All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Ocular echography or ocular ultrasonography (Ophthalmic ultrasound) is an important modality of ophthalmic investigation.
Mechanism of ocular ultrasound
The ultrasound uses piezoelectric lead-zirconate-titanate crystals which generate ultrasonic (inaudible, more than 20 kilohertz) sound waves from electricity. The ultrasonic wave gets reflected from any echodense object. The piezoelectric crystal picks up the reflected sound and converts it to electric signals, which give the image of the echogram.
If the velocity of sound in the media is known, the distance of the object from the probe can be measured. The echodensity of the object determines the amount of reflected sound wave received by the probe and hence the intensity of whiteness in B scan and the amplitude in the A scan.
Speed of sound in various media
The speed of sound varies according to the media through which it passes. The distance, or axial length, is calculated from the speed and time (required by the sound to reach the lesion and come back from the lesion to be detected by the piezoelectric material). When the speed is slowed (e.g., silicone oil), the machine erroneously shows a long axial length.
| Medium | Speed in meter per second |
|---|---|
| Aqueous and Vitreous | 1532 |
| Normal lens | 1641[1] |
| Intraocular and orbital soft tissue, blood | 1550[1] |
| Air | 343 |
Frequency of the probe
Ophthalmic ultrasound probe usually uses 7.5, 8, 10, or 12 megahertz (MHz) probes, which is in contrast to the 2.5 or 3.5 MHz probes used for abdominal ultrasound.[2] When the frequency of the probe increases, the resolution of the image increases but the depth of penetration of the ultrasound decreases. A probe using 20 MHz has been used for high resolution imaging of the retina, including detection of cystoid macular edema, central serous chorioretinopathy, and evaluation of choroidal echoarchitecture.[3] Ultrasound biomicroscopy (UBM) uses 35 MHz and 50 MHz probes. The 35 MHz probe has a higher penetration and can evaluate the ciliary body and ciliary processes in detail.
Types of ocular ultrasound
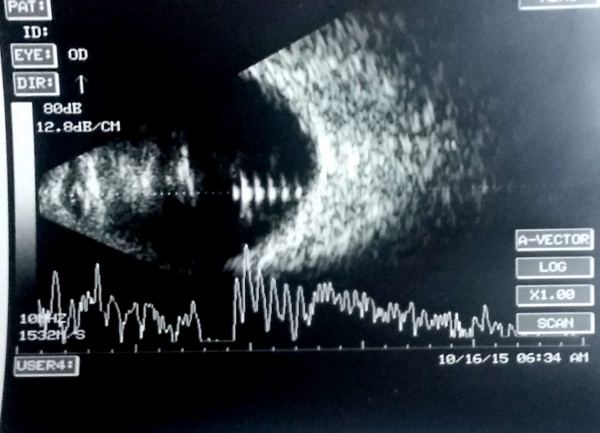
A scan
Amplitude scan shows the amplitude of the echoes as vertical height from a baseline as the strength of the echoes. The horizontal distance between two echoes can be used to measure the distance between two structures. Ocular axial length is often measured using an A scan probe during ocular biometry before cataract surgery.
B scan
The brightness scan gives a 2-dimensional display showing the size and echotexture of a lesion.
Conventions during ocular ultrasound
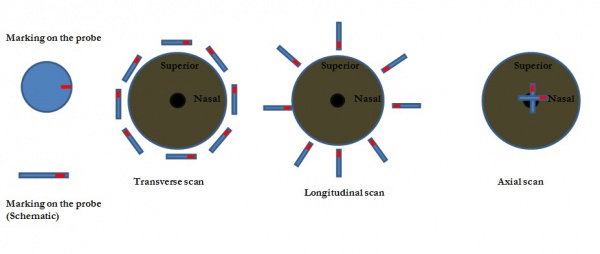
The B scan probe has a marking. Conventionally the marking denotes the upper part of B scan. The orientation of the B scan probe may be longitudinal, transverse, or axial. In longitudinal scans, the longest diameter of the oval probe face is perpendicular to the limbus and the marking always faces towards the limbus. In transverse scans, the axis of the probe is parallel to the limbus. For upper and lower horizontal positions of the probe near the limbus, the marking faces nasally. In vertical and oblique probe positions, the marking is kept superior.[1]
Indications of ocular ultrasound
- Ocular biometry for calculation of the power the intraocular lens
- Cases with media haze in which the posterior segment cannot be evaluated clinically
- Cornea: Corneal scar, hazy cornea, corneal edema, and others
- Anterior chamber: Hyphema, severe anterior segment inflammation with exudates
- Dense cataract
- Pupillary membrane, posterior synechiae
- Retrolental membrane, posterior capsular opacity
- Vitreous hemorrhage, Severe vitreous membranes/exudates
- To determine the nature of an ocular mass or optic disc lesion
- To differentiate retinal detachment (RD) of rhegmatogenous etiology from an exudative retinal detachment and also to differentiate RD from retinoschisis
- To detect and localize intraocular foreign bodies
- To evaluate orbital lesions
- To evaluate the retina, choroid, and sclera in various conditions, including inflammatory diseases
Screening technique using B scan
In case of media haze, the systematic B scan examination includes four transverse scans (scanning superior, nasal, inferior, and temporal retina) and two axial scans (Horizontal and vertical).[1]
Evaluation of an ocular ultrasonogram
The evaluation of ophthalmic ultrasonogram includes:
- Location of the echo
- Size/shape of echo
- Aplitude of echo (the brightness of echo in B scan)
- Movements of the lesion with ocular movements
- Echotexture of the lesion (homogenous/heterogenous)
- Attenuation of sound beam due to reflection/scattering or absorption of sound energy, which leads to a decrease in the amplitude within the lesion. Structures with very strong sound attenuation, such as calcification/bone/metallic foreign body, produce acoustic shadowing.
