Pediatric Low Vision
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Pediatric low vision is defined as irreversible vision loss or permanent visual impairment in a person younger than 21 years old, which cannot be improved with refractive correction, medical treatment, or surgical intervention.[1] Pediatric low vision can result in challenges with reaching developmental milestones, obstacles with achieving educational goals, difficulty with social interactions, and loss of independence. In the pediatric population, low vision may be mistaken for intellectual disability and behavioral disorders, and may be masked by concomitant systemic health issues that obscure its diagnosis. Therefore, a keen understanding of how to detect and manage pediatric low-vision can have an important and lifelong impact on this vulnerable patient population.
Definition of Pediatric Low Vision
Pediatric low vision, as defined by the American Academy of Ophthalmology’s Preferred Practice Patterns for Vision Rehabilitation, is irreversible vision loss or impairment in a person under 21 years old, which cannot be improved with refractive correction, medical treatment, or surgical intervention.[1] Specific parameters include a best-corrected visual acuity (BCVA) of 20/40 (the minimal visual acuity required for driving in many states) or worse in the better-seeing eye.[2] Low vision can also be characterized as a BCVA of 20/30 or worse if contrast sensitivity is lower than 1.4 log units in an individual performing everyday tasks such as reading, driving, or recognizing faces.[3]
Causes of Pediatric Low Vision
The etiologies for low vision in the pediatric population are many and varied. For example, pediatric low vision may be due to a primary ocular structural abnormality, or secondary to other ocular pathology. It may develop as one of the ophthalmologic manifestations of a genetic or systemic syndrome, or may occur as a result of cerebral visual impairment (CVI). Limited epidemiologic data to date cite nystagmus, optic atrophy, optic nerve hypoplasia, and CVI as some of the most common causes of pediatric low vision.[4]
Structural abnormalities affecting any part of the eye, from front to back, may contribute to pediatric low vision. Examples include, but are not limited to, the following: corneal opacification, congenital cataract, primary aphakia, chorioretinal coloboma, optic nerve hypoplasia, and foveal hypoplasia. Ocular pathology such as limbal stem cell deficiency, congenital nystagmus, aniridia, retinal dystrophy, trauma, and iatrogenic damage can result in, or contribute to, low vision.[1][4]
The list of genetic and systemic conditions associated with pediatric low vision is extensive. Some of the more common syndromes include Leber congenital amaurosis, Stargardt disease, Retinitis Pigmentosa, Achromatopsia, and ocular or oculo-cutaneous albinism. Other less common but well-known syndromes that may be associated with pediatric low vision include, Axenfeld-Rieger, Bardet Biedl, CHARGE, Hurler, Lowe, Stickler, Sturge Weber, and Usher syndrome. A more extensive list of genetic conditions and their ocular manifestations leading to low vision can be found in Table 1.[5][6]
Table 1. Genetic and systemic syndromes associated with pediatric low vision[5][6]
| Genetic or system condition | Ocular manifestations contributing to low vision |
|---|---|
| Leber congenital amaurosis | nystagmus, high hyperopia, reduced accommodative capacity, photophia |
| Stargardt disease | central vision loss, photophobia, color vision deficit, delayed and/or reduced dark adaptation |
| Retinitis Pigmentosa | night blindness, progressive peripheral visual field restriction, tunnel vision |
| Achromatopsia | reduced BCVA, impaired color vision, photophobia, nystagmus |
| Oculo-cutaneous albinism | optic nerve and/or foveal hypoplasia, nystagmus, strabismus, photophobia, refractive error |
| Axenfeld-Rieger Syndrome | correctopia, polycoria, glaucoma |
| Bardet-Biedl Syndrome | delayed and/or reduced dark adaptation, photophobia, loss of central and color vision |
| CHARGE Syndrome | chorioretinal coloboma, cataract, ptosis, strabismus, microphthalmia, microcornea |
| Hurler Syndrome | corneal clouding, retinal pigmentary degeneration, optic nerve head swelling, glaucoma |
| Lowe Syndrome | congenital cataract, corneal keloid, infantile glaucoma |
| Stickler Syndrome | optically empty vitreous, retinal tear or detachment, pathologic myopia |
| Sturge Weber Syndrome | choroidal hemangioma, glaucoma |
| Usher Syndrome | night blindness, progressive peripheral visual field loss |
