Toric IOLs
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Entity
Toric IOLs refer to astigmatism correcting intraocular lenses used at the time of cataract surgery to decrease post-operative astigmatism.
Visit EyeSmart from the American Academy of Ophthalmology to learn more about astigmatism.
Patient Selection
The patient should have visually significant cataract and astigmatism. A good candidate will be interested in spectacle independence even if only for one focal point (usually distance). It should be made clear to the patient that correction (spectacle or contact lens) will be required for other distances (typically near and intermediate). Realistic expectations on the patient's part make for a successful outcome. Multifocal/extended depth of focus toric IOLs which may help in reducing spectacle dependance for near and or intermediate distance are also available.
Preoperative evaluation
The toric lenses currently available are designed to correct regular corneal astigmatism and are universally recommended in cases with preoperative corneal astigmatism of 1D (AMO Tecnis Toric package insert) or more. It is important to manage expectations as well as to perform a complete ophthalmic examination before offering a toric lens, as cases of irregular astigmatism caused by corneal scars or ectasia are not suitable candidates. Zonular instability, posterior capsular dehiscence, poor pupillary dilation and prior surgeries such as vitreoretinal procedures, bucking and glaucoma implants are all relative contraindications as the desired results may not be achieved. [1]
Available Toric IOLs
Standard toric IOLs are available in cylinder powers of 1.5D to 6.0D. They are usually intended for regular corneal astigmatism in a range from 0.75D to 4.75D and extended series or customized IOLs are available to achieve higher cylindrical power. [2] Toric IOLs are available as monofocal, enhanced monofocal and multifocal/EDOF lenses.
Monofocal lenses
The following are monofocal intraocular lenses. Patients will still require spectacle correction for other distances.
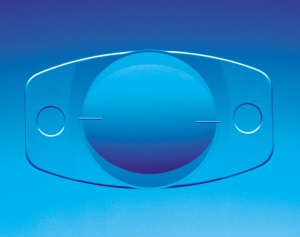
AcrySof and Clareon Toric IOLs (Alcon Labs, Fort Worth, Tx) (Figure 1) are a one-piece design, hydrophobic acrylic lens that comes clear or with a yellow chromophore. The optic is 6.0 mm. This lens can go through incision sizes as small as 2.2 mm. The IQ Toric version of this lens is aspheric and comes in the cylindrical powers as on the table below. They are able to correct up to +4.5 D of corneal astigmatism. The spherical range available is 6 to 30 D. The lens has 3 axis marking dots on either side of the optic periphery which designate the direction of the steep axis of toric power. These are aligned with the haptics for easy alignment.
| Model | Cylinder Power (D) | Cylinder Power (D) |
| at IOL plane | at Corneal Plane | |
| SN6AT3 | 1.50 | 1.03 |
| SN6AT4 | 2.25 | 1.55 |
| SN6AT5 | 3.00 | 2.06 |
| SN6AT6 | 3.75 | 2.57 |
| SN6AT7 | 4.50 | 3.08 |
| SN6AT8 | 5.25 | 3.60 |
| SN6AT9 | 6.00 | 4.11 |
Hoya iSert Toric 351 is a hydrophobic acrylic lens with PMMA haptics, which total size is 12.5 mm and optic size is 6.0 mm and can be inserted through a 2.2mm incision. Its spherical power goes from +10.0 D to + 30.0 D and cylindrical powers of +1.5 D to +6.0 D. [3]
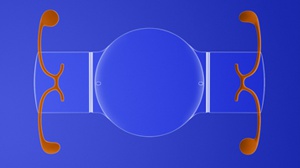
Staar Toric IOL (Staar Surgical, Monrovia, Ca) (Figure 2) is a silicone plate haptic design IOL. It can be implanted through a 3.0 mm clear corneal incision. As with all plate lenses, it should not be implanted in a compromised capsular bag. It is available in 2 models with differing lengths. Model AA4203-TF (10.8 mm in length) comes in spherical powers of 21.5 to 28.5 D. The AA4203-TL (11.2 mm) comes in spherical powers of 9.5 to 23.5 D. This lens comes in 2 cylindrical corrective powers: +2.0 D corrects corneal astigmatism of +1.2 to +1.4 D and the +3.5 D toric corrects +2.2 to +2.4 D of astigmatism. The axis of toric power is marked with 2 hash marks at the optic periphery. [4]
AMO Tecnis Toric IOL, Toric IOL II (Abbott Medical Optics, Inc, Santa Ana, CA) (Figure 3) is a one-piece design aspheric, hydrophobic acrylic IOL which was FDA approved in April 2013. It can be implanted through a 2.2 mm incision with the AMO Platinum inserter using the wound assist technique. It comes in 4 powers which can correct astigmatism from 0.75 diopters to 3.62 Diopters.
