Asteroid Hyalosis (AH)
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.

Disease Entity
Asteroid hyalosis (AH) is a common (1 in 200 person) clinical entity in which calcium-lipid complexes are suspended throughout the collagen fibrils of the vitreous. [1]
Disease
Benson, in 1894, was the first to describe accurately and to differentiate AH from synchysis scintillans. Because the vitreous particles resembled “stars on a clear night” he termed the condition asteroid hyalitis, but Luxenberg and Sime later suggested the term “asteroid hyalosis” in view of the absence of inflammatory changes.[2] Clinically, the AH granules move with the movement of eye and do not gravitate downwards like synchysis scintillans.
Etiology
Histologically, asteroid bodies are rounded structures that stain positively with alcian blue and positively with stains for neutral fats, phospholipids, and calcium. The bodies stain metachromatically and exhibit birefringence. Occasionally, asteroid bodies will be surrounded by a foreign body giant cell, but the condition is not generally associated with vitreous inflammation.
Risk Factors
AH is a relatively uncommon, usually seen unilaterally in patients over 55 years of age. It has no race predisposition, but occurring with much greater frequency in men (1.4 %) than in women (0.6%).[4]
The reported incidence in the general population is 1% according to the Australian Blue Mountains Eye Study[4] and 1.2% prevalence which reported in the U.S. Beaver Dam Eye Study.[5]
The estimate prevalence of AH in Seoul, Korea is 0.36%.[6]
The Blue Mountains Eye Study also found no evidence to support earlier observation of a significant association between asteroid hyalosis and diabetes, heart disease, higher body mass index, a history of gout and of higher levels of alcohol consumption, as reported by previous studies.[6]
Increased odds were found for associations with asteroid hyalosis, but none of these associations were statistically significant.[4]
According to an unique epidemiological autopsy cohort study from the University of California at Los Angeles (UCLA) autopsy eye database from 1965 to 2000 where 10 801 patients were examined for AH and its systemic associations yielded a higher prevalence (1.96%) of AH than previous studies.
Asteroid hyalosis was strongly correlated with age and inversely correlated with posterior vitreous detachment.[7]
No statistically significant association between AH and ARMD or DM was found. Most patients (86%) had unilateral vitreous deposits and IOP values were lower in the affected eye. PPV combined with phacoemulsification proved to be a safe and effective therapy in selected patients.[8]
General Pathology
The exact mechanism of formation of asteroid bodies is not known; however, element mapping by electron spectroscopic imaging has revealed a homogeneous distribution of calcium, phosphorus, and oxygen. The electron energy loss spectra of these elements show details similar to those found for hydroxyapatite. Immunofluorescence microscopy has revealed the presence of chondroitin-6-sulfate at the periphery of asteroid bodies; and carbohydrates specific for hyaluronic acid were observed by lectin-gold labeling to be part of the inner matrix of asteroid bodies. Thus, asteroid bodies exhibit structural and elemental similarity to hydroxyapatite, and proteoglycans and their glycosaminoglycan side chains appear to play a role in regulating the biomineralization process.[9]
Pathophysiology
Although AH has been associated with several systemic diseases, the causes and mechanisms of AH formation remain unknown. Three major studies mentioned above conclude that AH is primarily associated with aging.