Ocular ultrasonogram (USG) in various ocular conditions
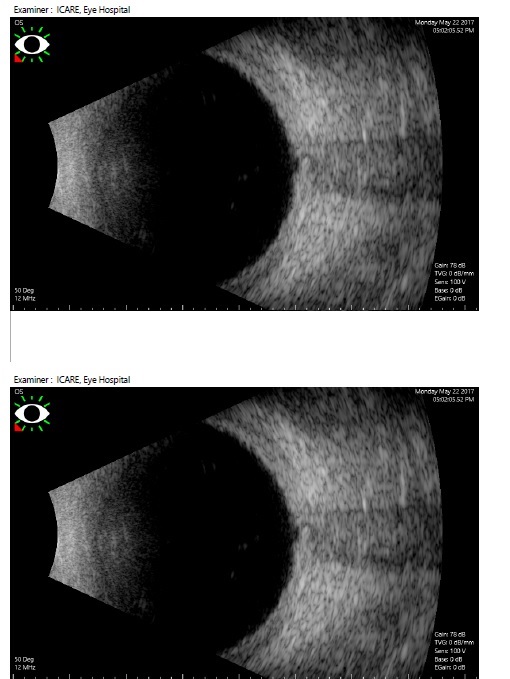
Ultrasonographic features of retinal detachment versus posterior vitreous detachment
One of the most important use of ocular ultrasound is to rule out a retinal detachment (RD) which may require vitreoretinal surgical intervention. Differentiation of a posterior vitreous detachment (PVD) from RD is important. An old RD may also have retinal macrocysts[4] at the macula or retinal periphery, which is detectable by the ultrasonography.
| Retinal detachment
(RD) |
Posterior vitreous detachment (PVD) | |
|---|---|---|
| Location | Attached to the optic disc at both sides | Is not attached to the optic disc in a complete PVD. In incomplete PVD, one or both sides may be attached to optic disc margin. |
| Shape | Thick folded membrane. May be smooth. | Usually fine, smooth/folded membrane. May be thick especially in cases with neovascularization of disc/fibrovascular proliferation |
| Amplitude of Echo | 100% compared to choroid-sclera. | Usually less than 100% |
| Persistence in low gain (around 40-50 decibel) | Persists | Disappears |
| After-movements | limited | good |
| Associated features | May have macrocysts (hemorrhagic or non-hemorrhagic), peripheral membrane also have 100% amplitude | Peripheral/anterior part of membrane usually has <100% spike, may be attached to the ocular coats (retina) at areas other than disc (at neovascularization of retina ) |