| IOL Model | Cylinder Power | Correction ranges based on combined corneal astigmatism (preop Kcyl + SIA) | |
| IOL Plane | Corneal Plane | ||
| ZCU150 | 1.50 | 1.03 | 0.75 - 1.50 D |
| ZCU225 | 2.25 | 1.54 | 1.50 - 2.00 D |
| ZCU300 | 3.00 | 2.06 | 2.00 - 2.75 D |
| ZCU375 | 3.75 | 2.57 | 2.50 - 3.00D |
| ZCU450 | 4.50 D | 3.08 | 3.00-3.50D |
| ZCU525 | 5.25 D | 3.60 | 3.5- 4.00 D |
| ZCU600 | 6.00D | 4.11 | 4.00-4.75 D |
EnVista toric IOL (Model MX60T) (Bausch + Lomb, Bridgewater, N.J.) This lens is an aspheric, aberration-free, biconvex, posterior-surface toric with an optic size of 6 mm. The cylinder powers in the IOL plane ranges from +1.25 to +5.75 D and +0.90 to +4.03 D in the corneal plane. The recommended incision size is 2.2 mm. [5]
Multifocal lenses
The advantage of the multifocal lenses is in addition to astigmatic correction they also provide extended range of vision including near, intermediate and far.
TECNIS Presbyopia correcting IOLs (Symfony Toric and Odyssey Toric) (Abbott Medical Optics, Inc, Santa Ana, CA) are biconvex lenses with wavefront-designed anterior toric aspheric surface. Tecnis OptiBlue toric IOLs ae, wavefront-designed anterior aspheric surface and achromatic technology to correct chromatic aberration for enhanced image contrast. These are a one-piece lens 5.0 D-34 D increment of 0.50 D with cylindrical power of 1.5D-3.75D : [6]
Model DXW150, DRT150: 1.50 D (IOL plane), 1.03 D (corneal plane)
Model DXW225, DRT225: 2.25 D (IOL plane), 1.54 D (corneal plane)
Model DXW300, DRT300: 3.00 D (IOL plane), 2.06 D (corneal plane)
Model DXW375, DRT375: 3.75 D (IOL plane), 2.75 D (corneal plane)
AcrySof® and Clareon presbyopia correcting Toric IOLs include (Alcon, Fort Worth, TX) Panoptix Trifocal Toric and Vivity non-diffractive extended depth of focus Toric IOL This hydrophobic lens has a spherical power of +6.0 to + 34.0 D ( Vivity IOL start 15D and up) and cylinder power of 1.0 to 3.0 D. The lens is foldable with the toric component incorporated on the posterior surface. Since the lens is biconvex and foldable, it can be implanted through a relatively small incision. [7]
Trulign Toric IOL (Bausch + Lomb, Bridgewater, N.J.) (Figure 4) is a modified plate haptic aspheric silicone accommodating IOL. The axis marks align with the flat meridian of the lens. The lens comes in 3 powers at the IOL plane: 1.25, 2.00 and 2.75 D (which correspond with the following powers at the corneal plane 0.83, 1.33 and 1.83 D respectively). This lens is available in spherical powers ranging from 10 D to 33 D in 0.5 D steps. The Trulign Toric IOL can reduce astigmatism and offers presbyopic correction as well. [8]
Diagnostic procedures
Accurate determination of the amount of astigmatism is paramount. Astigmatism can be further defined as refractive, lenticular and corneal. A careful manual refraction is key to determining refractive astigmatism. Corneal astigmatism is usually measured with keratometry and/or topography. Cylinder and axis are confirmed on manual keratometry, K's on an optical biometer such as an IOL Master or Lenstar LS 900 and corneal topography. All measurements should be similar in both direction and magnitude of astigmatism. It is crucial to differentiate the lenticular contribution to the total astigmatism. The patient will be undergoing cataract surgery so only the corneal astigmatism will need to be addressed.