In the Beaver Dam Study of Wisconsin where 4952 patients were examined with prevalence increasing from 0.2% in subjects 43–54 years of age to 2.9% in those aged 75–86 years.[5]
The Australian Blue Mountains Eye Study of 3654 patients aged 49–97 years confirmed a similar 1% prevalence of AH. In this group, the prevalence of AH also increased with age from 0% of persons 49–55 years of age to 2.1% of persons aged 75–97 years, and AH was again more prevalent in men.[4] A higher, 1.96%, prevalence of AH was observed in the third study from the University of California at Los Angeles (UCLA) autopsy eye database from 1965 to 2000 where 10 801 patients were examined.[7] This retrospective study, which demographically matched the characteristics of the US population on the 2000 census, also showed an inverse relationship between AH and posterior vitreous detachment. Although these three major studies found AH to primarily correlate with ageing, others suggest that AH is associated with diabetes mellitus (DM), hypertension, hypercholesterolemia or lipidemia, or increased serum calcium levels. Of these, a link to DM is most often cited; however, this link is also the most controversial. Although AH predominantly occurs unilaterally, AH should be bilateral if linked to systemic diseases such as DM because each eye is equally exposed to hyperglycemia. Bilateral ‘trends’ of AH have been suggested among diabetic populations UCLA autopsy study[7], which observed a statistical association between diabetes and bilateral AH before adjusting the data for age and sex. However, in the UCLA study, AH was present only in 20 of 780 diabetics. AH formation in diabetics has been suggested to be secondary to retinal vascular changes. The overall relationship between DM and AH is further complicated by data suggesting that AH may arrest the process of vitreous collapse or contraction in eyes with proliferative diabetic retinopathy.[10]
Diagnosis
Diagnostic procedures
Traditional methods of funduscopic visualization can be limited in the AH eyes, and alternative imaging modalities such as Flourescein Angiography(FA) and ultrasonography may not provide adequate diagnostic capabilities to yield accurate diagnoses.[11] In the National Screening Program in England, Asteroid hyalosis was the cause of ungradable photographs in approximately 0.4% of the screened population of people with diabetes and was the cause of 8.5% of all ungradable retinal screening photographs during the time of the study. Suggested that another method of screening, such as slit lamp biomicroscopy and possibly optical coherence tomography, is required for such patients.[12]
Complete PVD appears to be unlikely to occur in eyes with AH. In addition, spontaneous PVD in eyes with AH might lead to vitreoschisis or residual whole layer or posterior vitreous cortex, possibly due to anomalous vitreoretinal adhesion.[13]
OCT identified the specific retinal anatomical abnormality, allowing for definitive diagnosis. FA and/or funduscopic evaluation assisted the diagnosis, but appropriate disease management should be ultimately guided by OCT.[11] OCT uses an 830-nm wavelength light beam that is less susceptible to distortion from asteroid bodies and other media opacities. With dense asteroids, however, the light beam can be absorbed or reflected. This degradation may occur with both incident and reflected light beams, leading to areas of lower signal strength and shadowing of certain areas on the retina. OCT technicians can minimize these image artifacts by properly positioning the patient for the clearest OCT scan, adjusting the focus knob to the most highly saturated diopter, using the polarization function, and ensuring proper corneal lubrication. OCT in the setting of media opacity of the vitreous cavity is not always fruitful. In eyes with varying degrees of vitreous hemorrhage, the 830-nm wavelength light beam of OCT is absorbed by blood, making imaging often imprecise or impossible. Absorption of the incident light by asteroid bodies is less consequential.[11]
Spontaneous PVD in AH might lead to anomalous PVD occasionally associated with vitreoschisis, possibly due to anomalous vitreoretinal adhesion. However, the diverse vitreoretinal diseases present in this study can, irrespective of the presence of AH, on their own be complicated by abnormal vitreoretinal adhesions and anomalous PVD. Furthermore, OCT was a useful instrument for investigating the vitreoretinal interface in eyes with AH, and intraoperative triamcinolone acetonide facilitated complete removal of residual vitreous cortex, possibly lowering the incidence of post-operative vitreoretinal interface disorders, although longer follow-up is necessary.[13]
In the cases when on the clinical examination revealed dense asteroid hyalosis obscuring the fundus with a limited view Optos ultra-wide field imaging also can be helpful in the diagnosis and management of retinal/ choroidal lesions.[14]
Differential Diagnosis
When evaluating vitreous opacities, it's essential to distinguish Asteroid Hyalosis (AH) from other conditions that present with similar findings. The primary differential diagnoses include:
- Synchysis Scintillans: Characterized by freely mobile, golden-brown cholesterol crystals within a liquefied vitreous, often associated with prior ocular trauma or disease.