| Doppler | Vascular | Usually avascular. The fibrovascular proliferations with attached vitreous membranes may have active vascularity. |
The retinal shortening and retinal to choroidal length ratio may denote an increased risk for recurrent retinal redetachment after vitreoretinal surgery.[5] Ocular echography may detect the location of break and characteristic of break (e.g., giant retinal tear). The amplitude of subretinal echoes may give a clue to its nature (clear fluid is anechoic; hemorrhage and turbid proteinaceous fluid show point echoes of mild to moderate amplitude).
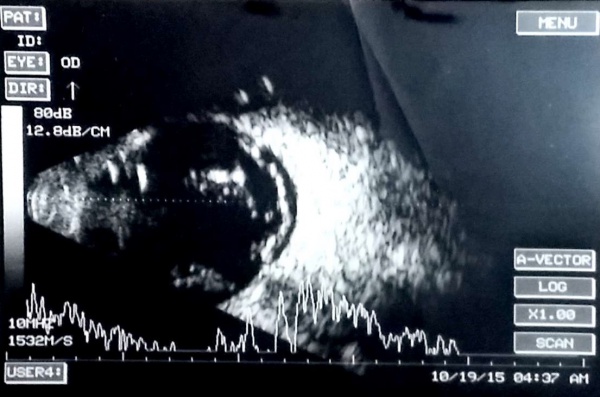
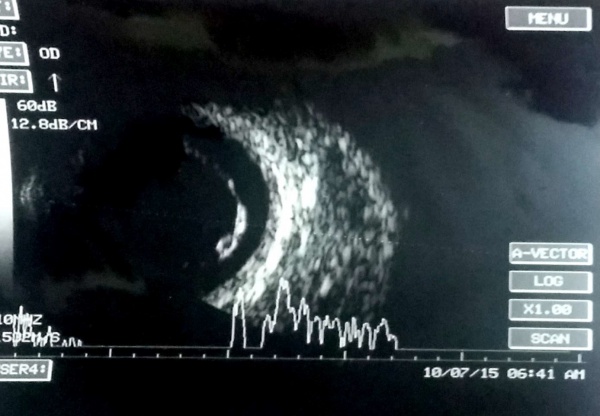
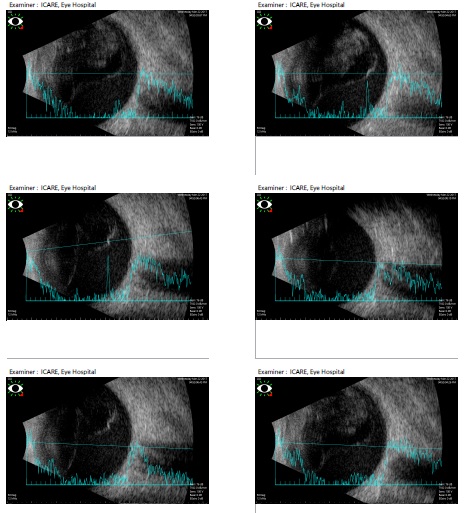
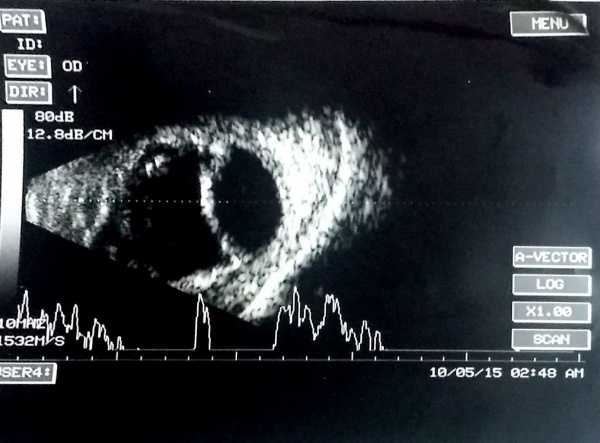
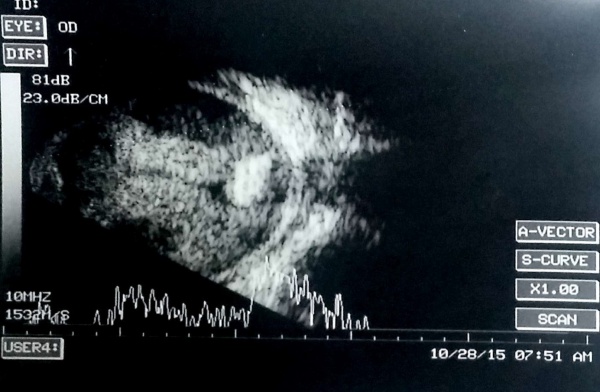
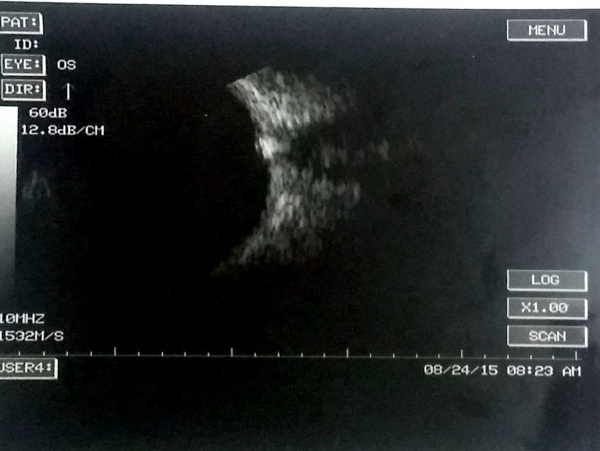
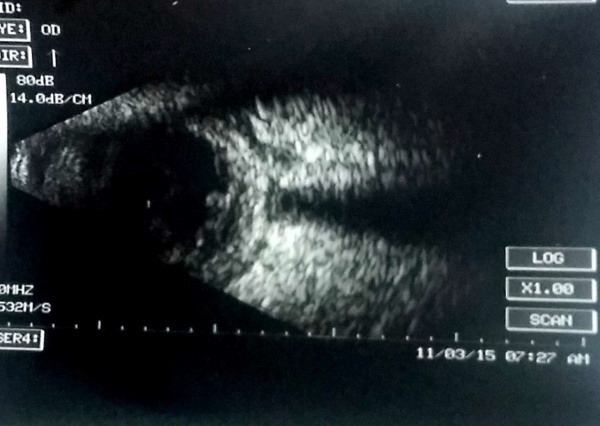
[The funnel RD is attached to the disc and is not showing after-movements with ocular movements.]
In cases of bullous retinal detachments with 'shifting fluid' (in sitting position the RD is inferior bullous and superior retina seems attached; in supine position, there is a total retinal detachment), it may be necessary to rule out an exudative retinal detachment (ERD). ERD usually shows subretinal echoe. A choroidal mass may be detectable, or the ultrasound may reveal another cause of the ERD (e.g., posterior scleritis, Vogt-Koyanagi-Harada syndrome).