CVI in the absence of other ocular disease, may also be associated with pediatric low vision.[1] CVI most commonly presents due to pre- or perinatal hypoxia, and can also be seen in the setting of some genetic syndromes.[7][8] CVI results from retrograde transsynpatic degeneration causing damage to the anterior visual pathways.[7][8] This damage most often manifests as visual field defects, reduced contrast sensitivity, and loss of visual acuity. Other ocular manifestations that compouond CVI include refractive error, and optic atrophy.[7][8]
Signs of Low Vision in Children
A child’s visual development is marked by specific milestones. From birth to approximately four months of age, an infant begins adjusting to light and focusing on objects in front of them.[9] From five to eight months depth perception and facial recognition become part of a child’s visual behavior. From nine to twelve months, babies begin to demonstrate hand-eye coordination and gross spatial recognition as they become mobile with crawling.[9] These skills build through the first two years of life allowing children to explore other objects of interest in their environment such as toys and foods.[9]
Knowing the key steps in normal visual development for each age group is therefore crucial in detecting early signs of delayed visual development. Table 2 outlines the signs of normal and delayed visual development according to a child’s age.[9][10] Decreased sensitivity to bright lights, delayed or absent eye contact, slowed development of an intentional social smile, lack of awareness of an infant’s own hands, the absence of goal-directed hand movements, and failure to fixate on familiar objects such as toys and faces may all be warning signs to the parents and/or the pediatrician of low vision.[9][10]
Table 2. Signs of normal and impaired visual development according to age
| Age | Normal visual development | Signs of possible visual impairment |
|---|---|---|
| Birth-4 months | Focusing on and tracking familiar objects | Decreased sensitivity to bright light, absent or delayed blink reflex to threat or light, slowed development of intentional social smile, nystagmus |
| 5-8 months | Depth perception, facial recognition, color vision | Delayed or absent eye contact, failure to fixate on objects or familiar faces, strabismus |
| 9-24 months | Hand-eye coordination, grasping objects, crawling | Lack of awareness of own hands, absence of goal directed hand and/or arm movements |
| >24 months | Crawling, walking, exploring the environment | Clumsiness with crawling, difficulty reaching toys, holding objects close to the face, problems navigating curbs or steps |
| School-age | Reading | Difficulty with reading, complaints of headache |
Once children become mobile, signs of low vision may be more obvious due to clumsiness with crawling, difficulty reaching for toys, and holding objects very close to the face. Older children may start to verbalize symptoms of blurry vision, eye strain or headaches.[1][9][10] As gross and fine motor skills develop hand-in-hand with visual processing, any delays in motor development should warrant an eye exam to rule out concomitant low vision.[1] By school age, children with low vision may present with difficulty in tasks such as reading, which may be mistaken for a learning disability.
Evaluation of Low Vision in Children
Children should be referred for low vision assessment as early as possible. Most commonly, children are referred to ophthalmology around school age or once they are old enough to vocalize symptoms of blurry vision.[11] Some parents seek earlier ophthalmologic evaluation when they notice that their child’s visual behavior is abnormal or delayed. The components and order of the pediatric low vision exam vary depending upon the age of the child and their ability to participate. The overarching goal of the pediatric low vision exam is to obtain as much information as possible regarding the child’s visual function and identify the cause for the low vision.
History
Taking time to obtain a thorough history regarding onset, severity and progression of low vision symptoms is critical. If the child is old enough, it is important to involve them as much as possible to encourage self-advocacy from an early age. For many patients, this will become increasingly important as they learn to protect their independence as their vision declines. In addition to standard history questions regarding timing of onset, severity, and progression of visual symptoms, the following components should be included in the pediatric low vision history:
- Family history of visual impairment
- Degree of impairment the child has in day-to-day activities
- Impact of visual symptoms on the child’s wellbeing and psychosocial functioning
- Prior use of low vision aids, including spectacles
- Difficulty with near tasks and mobility.