- Vitreous Hemorrhage: Presents as diffuse or localized blood within the vitreous cavity, typically linked to retinal tears, proliferative diabetic retinopathy, or trauma.
- Vitritis (Inflammatory Vitreous Opacities): Inflammatory cells in the vitreous due to infections or autoimmune conditions, often accompanied by pain, redness, and decreased vision.
- Amyloidosis: Deposition of amyloid proteins in the vitreous, leading to opacities; often part of a systemic condition.
- Malignancies (e.g., Intraocular Lymphoma): Can present with vitreous opacities and are often associated with other systemic signs.
A comprehensive clinical evaluation, including patient history, ocular examination, and imaging studies, is crucial for accurate differentiation among these conditions.
For a detailed comparison between Asteroid Hyalosis and Synchysis Scintillans, please refer to the table in the previous section.
| Characteristic | Asteroid Hyalosis (AH) | Synchysis Scintillans (SS) |
|---|---|---|
| Age of Onset | Typically occurs in individuals over 55 years old. | More common in younger individuals, often around the 3rd decade of life. |
| Incidence | Relatively uncommon; prevalence ranges from 0.5% to 1.2% in various studies. | Extremely rare condition. |
| Laterality (Unilateral/Bilateral) | Usually unilateral. | Often bilateral. |
| Appearance | Numerous small, yellow-white, spherical opacities suspended throughout the vitreous, resembling "stars in the night sky." | Small, highly refractive, multicolored, flat, angular, or disc-shaped opacities giving a "snow globe" effect. |
| Composition | Calcium-lipid complexes (calcium soaps). | Cholesterol crystals. |
| Mobility | Move with the vitreous and return to their original position after eye movements; do not settle inferiorly. | Freely mobile within a liquefied vitreous; settle inferiorly due to gravity when the eye is stationary. |
| Vitreous State | Vitreous remains intact. | Vitreous is liquefied (syneresis). |
| Associated Conditions | Often associated with aging; previously thought to be linked with systemic conditions like diabetes and hypertension, but recent studies have not confirmed significant correlations. | Typically occurs in severely diseased eyes; associated with conditions such as vitreous hemorrhage, chronic uveitis, retinal detachment, ocular trauma, and advanced diabetic retinopathy. |
| Visual Acuity Impact | Usually asymptomatic with minimal impact on vision; may cause difficulties in fundus examination due to obscured view. | Can cause visual disturbances, including floaters or reduced visual acuity, especially if opacities are numerous or mobile. |
| Ultrasound Findings |
|
|
| Management | Typically no treatment required unless it significantly interferes with vision or fundus examination; vitrectomy may be considered in such cases. | Treatment focuses on addressing underlying conditions; vitrectomy may be considered if visual impairment is significant. |
Management
Complications
Asteroid Hyalosis rarely causes visual disturbances, and surgical removal is only rarely required. There have been a few reports of AH in patients with RP.[15] In some cases, a standard three-port vitrectomy was needed to remove the vitreous opacities because of progression of the vitreous opacities and decreased vision.