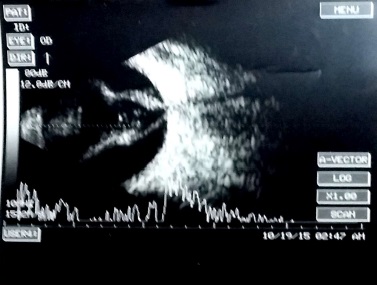
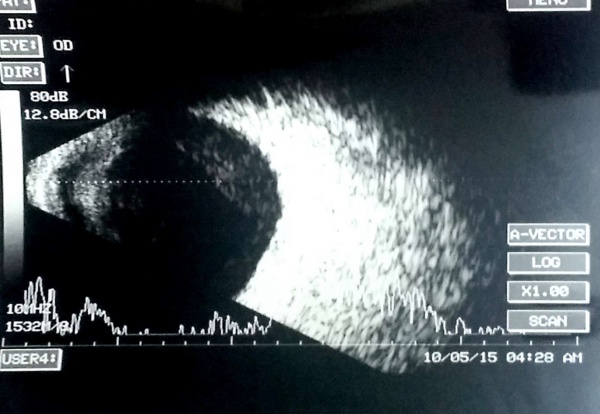
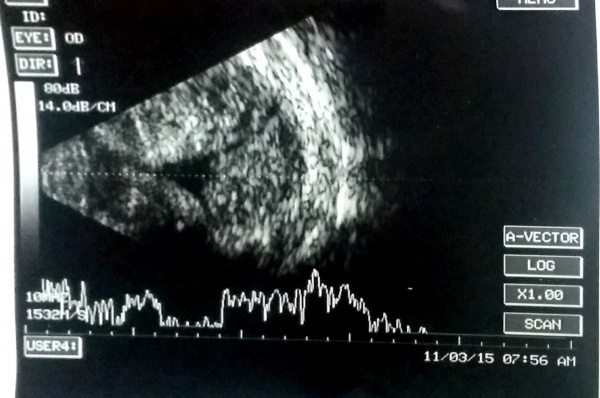
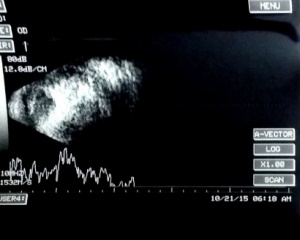
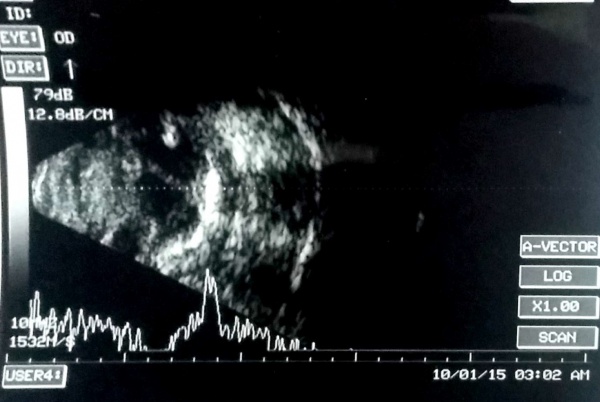
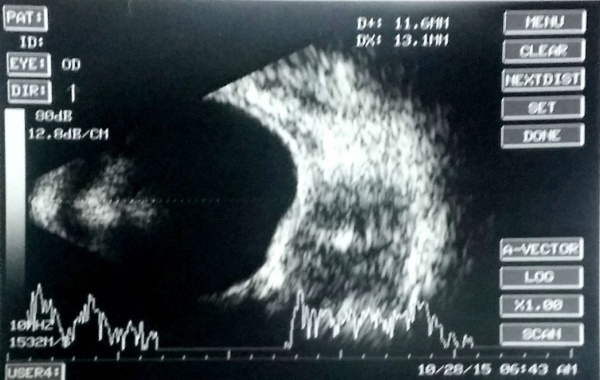
A case of choroidal hemangioma[6] with exudative RD. Note the limited after-movements.
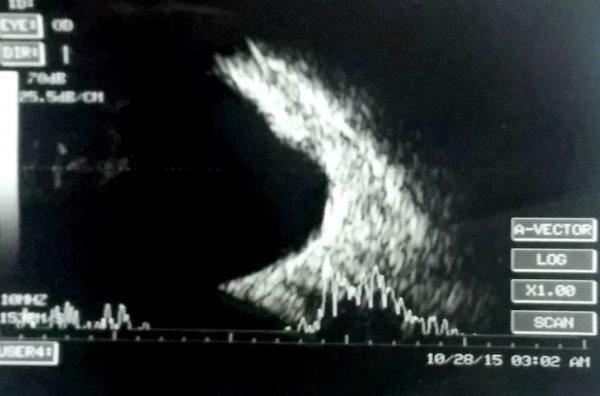
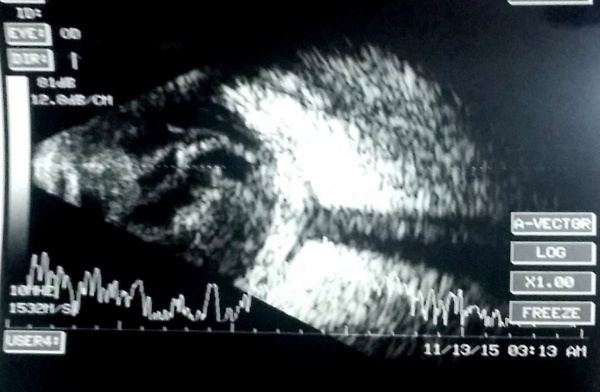
An ocular USG also detects tractional retinal detachments, which have concave or table-top appearance and limited after-movements. Most commonly, there is evidence of neovascularizations or fibrovascular proliferations.