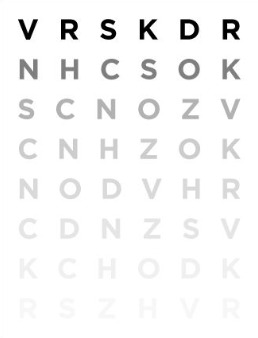
Visual Acuity
Visual acuity should always be measured with the child’s age, school performance, and cognitive ability in mind.[11] Gold standard low vision acuity testing requires near and distance logMAR testing using age appropriate optotypes (Figure 1).[11][12][13] Single line testing may overestimate visual acuity compared to the full chart test; however full chart tests may cause “crowding phenomenon” or “contour interaction”, both of which can falsely underestimate results.[11][12][13] Near vision testing may be more reflective of the child’s functional vision, and in many cases may be the only option if the child is unable to identify the largest optotype at a distance.
Assessment according to age
1. 0-36 months: Teller Acuity Cards are the gold standard for visual acuity testing in this age group and have been validated for children with low vision.[13][14] Teller acuity cards rely on the patient’s behavior and eye movements in response to being shown a series of cards with different gratings.[15]
2. 4-7 year old: LEA symbols have been validated for pre-literate children.[12][13] Landolt C or HOTV optotypes can be alternate options for older children who have started to learn letters, but may not know the alphabet consistently well enough to perform Snellen testing.[12][13]
3. 8-13 year old: The LogMAR chart is the best option for children with low vision who are literate.[13]
Visual Fields
Visual field assessment in young children can be difficult. Nonetheless, results are important for understanding the impact of low vision on a child’s mobility and visuo-spatial orientation.
Confrontation visual fields: Testing should be performed by having the child focus on a central object, while moving colorful targets into the peripheral field. How far the peripherally moving objects travel before the child notices them is the border of the visual field.
Kinetic perimetry: In cooperative children over approximately 6 years old, Goldman visual field testing is preferable for objective delineation of any field loss and for detecting the presence of visual scotomas.[10][16]
Standard automated perimetry: For children who are able to participate in automated field testing, machines such as the Humphrey Visual Field or Octopus can provide accurate results faster than manual kinetic perimetry.
Contrast Sensitivity
Results of contrast sensitivity testing may provide insight into a discrepancy between a child’s formal visual acuity testing and their day-to-day visual functioning, as decreased contrast sensitivity may correlate with poor visual functioning despite relatively intact visual acuity.[10]
Hiding Heidi Low Contrast Face Test: Consists of four charts with contrast levels of 1.25%, 2.5%, 5%, 10%, 25%, 100%, and a blank card (Figure 1). Children are presented with two cards, one blank and another a cartoon face at a specific contrast level. Children are asked to identify which card has the cartoon image.[17] A demonstration of how this test is performed is depicted in the video below.
Pelli-Robson test: A chart with Snellen letterns of a standard size and presented in varies degrees of contrast. For older children, this test can be performed at a distance of 1 meter (Figure 2).[18]
Color Vision
Assessing a child’s color vision may help explain difficulties with object recognition, as well as anticipate future challenges with schoolwork. Red/green color vision is evaluated using the Ishihara test.[10] Other validated color vision tests for children with reduced visual acuity include the Farnsworth D-15 test, or the abbreviated Mollon-Reffin minimalist (MRM) test.[10][16][19] The Color Vision Testing Made Easy can evaluate for red/green deficits as early as 4 years of age. [20][21]
Refraction and Accommodative Capacity
Cycloplegic refraction, while included in any pediatric eye exam, is especially important in the pediatric low vision evaluation as this population has a high incidence of refractive error. In addition, even minor refractive correction can lead to improved quality of vision and visual functioning. Polycarbonate lenses are prescribed for the added benefit of eye protection. Lastly, dynamic retinoscopy prior to cycloplegia can be used to evaluate the child’s accommodative capacity, which if impaired, may prompt the addition of bifocal correction to aid with near work at school and near leisure activities.[10]
Additional Testing
In many instances, additional testing may be pursued to collect both anatomic and functional information about the child’s visual system. Such tests may include ocular coherence tomography (OCT) of the optic nerve and/or macula, electroretinogram (ERG), and visual evoked potential (VEP). Depending on the test and age of the child, sedation or general anesthesia may be required.