A study at the Kyushu University Hospital (Fukuoka, Japan), based on cohort of 320 patients with RP found 10 patients developed AH. Among these patents, 2 patients were younger than 50 years; bilateral AH was present in 4 of 10 cases; and rapidly progressive AH was found in 2 cases with associated loss of vision. The exact mechanism of progressive vision loss was unclear, however, one possible explanation may be that the vitreous condition in eyes with RP is different from that in normal eyes because of the blood–retinal barrier breakdown seen in patients with RP.[15]
Dramatic loss of visual acuity is unusual. Although there have been reports of surface calcifications of intraocular lenses in patients with asteroid hyalosis.[16]
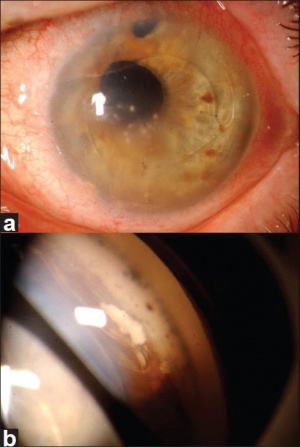
Also there are some reports of asteroid hyalosis prolapse into the anterior chamber, simulating metastasis.[3]
Additional Resources
References
- ↑ Ophthalmology, A.A.o., Section 12: Retina and Vitreous. Basic and Clinical Science Course. 2014-2015: American Academy of Ophthalmology. p. 311-312.
- ↑ Yazar, Z., et al., Asteroid hyalosis. Eur J Ophthalmol, 2001. 11(1): p. 57-61.
- ↑ Jump up to: 3.0 3.1 Shields, C.L., et al., Vitreous asteroid hyalosis prolapse into the anterior chamber simulating iris metastasis. Middle East Afr J Ophthalmol, 2012. 19(3): p. 346-8.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Mitchell, P., M.Y. Wang, and J.J. Wang, Asteroid hyalosis in an older population: the Blue Mountains Eye Study. Ophthalmic epidemiology, 2003.
- ↑ Jump up to: 5.0 5.1 Moss, S.E., R. Klein, and B.E.K. Klein, Asteroid hyalosis in a population: The Beaver Dam Eye Study. American Journal of Ophthalmology, 2001. 132(1): p. 70-75.
- ↑ Jump up to: 6.0 6.1 Kim, J.H., et al., Prevalence of and risk factors for asteroid hyalosis in Seoul, Korea. Retina (Philadelphia, Pa.), 2008. 28(10): p. 1515-1521.
- ↑ Jump up to: 7.0 7.1 7.2 Fawzi, A.A., et al., Asteroid hyalosis in an autopsy population: The University of California at Los Angeles (UCLA) experience. Arch Ophthalmol, 2005. 123(4): p. 486-90.
- ↑ Galveia, J., et al., Asteroid hyalosis: clinical review of 58 cases. Revista Brasileira de Oftalmologia, 2013. 72(5): p. 312-315.
- ↑ Ophthalmology, A.A.o., Section 04: Ophthalmic Pathology and Intraocular Tumors. Basic and Clinical Science Course. 2014-2015: American Academy of Ophthalmology. p.138-139.
- ↑ Kador, P.F. and M. Wyman, Asteroid hyalosis: pathogenesis and prospects for prevention. Eye (London, England), 2008. 22(10): p. 1278-1285.
- ↑ Jump up to: 11.0 11.1 11.2 Hwang, J.C., et al., Optical coherence tomography in asteroid hyalosis. Retina (Philadelphia, Pa.), 2006. 26(6): p. 661-665.
- ↑ Wright, A.D., Y.C. Yang, and P.M. Dodson, Asteroid hyalosis and photographic diabetic retinopathy screening. Diabetic Medicine, 2010.
- ↑ Jump up to: 13.0 13.1 Mochizuki, Y., et al., Anatomical findings of vitreoretinal interface in eyes with asteroid hyalosis. Graefes Arch Clin Exp Ophthalmol, 2009. 247(9): p. 1173-7.
- ↑ Motiani, M.V., et al., Diagnosis of Choroidal Melanoma in Dense Asteroid Hyalosis. Seminars in ophthalmology, 2016: p. 1-3.
- ↑ Jump up to: 15.0 15.1 Ikeda, Y., et al., Retinitis pigmentosa associated with asteroid hyalosis. Retina (Philadelphia, Pa.), 2010. 30(8): p. 1278-1281.
- ↑ Heagley, D., et al., Asteroid hyalosis of the vitreous humor: an uncommon finding. Diagn Cytopathol, 2013. 41(10): p. 926-7.

