Uveitis-Glaucoma-Hyphema Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
- Glaucoma secondary to other eye disorders H40.51X (right eye), H40.52X (left eye) H40.53X (bilateral)
- Mechanical complication of IOL implant T85.22X (displaced) or T85.23X (other)
- Lens-induced iridocyclitis H20.21 (right eye), H20.22 (left eye), H20.23 (bilateral)
Disease
Uveitis-Glaucoma-Hyphema (UGH) Syndrome or Ellingson syndrome is a complication of intraocular chafing from intraocular lens (IOL) implants leading to a spectrum of iris transillumination defects and pigmentary dispersion to microhyphemas and hyphemas with elevated intraocular pressure (IOP). It is most commonly caused by chafing from anterior chamber intraocular lenses but can occur from any type of pseudophakic lens. It is characterized by chronic inflammation, cystoid macular edema (CME), secondary iris neovascularization, recurrent hyphemas, and glaucomatous optic neuropathy leading to a loss of vision. Surgical intervention is often required as definitive treatment.[1]
History
The term UGH Syndrome was first coined by Ellingson in 1978.[2] He noticed that certain styles of anterior chamber intraocular lenses had warped footplates leading to a rocking motion of the lens and mechanical irritation of adjacent anterior chamber angle structures. The incidence of UGH has sharply declined due to refinement of lens design, IOL fabrication, IOL material, surgical techniques, and increased use of posterior chamber IOLs. As these factors changed, studies showed that the incidence of UGH syndrome decreased from a mean of 2.2 to 3% to 0.4 to 1.2% depending on the IOL type over a one-year period.[3]
Etiology
The disease is the result of mechanical irritation of anterior segment structures from an intraocular lens. This can also occur from cosmetic iris implants.[4]
Epidemiology
This entity can occur in any age group with an intraocular lens. While most commonly in elderly adults, it has been reported in the pediatric population.[5] Evidence of UGH occurring within 6 months of intraocular lens implant is consistently higher in anterior chamber lenses than in iris plane lenses than in posterior chamber lenses.[3] Single-piece acrylic IOLs placed within the sulcus tend to have a high UGH complication rate.[6]
General Pathology
Anterior chamber bleeding can be due to by peripupillary contact of iris with lens optic/haptics, and warpage of footplates or edge imperfections leading to mechanical irritation and erosion of uveal structures including the iridocorneal angle, iris, and ciliary body. This chafing can lead to a breakdown of the blood-aqueous barrier and subsequent release of pigment, red blood cells, protein, and white blood cells into the anterior chamber.[3] The release of red blood cells causes a microhyphema or hyphema. With pigment, red blood cells, and white blood cells in the anterior chamber, the trabecular meshwork can become blocked causing an increase in intraocular pressure. Additionally, contact with angle structures by the IOL can cause destruction of outflow structures and increased IOP. Electron microscopy of explanted IOLs often reveals melanosomes on the IOL, likely from damaged iris pigment epithelial cells.[7]
Prevention
Prevention of UGH syndrome is the main reason for the decreased incidence of the disease. During routine cataract surgery, a 1 piece lens and haptics should be placed within the lens capsule. If this is not possible due to intraoperative complications, then there are other lens types and techniques that should be undertaken to prevent uveal disruption from the intraocular lens. A 1 piece lens should not be placed in the sulcus.[6] If there is enough support a 3-piece lens should be placed within the sulcus. Additionally, reverse optic capture of the lens can be attempted by placing the edges under the anterior capsulorhexis.[6] It is important to place the 3 piece lens in the correct orientation within the sulcus as the lens is vaulted. If there is inadequate capsular support then a 3 piece sulcus lens can be fixated via scleral fixation. If an ACIOL is required then the correct size of the lens should be chosen. The general size for ACIOL placement is horizontal corneal white-to-white distance plus 1mm.[6] An incorrectly sized ACIOL can result in UGH syndrome via tilting and haptic chafing on anterior segment structures. The ACIOL is also vaulted and must be placed in the correct orientation. Upside-down lens syndrome[8] is characterized by 'chronic iritis, cystoid macular edema, pupil capture, iris adhesions, and corneal decompensation' due to inverted placement of the Kelman multiflex anterior chamber IOL.
There is an increased risk of corneal decompensation with an ACIOL which can create further complications.[9]
Diagnosis
The diagnosis of UGH Syndrome is clinical, based on history, physical exam, and supplemented by imaging.
Symptoms
Patients often present with intermittent decreased or blurred vision, intermittent white-out of vision, photophobia, redness, and ocular pain in the involved eye. The patient’s ocular discomfort may be out of proportion to ocular findings.
Signs
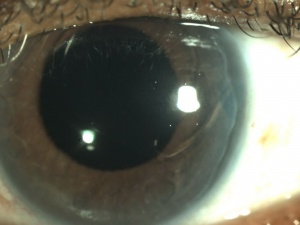
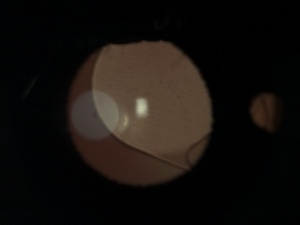
The examination can reveal a variety of physical exam findings. The ophthalmologist should look for the following signs on slit-lamp microscopy: raised IOP, microhyphema or hyphema, anterior chamber cells, and flare or hypopyon, iris neovascularization, iris-lens contact, iris transillumination defects, dislocated or malpositioned IOL, misplaced haptic, vitreous hemorrhage if the posterior capsule is not intact, and or CME. Examples of these can be seen in the figures to the right. Additionally, gonioscopy should be performed to look for blood within the angle, increased pigmentation of the trabecular meshwork, signs of mechanical erosion. Gonioscopy can also be used to aid in finding the haptic location that may be the cause of anterior chamber structure erosion.