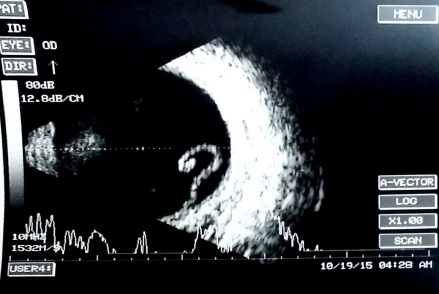
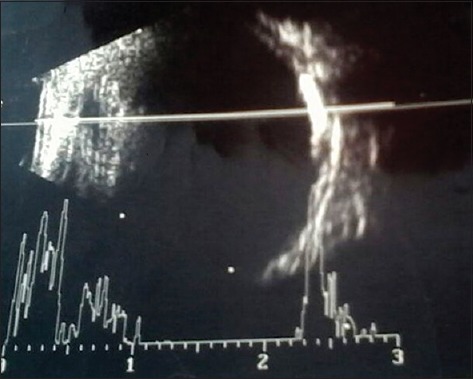
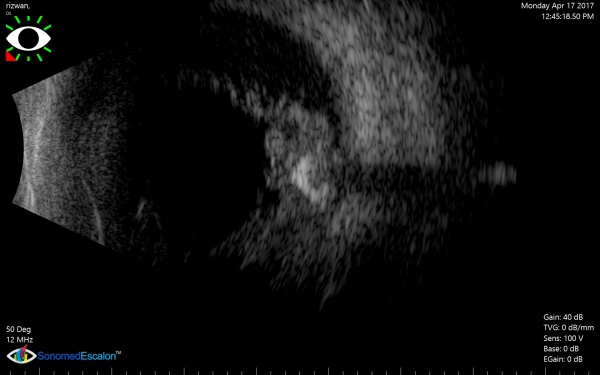
A PVD is usually a thin wavy membrane which moves freely with ocular movements.
Cupping of the optic nerve head
The optic nerve head may show depression or bean pot like configuration in ultrasound, especially in blind eyes with end-stage glaucoma. Ocular echography constitutes an important modality for detecting the cause of vision loss in severe visual impairment with opacity in the ocular media.
Excavation/ectasia/protrusion of ocular coats
The USG also detects elongated globe in pathological myopia with posterior staphyloma. The coloboma of optic nerve head or fundus can be documented.
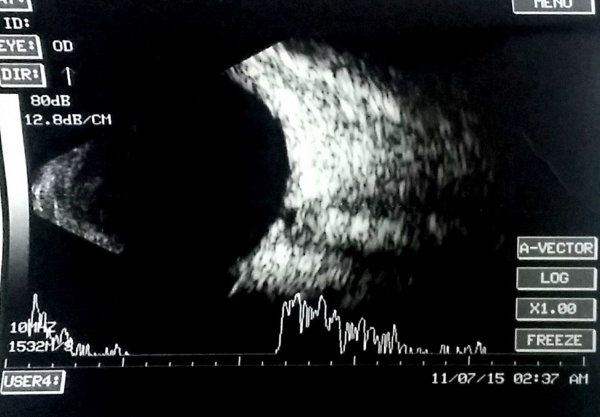
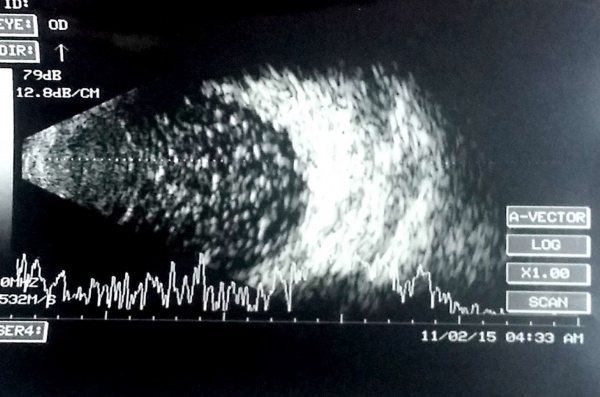
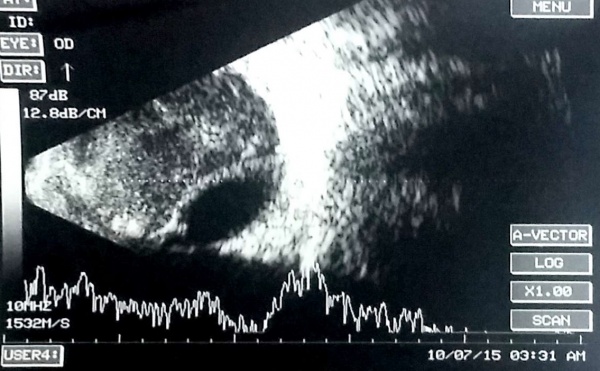
Ultrasonographic features of Vitreous hemorrhage
Vitreous hemorrhage reveals multiple mobile point echoes in the vitreous cavity. The amplitude of such point echoes is usually mild to moderate. In cases of vitreous hemorrhage due to proliferative retinopathies (e.g., proliferative diabetic retinopathy, retinal vasculitis), it is also necessary to localize the area of neovascularization/fibrovascular proliferation. The areas of neovascularization (NV) are denoted by areas of strong vitreoretinal adhesion, the PVD is attached to the NV in a 'v' shaped configuration. In vitreous hemorrhage related to a PVD-induced retinal tear, a PVD is obvious in the USG. Also, the anterior extent of the PVD may be seen attached to the anterior flap of retinal tear. In old patients with evidence of age-related macular degeneration in the fellow eye, it is necessary to rule out a large choroidal neovascular membrane with subretinal bleed and breakthrough bleeding into the vitreous.