Management of Pediatric Patients with Low Vision
The approach to management will vary depending on the child’s age and level of visual impairment. Fortunately, there is a wide array of tools available from in-person approaches to advanced technology. An interdisciplinary team, with special attention to the psychosocial impact of low vision on a child, is critical for comprehensive and effective care. Low vision services help alleviate restrictions in social activities, sports, and other hobbies or leisure activities, thereby helping to improve quality of life.
An Interdisciplinary Team
May include, but are not limited to, a combination of the following:[22]
1. Pediatric ophthalmologist
2. Optometrist
3. Occupational therapist
4. Vision rehabilitation therapist
5. Assistive technology trainers
6. Orientation and mobility specialist
7. Psychologist
8. Vocational counselors
Near Vision Aids
Children who have poor near vision will often move closer and adopt an unnatural body position to view objects in more detail. This can be problematic overtime, as they can develop poor posture and strain on their neck. They may benefit greatly from a number of optical low vision devices to enhance their near vision including single vision spectacle magnifiers, hand-held or stand magnifiers, and monocular telescopes.[23]
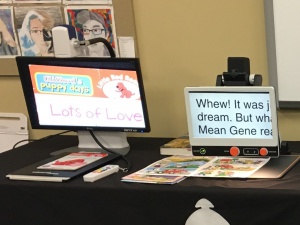
Electronic Low Vision Devices
Video magnifiers (or closed-circuit television) systems use a mounted or handheld camera to project a magnified image onto a separate screen. They are ergonomically sound and offer the highest degree of magnification, but their cost may be prohibitive.[23] Smartphone applications, as well as artificial intelligence technology, have contributed significantly to the available assistive technology for individuals of all ages with low vision. For example, Siri and Alexa, operate using voice recognition and do not require visual cues or interaction. Audiobooks, screen readers for email and audio conversion for text messaging, are additional resources that can significantly impact individuals of all ages living with low vision. The American Foundation for the Blind offers a list of low vision assistive technology.
Glare Control
Individuals with low vision often experience photophobia for which tinted lenses both for near and distance can be prescribed. Tinted lens can also come in different colors to provide contrast enhancement of objects in the environment. Furthermore, children who are sensitive to glare may benefit from glasses with special absorptive filters and side shields to filter out glare-producing light.[23][24]
Assistance with Activities of Daily Living (ADLs)
It is critical that children with low vision foster independence with ADLs from a young age. At home, consistent placement of items surrounding food preparation, self-hygiene, and dressing can help a child develop systems for ADLs independent of visual cues. For children who have received instruction in braille, labeling of household items can help with certain tasks. At school, large print books, adaptive technology, bolded writing, sloped desks for closer working distance, optimal illumination, and even tablet/e-readers with font enlargement can enhance a child’s learning experience.[23]
In both the home and school settings, occupational therapists can play a central role in helping a child with low vision optimize their gross and fine motor abilities to maximze ADL independence.
