All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Summary
Tolosa-Hunt syndrome describes episodic orbital pain associated with paralysis of one or more of the third, fourth and/or sixth cranial nerves, which usually resolves spontaneously but can relapse and remit.
History
It was first described in 1954 by Tolosa, who found granulomatous inflammation in the cavernous sinus during autopsy of a patient with severe left-sided trigeminal pain and total ophthalmoplegia[1]. In 1961, Hunt reported 6 cases of unilateral painful ophthalmoplegia that tested negative with angiography and lumbar puncture and rapidly resolved with steroids.[1]
Disease Entity
Tolosa-Hunt syndrome was first classified by the International Headache Society in 2004 and now is a part of Classification ICHD-3. ICD-10 for Tolosa Hunt Syndrome is H49.40.
Disease
Unilateral orbital or periorbital pain with paresis of third, fourth and/or sixth cranial nerves secondary to idiopathic inflammation of the cavernous sinus, superior orbital fissure or orbit.
The ICHD-3 Diagnostic criteria for Tolosa-Hunt syndrome are as follows[2]:
A. Unilateral orbital or periorbital headache fulfilling criterion C
B. Both of the following:
a. Granulomatous inflammation of the cavernous sinus, superior orbital fissure or orbit, demonstrated by MRI or biopsy
b. Paresis of one or more of the ipsilateral third, fourth, and/or sixth cranial nerves.
C. Evidence of causation demonstrated by both of the following:
a. Headache is ipsilateral to the granulomatous inflammation
b. Headache has preceded paresis of the third, fourth, and/or sixth nerves by ≤2 weeks, or developed with it.
D. Not better accounted for by another ICHD-3 diagnosis (see differential diagnosis section for more detail)
Of note:
Some reported cases of Tolosa-Hunt syndrome had additional involvement of the trigeminal nerve (commonly the first division) or optic, facial or acoustic nerves. Sympathetic innervation of the pupil is occasionally affected.
The syndrome has been caused by granulomatous material in the cavernous sinus, superior orbital fissure or orbit in some biopsied cases.
Careful follow-up is required to exclude other possible causes of painful ophthalmoplegia.
Etiology
Tolosa-Hunt syndrome is idiopathic.
Risk Factors
A possible risk factor for Tolosa-Hunt syndrome is a recent viral infection.
Pathophysiology
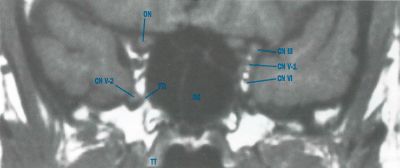
Tolosa-Hunt syndrome is idiopathic, sterile inflammation of the cavernous sinus. Its pathology is described as fibroblastic, lymphocytic, and plasmocytic infiltration of the cavernous sinus. Granulocytic and giant-cell infiltrations have also been described. Pathology may extend to involve the superior orbital fissure (sphenocavernous or parasellar syndrome) or orbital apex and affect the optic nerve. Involvement of cranial nerves III, IV, and VI, the superior division of the fifth cranial nerve, as well as the sympathetic fibers in the cavernous ICA or parasympathetic fibers that surround the oculomotor nerve can occur secondary to granulomatous inflammation.
Diagnosis
Symptoms
Painful ophthalmoparesis or ophthalmoplegia is the hallmark of Tolosa-Hunt syndrome[3]. The patient may complain of double vision worse at distance, headaches, dizziness, nausea, neck stiffness, photophobia, blurred vision, and a “boring” pain may be associated with the headache.
Physical Exam
In addition to the standard ophthalmic examination of the patient including vision, IOP, pupil check for APD and nystagmus, slit-lamp and dilated fundus exam, a complete sensorimotor exam should be done. This includes oculomotor exam (to check for esotropia, exotropia, hypertropia or hypotropia), ductions, vergence, saccades, pursuit, and head tilt/turn. A common finding is abduction deficit associated with esodeviation that increases with gaze to the affected side. Lids should be checked for ptosis or lid retraction or any change in lid aperture during eye movements (to check for aberrant regeneration). Lid strength, fatigue or variability should be noted. Facial sensation should be checked. Stereopsis and color plates should also be evaluated.
Clinical diagnosis
Involvement of multiple contiguous cranial nerves strongly suggest a lesion in the cavernous sinus or subarachnoid space. Only one nerve may be involved, most likely the sixth cranial nerve, which is the only one not protected within the dural wall of the cavernous sinus.