Note the after-movements of the PVD in this patient with subhyaloid hemorrhage and vitreous hemorrhage.
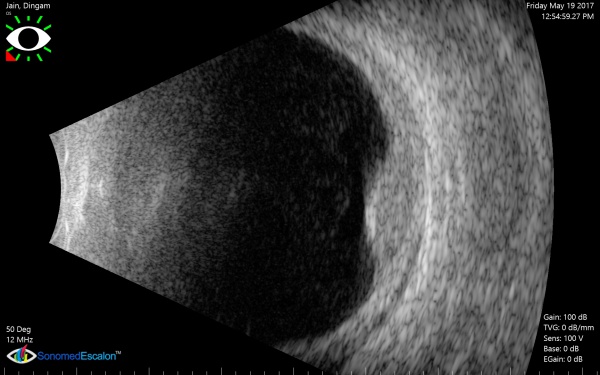
It is important to keep the gain in optimal setting (around 70decibels- varies with different machines), as high gains (e.g., 100 decibels) show many echoes in normal transparent vitreous and may give a false impression of vitreous hemorrhage.
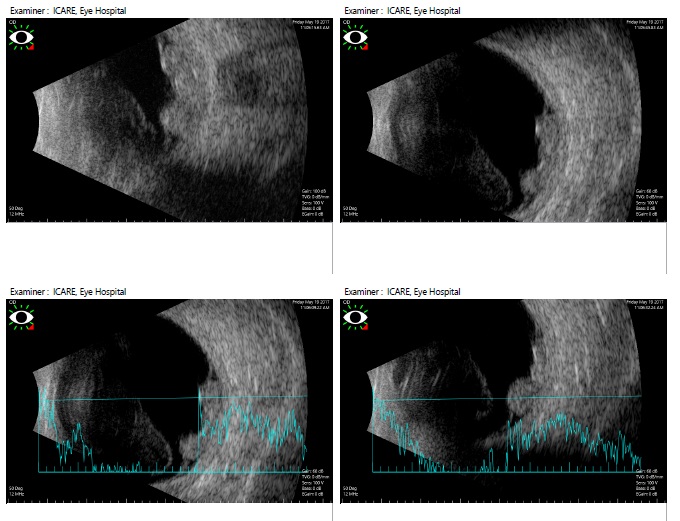
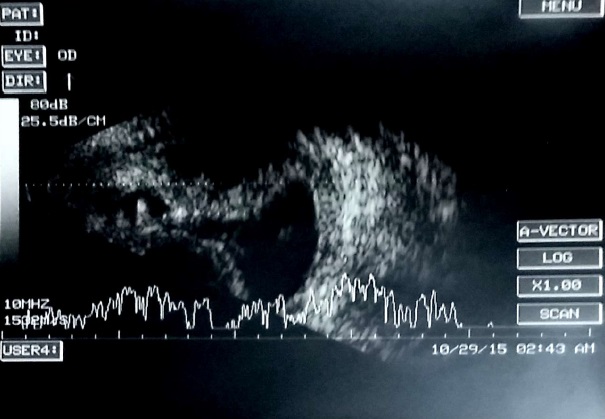
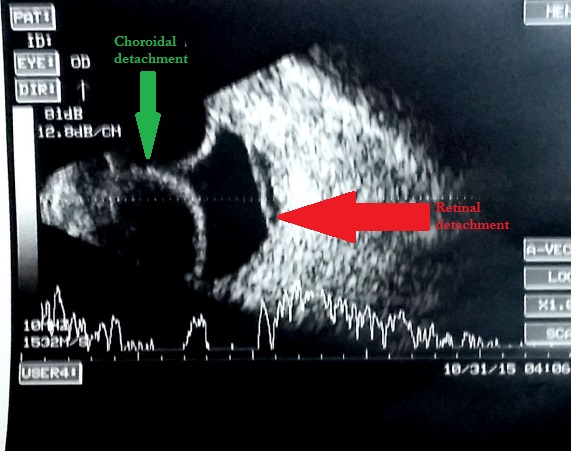
Ultrasonographic features of choroidal detachment (CD)
A CD is denoted by a round mound which is limited by the strong uveoscleral attachments (scleral spur, vortex veins, and optic nerve). It has limited mobility and an A scan passing perpendicularly through a CD shows 'M' (double peak) shape. The shape is typically of a smooth dome, usually not attached to the optic disc. The fluid in the suprachoroidal space may be anechoic (serous CD) or have mild to moderate amplitude point echoes (hemorrhagic CD). When CDs touch each other they are called kissing choroidals, and such cases may be more prone to permanent adhesion and may guide the timing of surgery in suprachoroidal hemorrhage. USG also notes the clot lysis in suprachoroidal hemorrhages and guides timing of surgery, and the location of the suprachoroidal hemorrhage guides the area of drainage.