Psychological Impact of Low Vision on Children
Children with low vision have a reportedly higher incidence of mental health concerns compared to their sighted peers.[25] Triggers may include reduced mobility, greater dependency on caretakers for daily activities, limited participation in leisure activities, and fewer opportunities for social development with peers.[25] Moreover, visual impairment can hinder a child’s ability to read facial expressions and learn to predict people’s behaviors, contributing to increased social isolation.[26][27]
Early detection of mental health concerns in children with low vision is crucial. Impaired mental health in children, unlike adults, may manifest with somatic symptoms such headaches, nightmares, irritable mood, or changes in cognition.[25] Social support from family, teachers and friends, professional counseling, and a focus on maintaining a child’s independence are key to addressing mental health concerns. Furthermore, inclusion of the child in his or her own care as much as possible from a very young age is critical for optimizing low vision care. Children with low vision should be given the tools to learn how to advocate for themselves to further promote their independence and overcome future obstacles that they are likely to encounter during a lifetime with low vision.
Treatment Outcomes
There is well-documented evidence that gains in visual acuity, enhanced visual functioning, improved quality of life, and stronger academic performance in children can be achieved with appropriate and comprehensive low vision management.[28][29] Furthermore, early intervention with low vision services is associated with improved outcomes compared to low vision support initiated at school age.[28][29]
Evidence in the literature evaluating treatment outcomes following low-vision rehabilitation services for children is lacking and reports are largely limited to small studies or case series.[30][31] Available data confirm that a majority of children receiving mobility and orientation training demonstrate gains in food preparation skills, home management, orientation and mobility, and shopping skills.[31] With regards to fine-motor tasks, a study of 4-5 year old children were found to have improvement in performance speed and accuracy of a number of fine-motor exercises after twelve sessions of training with a stand magnifier.[30]
Knowledge and data surrounding low vision in children is growing. This area within pediatric ophthalmology clearly remains one of great interest and need.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Fontenot JL, Bona MD, Kaleem MA, et al. Vision Rehabilitation Preferred Practice Pattern®. Ophthalmology. 2018;125(1):P228-P278.
- ↑ Shah P, Schwartz SG, Gartner S, Scott IU, Flynn HW. Low vision services: a practical guide for the clinician. Ther Adv Ophthalmol. 2018;10:251584141877626.
- ↑ West SK, Rubin GS, Broman AT, et al. How Does Visual Impairment Affect Performance on Tasks of Everyday Life?: The SEE Project. Arch Ophthalmol. 2002;120(6):774-780.
- ↑ 4.0 4.1 Wilkinson ME, Trantham CS. Characteristics of children evaluated at a pediatric low vision clinic: 1981-2003. J Vis Impair Blind. 2004;98(11):693-702.
- ↑ 5.0 5.1 Lambert S and Lyons C. Taylor and Hoyt’s Pediatric Ophthalmology and Strabismus. Ed 5:Elsevier;2017.
- ↑ 6.0 6.1 Hered Rw (Ed). 2019-2020 BSCS (Basic and Clinical Science Course), Section 06: Pediatric Ophthalmology and Strabismus.
- ↑ 7.0 7.1 7.2 Fazzi E, Signorini SG, Bova SM, et al. Spectrum of visual disorders in children with cerebral visual impairment. J Child Neurol. 2007;22(3):294-301.
- ↑ 8.0 8.1 8.2 Bosch DGM, Boonstra FN, Willemsen MAAP, Cremers FPM, De Vries BBA. Low vision due to cerebral visual impairment: Differentiating between acquired and genetic causes. BMC Ophthalmol. 2014;14(1):1-9.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Keirstan B. Baby’s Vision Development: What to Expect the First Year. https://www.aao.org/eye-health/tips-prevention/baby-vision-development-first-year. Accessed May 20, 2020.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 Hyvärinen L, Walthes R, Jacob N, et al. Delayed Visual Development: Development of Vision and Visual Delays. https://www.researchgate.net/publication/292681903. Accessed July 20, 2020.
- ↑ 11.0 11.1 11.2 11.3 Randeree J, Speedwell L. Paediatric low vision. https://assets.markallengroup.com/article-images/image-library/147/uploads/importedimages/paediatric-low-vision-2.pdf. Accessed July 20, 2020.
