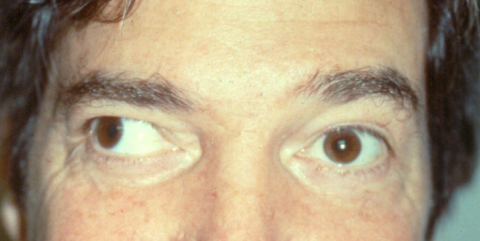
Exotropia
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Strabismus / ocular misalignment
Disease
Exotropia is a type of eye misalignment, where one eye deviates outward. The deviation may be constant or intermittent, and the deviating eye may always be one eye or may alternate between the two eyes.
Types
Pseudoexotropia
The term pseudoexotropia refers to a false appearance of exodeviation when in fact the eyes are properly aligned. Pseudoexotropia may occur when there is a wide inter pupillary distance or a positive angle Kappa (angle between the pupillary and visual axis).[2]
Exophoria
This is an exodeviation that is latent and is controlled by fusion under normal binocular viewing conditions. It is detected when binocular vision is interrupted during an alternate cover test. A high percentage of normal people, display a small exophoria on clinical examination, but is within normal limits and of no concern.
Congenital Exotropia/Infantile Exotropia
This is a large angle usually constant exodeviation with an onset in the first six months of life which does not resolve. There is an increased incidence with cerebral palsy and other neurologic disorders or craniofacial disorders. A careful developmental history is important and referral for neurologic assessment should be considered in these patient.
Sensory Exotropia
A blind or poorly seeing eye may drift outward. Infants or young children with a blind or poorly seeing eye usually develop esotropia (cross-eyes), but in children older than 2-4 years of age and adults, the eye will typically become exotropic.
Intermittent exotropia
This is the most common type of exodeviation. Onset is in childhood. There are 3 subtypes which will be discussed later in this article.
Convergence insufficiency
This type of exodeviation is often first noted in older children and teenagers. The exodeviation has greater magnitude at near fixation than at distance fixation.
Consecutive exotropia
This occurs when a person who was formerly esotropic becomes exotropic. In most cases this occurs from a surgical overcorrection of the esotropia.
Etiology
The etiology of exotropia is unknown, but on a rudimentary level there is impaired ability to maintain fusion and alignment. In the case of sensory exotropia, the poor acuity of one eye is the cause of the inability to maintain alignment.
Risk Factors
Neurologic disorders, prematurity, maternal substance and alcohol abuse during pregnancy, genetic abnormalities, uncorrected refractive errors and a family history of strabismus, all increase the risk of having exotropia.
General Pathology
Intermittent exotropia, the most common type of exotropia, has a usual onset between infancy and 7 years of age. There is no specific refractive error associated with exotropia. Although there is no specific racial predilection, Asians with strabismus are more often exotropic when compared to other racial groups.
Diagnosis
Symptoms
Symptoms may be mild or severe. If suppression of the deviating eye occurs, the patient can have diminished binocular vision and stereopsis. Those with later onset and milder frequency deviations can experience diplopia. Asthenopia can also occur with reading.
Exophoria
Many people will display exophoria on alternate-cover testing but have no symptoms. Occasionally may have symptoms of asthenopia.
Congenital/Infantile exotropia
Congenital exotropia has an onset during the first 6 months of life which is usually constant, large angle and does not resolve spontaneously.
Sensory exotropia
Sensory exotropia develops in older children or adults with one poorly seeing eye.
Intermittent exotropia
This is the most common type of manifest exodeviation. The intermittent deviation is more likely to be manifest when fatigued, ill, or in a lowered mental state (ex. ETOH use). It is more commonly manifest with distance fixation and also in bright sunlight. Types of intermittent exotropia[3]:
- Basic- The magnitude of distance and near deviations are within 10 prism diopters (units of measurement) of each other. These patients have normal convergence.
- Divergence excess- The angle of the exodeviation measures greater at distance than near by ≥ 10 prism diopters.
- Pseudo-divergence excess- The angle of the exodeviation measures greater at distance than near by ≥ 10 prism diopters but this difference becomes minimal after 60 minutes of monocular occlusion for 30-60 min.