Vitreous opacities/echoes
Asteroid hyalosis is denoted by moderate to high amplitude point spikes which are separated from the PVD by a clear space . In silicone oil, the speed of sound is low (980 meter/second for 1000 centiStokes and 1040 meter/second for 5000 centiStokes ) and hence the measured axial length by echography is unusually long.[7] Sound attenuation under silicone oil is high, making it unreliable for detection of retinal detachment under silicone oil. After removal of silicone oil, some emulsified droplet of silicone oil may remain in the vitreous cavity giving rise to mobile moderate to high amplitude point spikes in the vitreous cavity.
Retinoschisis
Retinoschisis is a thin immobile membrane with convex and smooth configuration usually on temporal retina of a hyperopic patient. The height of this round mound typically does not decrease on indentation or pressure (versus retinal detachment where the height reduces on indentation).
Intraocular masses
Ultrasonographic appearance of Choroidal melanoma
A choroidal melanoma shows a solid mass with homogenous appearance (moderate to low reflectivity) arising from the choroid with collar-button or mushroom appearance, acoustic hollow, and choroidal excavation. The A scan shows a typical reduction of amplitude with angle kappa which denotes the sound attenuation within the mass. The mass may be associated with retinal detachment, extrascleral extension, and uncommonly subretinal or suprachoroidal hemorrhage.
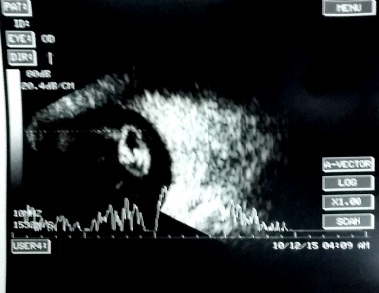
Ultrasonographic appearance of Retinoblastoma
Ocular echogram showing moderate to high amplitude echoes usually with acoustic shadow (calcification) in a child with leukocoria denotes a retinoblastoma unless proven otherwise.
Ultrasonographic features of Choroidal Osteoma
Choroidal osteoma shows a choroidal mass high amplitude and acoustic shadow.[8]
Ultrasonography of Choroidal hemangioma
It is solid dome shaped mass of choroid with high amplitude (and thickening of the choroid) but no angle kappa (sound attenuation) unlike choroidal melanoma. The lesions are usually mildly elevated (height is less than width), unlike the melanoma which may have height more than width.
Intraocular calcification
The causes of intraocular calcification extremely high amplitude lesion with acoustic shadow include
- Intraocular calcification due to optic nerve head drusen,[9] retinoblastoma, retinocytoma, astrocytic hamartoma, choroidal osteoma, and phthisis bulbi.[10]
Inflammation and infection
Endophthalmitis
Endophthalmitis is a purulent inflammation of intraocular fluids and adjacent structures usually due to infection.[11] The USG shows mild to moderate amplitude point spikes in the vitreous that are very similar to vitreous hemorrhage. Clinical evidence of inflammation, hypopyon and vitritis with recent penetrating trauma or ocular surgery points towards endophthalmitis in such cases. It may be associated with retinal detachment, intraocular foreign body, choroidal detachment and others. The USG may also be used to look for the response to therapy and reduction in vitreous echoes.
Panophthalmitis
It is denoted by thickening of the ocular coats, subtenon fluid, and clinical evidence of pain and limitation during ocular movements, usually in cases with orbital cellulitis and/or penetrating ocular trauma with endophthalmitis.
Posterior Scleritis
The thickness of ocular coats is increased with fluid in subtenon space and around optic nerve (T sign). Inflammation of adjacent structures (e.g., dacryoadenitis) may also cause a secondary posterior scleritis with subtenon fluid.[12]
The thickness of ocular coats is also increased in sympathetic ophthalmia,[13] Vogt-Koyanagi-Harada syndrome, phthisis bulbi, small globe (nanophthalmos)[14], panophthalmitis, and other conditions.
Cysticercus
Cysticercus is denoted by a round cystic lesion with a hyperechoic dot like lesion (scolex). Rarely, retinal detachment may be associated with cysticercus, which is demonstrated in USG. USG also picks up the real time movement of live cysticercus. Myocysticercus may also be detected and monitored for response to therapy.
Trauma
In acute trauma with open globe injury, the ocular ultrasound may be avoided the as undue pressure on globe may lead to expulsion of intraocular contents. Trauma can lead to vitreous hemorrhage, retinal detachment, suprachoroidal hemorrhage, and others.
Foreign body
USG forms an indispensable part in the management of intraocular foreign body (IOFB). It detects and localizes the foreign body and the size of the foreign body can be measured. Metallic IOFBs shows extremely high amplitude with acoustic shadow.
Extreme anterior and inferior parts of the vitreous cavity need to be examined with USG along with detailed protocol for screening using B scan in cases of suspected IOFB. CT orbit with thin slices rules out multiple IOFBs/orbital foreign bodies and clearly delineates location/detection of IOFB, especially if the foreign body is spanning across the vitreous cavity, ocular coats, and retro-ocular space.
Post-surgery evaluation
USG is helpful for evaluation of the posterior segment after ocular surgeries when media become hazy due to corneal edema, hyphema and other reasons. Other conditions in which USG plays a critical role includes endophthalmitis, retinal detachment, choroidal detachment, and rupture of the posterior ocular coats.