Diagnostic procedures
Ultrasound biomicroscopy (UBM) is often used in the diagnosis of UGH syndrome to aid in the visualization of malpositioned IOLs and their contact with uveal tissue. The UBM probe should be used to confirm the position of haptics and optics and their relationships to surrounding ocular structures. This can help the clinician in reconfirming the clinical suspicion of UGH syndrome and aid in treatment decision-making.[7] Additionally, optical coherence tomography (OCT) can aid in the guidance of diagnosing CME; however, it is not needed to diagnose UGH syndrome itself.
Management
Treatment
IOL repositioning, explantation, and/or exchange successfully resolve recurrent episodes of hyphema or uveitis from UGH syndrome.[7] However, medical treatment of underlying signs/symptoms should be undertaken until definitive surgery can be undertaken:
- Uveitis: topical corticosteroids for control of anterior inflammation.[10]
- Intraocular Hypertension: IOP lowering topical and systemic medications such as prostaglandin analogs, beta-adrenergic antagonists, alpha-adrenergic agonists, and carbonic anhydrase inhibitors.[10] Parasympathomimetic agents, such as Pilocarpine, should be avoided due to its miotic effects and a possible increase in mechanical chafing to the iris.[7]
- Hyphema: limited activity, head elevation, cycloplegics for ciliary spasm or photophobia, and topical corticosteroids for associated inflammation.[11]
Additional Resources
References
- ↑ Foroozan R. Tabas JG, Moster ML. Recurrent microhyphema despite intracapsular fixation of a posterior chamber intraocular lens. J Cataract Refract Surg 2003;29:1632-5.
- ↑ Ellingson FT. The uveitis-glaucoma-hyphema syndrome associated with the Mark-VII Cloyce anterior chamber lens implant. Am Intraocular Implant Soc J. 1978;4:50.
- ↑ Jump up to: 3.0 3.1 3.2 Apple DJ, Mamlis N, Loftfield K, Googe JM, Novak LC, Kavka-van Norman D, Brady SE, Olson RJ. Complications of Intraocular Lenses. A Historical and Histopathological Review. Surv Ophthalmol 1984;29:1-54
- ↑ Arthur SN, Wright MM, Krammarevsky N, Kaufman SC, Grajewski AL. Uveitis-Glucoma-Hyphema Syndrome and Corneal Decompensation in Association with Cosmetic Iris Implants. Am J Ophthalmology 2009;148:790-3.
- ↑ Lin CJ, Tan CY, Lin SY, Jou JR. Uveitis-glaucoma-hyphema syndrome caused by posterior chamber intraocular lens—a rare complication in pediatric cataract surgery. Ann Ophthalmology 2008;40(3-4):183-4.
- ↑ Jump up to: 6.0 6.1 6.2 6.3 Chang DF, Masket S, Miller KM, Braga-Mele R, Little BC, Mamalis N, Oetting TA, Packer M. Complications of sulcus placement of single-piece acrylic intraocular lenses. Recommendations for backup IOL implantation following Posterior Capsule Rupture. J Cataract Refract Surg 2009;35:1445-58.
- ↑ Jump up to: 7.0 7.1 7.2 7.3 Piette S, Canlas O, Tran HV, Ishikawa H, Liebmann JM, Ritch R. Ultrasound Biomicroscopy in Uveitis-glaucoma-hyphema Syndrome. Am J Ophthalmology 2002;133:839-41.
- ↑ Fintelmann RE, Kim SK, Hwang DG. Upside-down lens syndrome: ocular complications secondary to inverted implantation of the Kelman Multiflex anterior chamber intraocular lens. Am J Ophthalmol. 2011 Jul;152(1):122-125.e2. doi: 10.1016/j.ajo.2011.01.025. Epub 2011 May 12. PMID: 21570051; PMCID: PMC5410585.
- ↑ Snellingen T, Shrestha JK, Huq F, Husain R, Koirala S, Rao GN, Pokhrel RP, Kolstad A, Upadhyay MP, Apple DJ, Arnesen E, Cheng H, Olsen EG, Vogel M. South Asian Cataract Management Study: complications, vision outcomes, and corneal endothelial cell loss in a randomized, multi-center clinical trial comparing intracapsular cataract extraction with and without anterior chamber intraocular lens implantation. Ophthalmology 2000;107:231–240
- ↑ Jump up to: 10.0 10.1 Eliassi-Rad B. Uveitic Glaucoma. EyeWiki. https://eyewiki.aao.org/Cataract. Accessed December 6, 2015.
- ↑ Oldham GW. Hyphema. EyeWiki. https://eyewiki.aao.org/Cataract. Accessed December 6, 2015.