the scleral spur, anterior to the iris[1]. Accurate measurement of the anterior chamber diameter is imperative for choosing the appropriately sized ACIOL. Different manufacturers have various sizing options. For example, Alcon anterior chamber intraocular lenses come in three sizes, while Bausch and Lomb anterior chamber lenses come in two different sizes. The most common method of sizing an ACIOL is by determining the white-to-white (WTW) diameter and adding 1mm; however, these estimations of angle position vary in accuracy depending on the anatomy of the patient. Additionally, the length varies depending on if the surgeon is sitting superiorly or temporally. Ultrasound biomicroscopy or other methods may be more reliable in determining the appropriate lens diameter but are still not consistently reliable[2][3].
Insertion Technique
Wound construction is important in placing an anterior chamber intraocular lens. Standard ACIOLs are made of PMMA and therefore are not foldable. The lens diameter is typically larger at 6mm, thus requiring a large 6mm incision. A scleral tunnel is often utilized, as it reduces corneal astigmatism from a larger corneal wound. While a corneal incision can be made, it can often result in significant irregular astigmatism [4].
Miostat or Miochol is often administered to constrict the pupil and pull the iris out of the angle prior to lens insertion. A peripheral iridotomy is created prior to lens insertion to avoid postoperative iris bombe or pupil block. A lens glide is often employed to assist in inserted of the ACIOL.
It is important that no iris tissue be incarcerated in the haptic loops. This can be ensured and helped by pulling each haptic loop centrally and anteriorly to seat the lens in the angle after it is completely inserted into the anterior chamber. If the pupil is peaked or oval, it is a sign that the iris is incarcerated in the haptic loops and should be repositioned.
Outcomes
ACIOLs have been associated with increased intraocular inflammation, pseudophakic bullous keratopathy, and uveitis/glaucoma/hyphema syndrome; however, newer, flexible, open-loop models have greatly improved outcomes when compared to older, inflexible closed-loop designs[5][6]. A retrospective analysis by Donaldson et. al compared ACIOL to sutured PCIOL and found no statistically significant difference in outcomes of best corrected visual acuity (BCVA) or complications [6]. But, another retrospective analysis by Kwong et al. comparing ACIOL to sclerally fixated PCIOL report superior outcomes in BCVA in the former group. Although further large prospective, randomized clinical trials are needed for definitive conclusions, the final treatment plan lies with surgeon preference and the unique characteristics of the patient[7][8]. In a review by the American Academy of Ophthalmology in 2003, it was determined that the literature supports the safe and effective use of open-loop ACIOLs, scleral-sutured posterior chamber IOLs, and iris-sutured posterior chamber IOLs for the treatment of aphakia in cases without adequate capsular support for placement of an IOL in the capsular bag or the ciliary sulcus[9].
Complications
Complications of ACIOLs are related to the proximity of structures to which the lens is placed. If the lens is not optimally sized and appropriately flexible, there is an increased chance of causing damage to the angle and iris, which can lead to chronic inflammation, elevated intraocular pressure, uveitis/glaucoma/hyphema syndrome, corneal endothelial damage and corneal decompensation.
References
- ↑ Por, Y. M., and M. J. Lavin. “Techniques of Intraocular Lens Suspension in the Absence of Capsular/Zonular Support.” Survey of Ophthalmology, vol. 50, no. 5, Jan. 2005, pp. 429–462. EBSCOhost, doi:10.1016/j.survophthal.2005.06.010.
- ↑ Hauff, W. “Calculating the Diameter of the Anterior Chamber before Implanting an Artificial Lens.” Wiener Klinische Wochenschrift, Supplement, vol. 171, pp. 1–19. EBSCOhost, search.ebscohost.com/login.aspx?direct=true&db=edselc&AN=edselc.2-52.0-0023085275&site=eds-live. Accessed 20 Oct. 2019.
- ↑ Wilczynski, Michal, et al. “Comparison of Internal Anterior Chamber Diameter Measured with Ultrabiomicroscopy with White-to-White Distance Measured Using Digital Photography in Aphakic Eyes.” EUROPEAN JOURNAL OF OPHTHALMOLOGY, vol. 20, no. 1, pp. 76–82. EBSCOhost, search.ebscohost.com/login.aspx?direct=true&db=edswsc&AN=000276361800011&site=eds-live. Accessed 20 Oct. 2019.
- ↑ Fine HF, Prenner JL, Wheatley M, et al. Surgical updates: Tips and tricks for secondary lens placement. Retina Today. Mar 2010:29-32.
- ↑ G.U. Auffarth, T.A. Wesendahl, S.J. Brown, D.J. AppleAre there acceptable anterior chamber intraocular lenses for clinical use in the 1990s? An analysis of 4104 explanted anterior chamber intraocular lenses Ophthalmology, 101 (1994), pp. 1913-1922
- ↑ Jump up to: 6.0 6.1 Donaldson, Kendall E., et al. “Anterior Chamber and Sutured Posterior Chamber Intraocular Lenses in Eyes with Poor Capsular Support.” Journal of Cataract & Refractive Surgery, vol. 31, no. 5, Jan. 2005, pp. 903–909. EBSCOhost, doi:10.1016/j.jcrs.2004.10.061.
- ↑ Kwong, Yolanda Y. Y., et al. “Comparison of Outcomes of Primary Scleral-Fixated versus Primary Anterior Chamber Intraocular Lens Implantation in Complicated Cataract Surgeries.” Ophthalmology, vol. 114, no. 1, Jan. 2007, pp. 80–85. EBSCOhost, doi:10.1016/j.ophtha.2005.11.024.
- ↑ Holt, Derick G., et al. “Anterior Chamber Intraocular Lens, Sutured Posterior Chamber Intraocular Lens, or Glued Intraocular Lens: Where Do We Stand?” CURRENT OPINION IN OPHTHALMOLOGY, vol. 23, no. 1, pp. 62–67. EBSCOhost, doi:10.1097/ICU.0b013e32834cd5e5. Accessed 19 Oct. 2019.
- ↑ M.D. Wagoner, T.A. Cox, R.G. Ariyasu, et al.Intraocular lens implantation in the absence of capsular support; a report by the American Academy of Ophthalmology (Opthalmic Technology Assessment) Ophthalmology, 110 (2003), pp. 840-859