Other considerations
The cataract corneal incision may induce astigmatism. Surgeons should consider the impact of their incision size and location on the cornea as it will determine the final residual corneal astigmatism. The Alcon online toric calculator (www.AcrySofToriccalculator.com) takes into account the effect of the main incision-induced astigmatism on the final recommended cylindrical power and the appropriate axis of IOL orientation.
Management
IOL Calculations
Surgeons should perform IOL calculations as per routine. This will determine the spherical power needed. Each surgeon is advised to use their preferred IOL formula.
Determination of Toric power required
For the Alcon AcrySof models, the surgeon can log on to the online toric calculator (www.AcrySofToriccalculator.com) and input the required information. The calculator will then determine the best model and the axis of orientation of the lens. Surgeons will find that, depending on the amount of main corneal incision induced astigmatism and the location of the incision, the toric power may change. Surgeons are encouraged to input varying main incision sites to consider their effect. Those surgeons who are more flexible about where they place their main incision may find they are able to correct higher astigmatism powers.
Staar Surgical also offers an online toric calculator (www.STAARToric.com). Again, the surgeon determines the spherical power as per routine IOL calculations methods. Corneal astigmatism will determine which of the two powers should be used. For corneal astigmatism from 1.4 to 2.3 D, Staar Surgical recommends the +2.5 D power and the +3.5 D toric for astigmatism above +2.3D.
Abbot Medical Optics has its own online calculator (www.tecnistoriciol.com/tecnis-toric-iol-calculator). This calculator gives the user a variety of options, including those that induce residual astigmatism on a different axis. It is imperative to check the orientation of the axis as well as the power of the suggested toric when using this calculator.
Bausch + Lomb also provides online resources (envista.toriccalculator.com). This calculator requires you to input keratometry information as well as incision location and IOL mean sphere power.
Surgery
Prior to beginning the surgical procedure, the precise reference marking of the cornea is done with the patient upright and looking forward. It is important that the patient is sitting for this procedure as cyclotorsion may occur when the patient lies down. The cornea is marked at the 3, 6- and 9-o'clock positions after instillation of a topical anesthetic. Some surgeons select to simply mark 3- and 9-o'clock. This can be done in the preoperative area or in the operating room. Corneal marking instruments are available which ease this step. This can also be marked with a skin marking pen.
After the patient is draped, the steep axis should be marked with a degree gauge so as to provide a guide for the orienting marks on the toric IOL later in the procedure. It is wise to double-check the axis with preoperative notes.
Then, the surgeon proceeds with the surgery as per routine.
IOL IMPLANTATION:
At this step, an ophthalmic viscoelastic device (OVD) is injected into the capsular bag. Cohesive OVDs e.g. Healon (AMO) or Provisc (Alcon) are preferred over the dispersive agents. Cohesive OVDs are less likely to coat the IOL surface and are easier to remove at the end of the case.
At this time, the toric IOL should be grossly aligned about 10-15 degrees counterclockwise of the final desired lens position. Viscoelastic is then carefully removed from behind the lens followed by anterior to the lens. The IOL may be secured in position with a second instrument if desired. Occasionally, during this step, the IOL may rotate the 10-15 degrees needed into position. If not, a second instrument is used to rotate it into the final position. When appropriately oriented, a gentle nudge posteriorly will hold it there securely. This step increase IOL contact with the posterior capsule, decreasing the incidence of postoperative rotation. If the IOL over-rotates, viscoelastic should be injected into the eye and the above steps repeated as it can only be rotated clockwise. Some IOLs use an acrylic material is 'tacky' that allows it to remain aligned on axis.
The procedure for the implantation of the STAAR toric is similar. It should be grossly aligned upon insertion into the capsular bag. A couple of pearls to prevent postoperative rotation are as follows. Thorough OVD removal is critical. Again, the surgeon should pay particular attention to OVD trapped behind the IOL. This maximizes IOL-posterior capsule contact which minimizes undesired rotation. The manufacturer also recommends the eye should be left a little 'softer' than usual.
A key point for all toric IOL models is that the OVDs must be completely removed from the eye and beneath the IOL at the end of the case to prevent rotation.
Some surgeons hydroimplant toric IOL (while the irrigation cannula of bimanual IA is inside the anterior chamber through the side port) after a complete removal of OVDs.