- ↑ 12.0 12.1 12.2 12.3 Morad Y, Werker E, Nemet P. Visual acuity tests using chart, line, and single optotype in healthy and amblyopic children. J AAPOS. 1999;(April):94-97.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Huurneman B, Boonstra FN. Assessment of near visual acuity in 0-13 year olds with normal and low vision: A systematic review. BMC Ophthalmol. 2016;16(1):1-15.
- ↑ Preston KL, Mcdonald M, Sebris SL, Dobson V, Teller DY. Validation of the Acuity Card Procedure for Assessment of Infants with Ocular Disorders. Ophthalmology. 94(6):644-653.
- ↑ Citation for Teller Acuity Card Image
- ↑ 16.0 16.1 Hyvarinen L. Considerations in Evaluation and Treatment of the Child With Low Vision. Am J Occup Ther. 1995;49:891-897.
- ↑ Citation for Hiding Heidi Low Contrast Face Test
- ↑ Citation for Pelli Robson Chart Image
- ↑ Pf OA, Hanson JVM, Gerth-kahlert C. Colour vision testing in young children with reduced visual acuity. Acta Ophthalmologica. 2020;(Dain 2004):113-120.
- ↑ Xie JZ, Tarczy-Hornoch K, Lin J, Cotter SA, Torres M, Varma R; Multi-Ethnic Pediatric Eye Disease Study Group. Color vision deficiency in preschool children: the multi-ethnic pediatric eye disease study. Ophthalmology. 2014 Jul;121(7):1469-74. doi: 10.1016/j.ophtha.2014.01.018. Epub 2014 Mar 16. PMID: 24702753; PMCID: PMC4839481.
- ↑ Cotter SA, Lee DY, French AL. Evaluation of a new color vision test: "color vision testing made easy". Optom Vis Sci. 1999 Sep;76(9):631-6. doi: 10.1097/00006324-199909000-00020. PMID: 10498004.
- ↑ Rainey L, Bernadette E, Elsman M, et al. Comprehending the impact of low vision on the lives of children and adolescents: a qualitative approach. Qual Life Res. 2016;25(10):2633-2643.
- ↑ 23.0 23.1 23.2 23.3 Lee SM, Cho JC. Low vision devices for children. Community eye Heal. 2007;20(62):28-29.
- ↑ WHO Programme for the Prevention of Blindness. Management of low vision in children: report of a WHO consultation. World Health Organization. https://apps.who.int/iris/handle/10665/61105. Accessed July 20, 2020.
- ↑ 25.0 25.1 25.2 Augestad LB. Mental Health among Children and Young Adults with Visual Impairments: A Systematic Review. J Vis Impair Blind. 2017;(October):411-425.
- ↑ Pinquart M, Pfeiffer JP. Identity development in German adolescents with and without visual impairments. J Vis Impair Blind. 2013;107(5):338-349.
- ↑ Labib TA, Sada MA El, Mohamed B, Sabra NM, Aleem HMA. Assessment and Management of Children with Visual Impairment. Middle East Afr J Ophthalmol. 2009;16(2):64-69.
- ↑ 28.0 28.1 Ganesh S, Sethi S, Srivastav S, Chaudhary A, Arora P. Impact of low vision rehabilitation on functional vision performance of children with visual impairment. Oman J Ophthalmol. 2013;6(3):170-175.
- ↑ 29.0 29.1 Kavitha V, Heralgi MM, Parkar M HS. Quality of life in children with low vision following use of low vision aids. Taiwan J Ophthalmo. http://www.e-tjo.org/preprintarticle.asp?id=251057. Accessed July 20, 2020.
- ↑ 30.0 30.1 Miller J. The use of self-reports and parent observations in assessing performance outcomes for teenagers who received vision rehabilitation services. J Vis Impair Blind. 2001;95(4):229-234.
- ↑ 31.0 31.1 Reimer AM, Cox RFA, Nijhuis-Van der Sanden MWG, Boonstra FN. Improvement of fine motor skills in children with visual impairment: An explorative study. Res Dev Disabil. 2011;32(5):1924-1933.