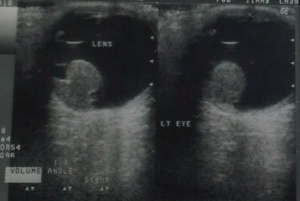
Retained lens material (posterior dislocation of lens fragments)
After posterior capsular rupture with dropped lens material in the vitreous cavity, the USG locates the lens material and gives an idea of the size of the lens fragments. The lens matter appears as a lesion in the vitreous cavity (usually inferiorly) with moderate to high amplitude which moves on ocular movement.
Dropped intraocular lens (IOL)
IOL is identified by high amplitude spike associated with acoustic reverberations.
Orbital ultrasound
Most of the ocular ultrasound machines provide an orbital mode in which deep structures within the orbit can be evaluated like in patients with proptosis. Orbital abscess shows a cavitary lesion with mild to moderate amplitude point echoes. USG may be used to measure the muscle thickness. Due to pressure from the orbital lesion the globe may be compressed. Longitudinal or transverse B scans can be used, as well as A scans to assess the extraocular muscles and the different pathologies associated with them. Muscle thickening is the most frequently found abnormality. Ultrasound, compared to MRI or tomography, is more effective in detecting these subtle changes. Some of the most frequent disorders that can be evaluated with ultrasound are: Thyroid eye disease, myositis, tumors, trauma and muscle thickening/thinning. Ultrasonography in patients with myositis is useful for diagnosis as well as for follow-up.[15][16]
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 Green RL, Byrne SF. Chapter 14: Diagnostic Ophthalmic Ultrasound. In: Ryan SJ, ed. Retina. Philadelphia: Elsevier/Mosby 2006. 265–350.
- ↑ Morgan MA, Nadrljanski MM. Ultrasound frequencies | Radiology Reference Article | Radiopaedia.org. Radiopaedia. https://radiopaedia.org/articles/ultrasound-frequencies (accessed 23 May 2017).
- ↑ Doro D, Visentin S, Maimone PE, et al. High-resolution ultrasonography in central serous chorioretinopathy. Am J Ophthalmol 2005;139:550–2. doi:10.1016/j.ajo.2004.08.059
- ↑ Tripathy K, Bypareddy R, Chawla R, et al. Optical Coherence Tomography Follow-up of an Unusual Case of Old Rhegmatogenous Retinal Detachment With a Hemorrhagic Macrocyst at the Macula. Ophthalmic Surg Lasers Imaging Retina 2015;46:1058–60. doi:10.3928/23258160-20151027-14
- ↑ Takkar B, Tripathy K, Azad SV, et al. Objective Quantification of Retinal Shortening: Sonographic Evidence of Intraretinal Proliferative Vitreoretinopathy. Ophthalmic Surg Lasers Imaging Retina 2016;47:746–50. doi:10.3928/23258160-20160808-08
- ↑ Tripathy K, Das A, Subhadarshani S. Sturge–Weber syndrome with choroidal hemangioma. Indian Dermatol Online J 2017;8:225. doi:10.4103/idoj.IDOJ_148_16
- ↑ Silicone Oil ~ Retinal Detachments IOL Power Calculations | East Valley Ophthalmology. http://www.doctor-hill.com/iol-main/silicone.htm (accessed 27 May 2017).
- ↑ Wadekar B, Tripathy K, Chawla R, et al. An 18-year-old female with unilateral painless vision loss. Oman J Ophthalmol 2016;9:193. doi:10.4103/0974-620X.192311
- ↑ Tripathy K, Chawla R, Meena S, et al. Unilateral giant peripapillary drusen and retinal drusenoid deposits in a case of X-linked retinoschisis. BMJ Case Rep 2016;2016. doi:10.1136/bcr-2016-214558
- ↑ Gaillard F. Calcification of the globe (differential) | Radiology Reference Article | Radiopaedia.org. Radiopaedia. https://radiopaedia.org/articles/calcification-of-the-globe-differential (accessed 27 May 2017).
- ↑ Tripathy K, Venkatesh P. Surgical management of endophthalmitis. 2016. doi:10.6084/m9.figshare.2059992.v1
- ↑ Kumawat B, Tripathy K, Venkatesh P, et al. Lacrimal abscess mimicking a choroidal mass: an ultrawide field evaluation. Can J Ophthalmol J Can Ophtalmol 2016;51:e92-94. doi:10.1016/j.jcjo.2016.01.010
- ↑ Tripathy K, Mittal K, Chawla R. Sympathetic ophthalmia following a conjunctival flap procedure for corneal perforation. BMJ Case Rep 2016;2016. doi:10.1136/bcr-2016-214344
- ↑ Venkatesh P, Chawla R, Tripathy K, et al. Scleral resection in chronic central serous chorioretinopathy complicated by exudative retinal detachment. Eye Vis Lond Engl 2016;3:23. doi:10.1186/s40662-016-0055-5
- ↑ Frazier S, Green RL. Ultrasound of the Eye and Orbit, 2nd Edition, Mosby 2002.
- ↑ Bechara I, Mercado C, Muñoz-Ortiz J, Montoya A. Characterization of patients with ocular pain evaluated with ultrasound. Eur J Ophthalmol. 2022 Dec Epub ahead of print. PMID: 36539998.