For higher amounts of astigmatism, a combination of a Toric IOL and astigmatic keratotomy may be the best means to address the total amount of cylinder.
Image-guided techniques
Iris-fingerprinting has been used since 2010. This technology utilizes iris crypts, nevi, and Brushfield spots as landmarks to place axis marks. Various image-guided systems exist, which include the CALLISTO Eye and Z design, VERION and TrueVision Surgical System. [9] [10] The iTRACE system and the Zaldivar toric Caliper Tool allow you to calculate the locations of the marks and their distance in degrees from the target IOL axis. Image-guided systems involve superimposed preoperative measurements and intraoperative images to provide a guide for toric IOL alignment. Intraoperative aberrometry can also be useful for IOL alignment; ORA (WaveTec Vision Systems Inc, CA, USA) and Holos IntraOp (Clarity Medical Systems, CA, USA) are used for real-time assessment of IOL toric alignment. [1]
Surgical follow up
Postoperative exams should be as for routine cataract extraction/IOL implantation cases. Most surgeons customarily see their patients on postoperative day #1, #7, and #28. Postoperative drop regimen is as per routine for uncomplicated cataract surgeries. An antibiotic, NSAID and steroid drops are part of most postoperative regimens.
Non-Surgical Options
Patients may elect to treat astigmatism with corrective lenses (spectacle or contact).
Complications
In addition to the usual complications associated with cataract extraction with intraocular lens implantation surgery, toric IOLs have a few other potential complications. Astigmatism may be overcorrected or undercorrected.
The toric IOL may rotate off-axis. There will be some partial effect if it rotates off-axis. For example, the correction effect of the AcrySof toric is reduced by 10% for every 3o rotation off-axis. For the lens to lose its full effect, it would have to be off-axis by 30o. Prevention of IOL rotation includes complete removal of OVDs, especially posterior to the IOL.
Prognosis
The vast majority of patients do extremely well when careful attention is paid to patient and lens selection and surgical technique. The technical surgical learning curve for the surgeon is fairly minimal for an outcome that is reliably predictable. Toric IOLs, exclusively or in conjunction with astigmatic keratotomy and/or strategic cataract incision placement, can result in excellent management of astigmatism and should be considered for astigmatic patients who desire spectacle freedom at distance.
Additional Resources
- www.lricalculator.com
- https://trulign.toriccalculator.com/
- Boyd K, Edmond JC. Astigmatism. American Academy of Ophthalmology. EyeSmart</Eye health. https://www.aao.org/eye-health/diseases/astigmatism-4. Accessed March 27, 2019.
- Yeu E. Intraocular Implants (IOLs). American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/treatments/intraocular-implants-iols. Accessed March 13, 2019.
References
- ↑ 1.0 1.1 Kaur M, Shaikh F, Falera R, Titiyal JS. Optimizing outcomes with toric intraocular lenses. Indian J Ophthalmol. 2017;65(12):1301-1313.
- ↑ Khan MI, Ch’ng SW, Muhtaseb M. The use of toric intraocular lens to correct astigmatism at the time of cataract surgery. Oman J Ophthalmol. 2015;8:38–43.
- ↑ https://hoyasurgicaloptics.com/html/page.php?page_id=7&pid=3&pc_mode_20=details
- ↑ http://db.staar.com/products/toric-iol/
- ↑ https://www.bauschsurgical.eu/products/cataract/intraocular-lenses-monofocal-and-premium/envista-toric/
- ↑ http://www.precisionlens.net/tecnis-symfony-toric-extended-depth-of-focus-iol-model-zxt
- ↑ https://www.myalcon.com/professional/cataract-surgery/intraocular-lens/acrysof-iq-restor-multifocal-iol/restor-30/data-support
- ↑ http://www.bausch.com/ecp/our-products/cataract-surgery/lens-systems/trulign-toric-iol
- ↑ Onishi H, Torii H, Watanabe K, Tsubota K, Negishi K. Comparison of clinical outcomes among 3 marking methods for toric intraocular lens implantation. Jpn J Ophthalmol. 2016;60:142–9.
- ↑ Osher RH. Iris fingerprinting: New method for improving accuracy in toric lens orientation. J Cataract Refract Surg. 2010;36:351–2.