In addition to the complete ophthalmic exam as described, the physician must closely look for Horner syndrome, facial hypoesthesia or engorgement of ocular surface vessels, orbital venous congestion, increased IOP or pulse pressure.
All positive findings should be noted and the differential diagnoses listed below should be considered.
Diagnostic Procedures
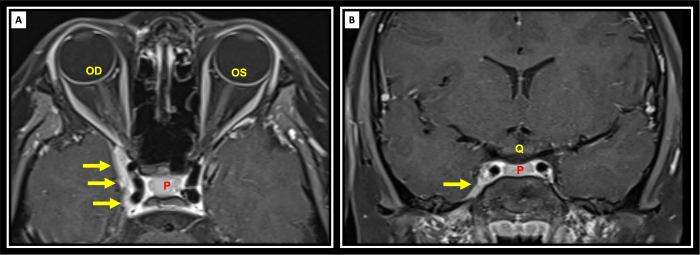
The most appropriate imaging includes MRI /MRA (DWI series) which provides information about the cavernous sinus and orbital apex in greater detail than a CT. MRI may be able to provide detail of granulomatous inflammation, aiding in formal diagnosis of Tolosa-Hunt syndrome. However, these results may be unreliable. Biopsy can also be used to demonstrate granulomatous inflammation and may be more reliable, but the procedure may be more difficult[3]
A CTA w/ and w/o contrast can also be obtained if an MRI/MRA is not available. A lumbar puncture may be done to check for opening pressure and CSF should be evaluated for infection/oligoclonal bands.
Recent evidence supports the use of High resolution 3D skull base MRI with isotropic constructive interference in steady state (CISS) and 0.6-mm cut images with and without contrast as effective way to visualize cranial nerves and cavernous sinus lesions that were not previously visualized.[4]
Laboratory Tests
Work up should include tests that can rule out the various diseases listed above given the history and context of the patient. This can include
Serum
- CBC w diff
- ESR
- CRP
- RPR and FTA-ABS
- ACE
- ANA
- p-ANCA, c-ANCA
- Anti dsDNA, Anti sm Antibody
- RF
- TFTs
- HBa1C and fasting glucose
- Lyme Panel
- Serum Protein Electrophoresis,
CSF: [5]
- Glucose
- Protein
- Cell count and differential (WBC, RBC)
- Cytology
- Culture
- Gram stain
- Oligoclonal bands
In few recent reports, associations with Pathogenic Nucleotide-Binding Oligomerization Domain 2 Polymorphism[6] and COVID-19 vaccination [7] have been reported.
Differential Diagnosis
Tolosa-Hunt syndrome is considered a diagnosis of exclusion. Thus, the following entities must be considered and ruled out before a diagnosis of Tolosa-Hunt syndrome is made:
- Ischemic disease: Hemorrhage, ischemic mononeuropathy
- Infectious process: post viral syndrome, chronic inflammation of petrous bone (recurrent ear infections), syphilis, basal meningitis
- Anatomical malformation: aneurysm, AVM, carotid-cavernous fistula, cavernous sinus thrombosis, pseudotumor cerebrii, Duane syndrome/Moebius syndrome, Chiari malformation
- Inflammatory disease: Sarcoidosis, granulomatosis with polyangiitis (formerly Wegener's), Behcet’s disease, IgG4 Disease
- Autoimmune condition: myasthenia gravis, thyroid disease, lupus
- Neoplastic disease: meningioma, neurogenic tumor, hemangioma, lymphoma/leukemia, schwannoma, pituitary adenoma, metastasis, CPA lesion, nasopharyngeal carcinoma, chordoma, chondrosarcoma, brain stem glioma in children
- Demyelinating disease: MS
- Others: Diabetes mellitus, Head trauma, BBPV, Meniere’s, ophthalmoplegic migraine
Management
Oral steroids are the mainstay of treatment. Both symptoms and physical exam findings (headache, ptosis, ophthalmoplegia, etc) can be expected to resolve rapidly with an oral steroid taper regimen over 3-4 months. The patient can be co-managed with the Neurology service to rule out other entities listed in the differential diagnosis of Tolosa-Hunt syndrome.
Before starting steroid, fungal infection of the orbit with fungal sinusitis (mucormycosis in diabetic/immunocompromised) is a differential diagnosis that must be considered, because in that case starting steroid will worsen the disease.
Several therapies have been investigated for instances of steroid-resistant Tolosa-Hunt syndrome. A case report by Lee, et al. has been published in which gamma-knife radiation therapy is used to provide marked short-term relief without relapse of symptoms[8]. Antimetabolic agents such as methotrexate, infliximab, and mycophenolate mofetil have also been shown to cause dramatic improvement in patients whom are deemed to be steroid-resistant[9][10][11]
Complications
A rare complication is aberrant regeneration of cranial nerves.
Prognosis
Prognosis of Tolosa-Hunt syndrome is excellent. Full recovery is expected with steroid treatment. The disease may have a relapsing-remitting course.
References
- ↑ Jump up to: 1.0 1.1 Tolosa E. Periarteritic lesions of the carotid siphon with the clinical features of a carotid infraclinoidal aneurysm. J Neurol Neurosurg Psychiatry 1954;17:300-2.doi:10.1136/jnnp.17.4.300
- ↑ Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211.
- ↑ Jump up to: 3.0 3.1 Mullen E, Green M, Hersh E, Iloreta AM, Bederson J, Shrivastava R. Tolosa-Hunt Syndrome: Appraising the ICHD-3 beta diagnostic criteria. Cephalalgia. 2018;38(10):1696-1700.
- ↑ Kontzialis M, Choudhri AF, Patel VR, Subramanian PS, Ishii M, Gallia GL, Aygun N, Blitz AM. High-Resolution 3D Magnetic Resonance Imaging of the Sixth Cranial Nerve, J of Neuro-Ophthalmol.Dec 2015; 35(4): 412-25 doi:10.1097/WNO.0000000000000313
- ↑ Amrutkar C, Burton EV. Tolosa-Hunt Syndrome. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459225/
- ↑ Vegunta, Sravanthi MD; Bohnsack, John MD; Crum, Alison MD; Digre, Kathleen MD; Katz, Bradley MD, PhD; Seay, Meagan DO; Quigley, Edward MD, PhD; Kennedy, Sean MD; Mamalis, Nick MD; Warner, Judith MD. Multiple Cranial Neuropathies and Pachymeningitis in a Patient With a Pathogenic Nucleotide-Binding Oligomerization Domain 2 Polymorphism. Journal of Neuro-Ophthalmology 41(4):p 547-552, December 2021. | DOI: 10.1097/WNO.0000000000001342
- ↑ Chuang TY, Burda K, Teklemariam E, Athar K. Tolosa-Hunt Syndrome Presenting After COVID-19 Vaccination. Cureus. 2021;13(7):e16791. Published 2021 Jul 31. doi:10.7759/cureus.16791
- ↑ Lee JM, Park JS, Koh EJ. Gamma Knife radiosurgery in steroid-intolerant Tolosa-Hunt syndrome: case report. Acta Neurochir (Wien). 2016;158(1):143-5
- ↑ Smith JR, Rosenbaum JT. A role for methotrexate in the management of non-infectious orbital inflammatory disease. Br J Ophthalmol. 2001;85(10):1220-4
- ↑ Halabi T, Sawaya R. Successful Treatment of Tolosa-Hunt Syndrome after a Single Infusion of Infliximab. J Clin Neurol. 2018;14(1):126-127
- ↑ Hatton MP, Rubin PA, Foster CS. Successful treatment of idiopathic orbital inflammation with mycophenolate mofetil. Am J Ophthalmol. 2005;140(5):916-8
- Albert et al. Principles and Practice of Ophthalmology. Third Edition. © 2008.
- Aligluo Z et al. Tolosa-Hunt syndrome: A case report. Journal of Neuroradiology. 1999. 26 (1): 68.
- BCSC series. Neuro-Ophthalmology. Section 5. American Academy of Ophthalmology.
- Dach F et al. Tolosa-Hunt syndrome: critical literature review based on IHS 2004 criteria. Cephalalgia an international journal of headache. 2007. 27 (8): 960-961.
- Duane’s Ophthalmology. Lipincott Williams & Wilkins. CD Rom 2006 Edition. www.oculist.net
- http://ihs-classification.org/de/
- Mendez et al. Painful ophthalmoplegia of the left eye in a 19-year-old female, with an emphasis in Tolosa-Hunt syndrome: a case report. Cases J. 2009; 2: 8271.
- Takahashi Y et al. Tolosa-Hunt Syndrome with Atypical Intrasellar and Juxtasellar Lesions:Two Case Reports. The Kurume Medical Journal. 1996. 43: 165-174.