- True divergence excess: The angle of the exodeviation measures greater at distance than near by ≥ 10 prism diopters but the difference persists even after monocular patching for 30-60 minutes and do not have high AC/A ratio.
- Divergence excess with high AC/A ratio: The angle of the exodeviation measures greater at distance than near by ≥ 10 prism diopters, which persists after monocular occlusion for 30-60 min and these patients have high AC/A ratio.
- Convergence insufficiency: The angle of the exodeviation measures greater at near than distance by ≥ 10 prism diopters.
Consecutive exotropia-
The patient has a history of esotropia treated with glasses or surgery, and subsequently converts to exodeviation.
Physical Examination
Pertinent Ophthalmological Examination Features for a person with exotropia:
- Visual Acuity
- Binocular function and stereopsis
- Motility evaluation
- Strabismus measurements (near, distance, extreme distance, and cardinal positions)
- Measures of fusional amplitudes
- Cycloplegic refraction
- In some cases - strabismus measurements after prolonged monocular occlusion and with +3.00 sphere near add test
- Evaluation of anterior and posterior ocular structures
Intermittent exotropia control in clinic may be categorized as follows[4]:
- Good control: Exotropia manifests only after cover testing, and the patient resumes fusion rapidly without blinking or refixating.
- Fair control: Exotropia manifests after fusion is disrupted by cover testing, and the patient resumes fusion only after blinking or refixating.
- Poor control: Exotropia manifests spontaneously and may remain manifest for an extended time.
Many ophthalmologist and researchers also use the Newcastle score to quantitatively grade the control of intermittent exotropia and it has been used in several clinical trials.[5]
| The Newcastle Control Score | |
| Home control | Score |
| Intermittent exotropia or monocular eye closure seen | |
| Never | 0 |
| <50% of time fixing in distance | 1 |
| >50% of time fixing in distance | 2 |
| >50% of time fixing in distance+seen at near | 3 |
| Clinic control | |
| Distance | |
| Immediate realignment after cover test | 0 |
| Realignment after blink or refixation | 1 |
| No realignment/manifest spontaneously | 2 |
| Near | |
| Immediate realignment after cover test | 0 |
| Realignment after blink or refixation | 1 |
| No realignment/manifest spontaneously | 2 |
| Total NCS = (home+near+distance) | |
Differential Diagnosis
Exotropia is not a disease entity by itself, it is a motility disturbance. Other conditions can display exotropia: Duane’s syndrome 3rd nerve palsy, Slipped or lost medial rectus muscle, Internuclear ophthalmoplegia, Orbital fibrosis.
Management
Nonsurgical
Treatment of the underlying treatable ocular condition or visual disturbance such as (ex. cataract, refractive error, amblyopia) needs to be addressed.
Nonsurgical treatments include: patching of the dominant eye or alternate eye patching in case there is no dominance seen [6][7], over-minus glasses[4], Botulinum toxin injection, and convergence exercises (for convergence insufficiency). Base in prism glasses can be used to relieve symptoms of diplopia or asthenopia. Effectiveness of non surgical treatments such as patching and over-minus glasses at times may only temporizing and these patients may eventually need surgical treatment. Pediatric Eye disease Investigator Group observational study showed that in children 3 to 10 years of age with intermittent exotropia and for whom surgery was not considered as the immediately needed treatment, stereoacuity deterioration or progression to constant exotropia over 3 years without any treatment was uncommon, and exotropia control, stereoacuity, and magnitude of deviation remained stable or improved slightly. [8]
Surgical
Performed to preserve or restore binocular function and alignment. Also may be performed for relief of diplopia and/or cosmesis. In general, long-term surgical success is better if the exotropia is intermittent instead of constant and the patient has better binocular function at the time of surgery. There is controversy as to the optimal time for surgical intervention. Surgery consists of operating on the extraocular muscles. The most common surgical procedure performed to treat intermittent exodeviation are either bilateral lateral rectus recession or unilateral lateral rectus recession and medial rectus resection. [9]
Additional Resources
- AAPOS website - frequently asked questions- topic: Exotropia
- https://www.aao.org/disease-review/intermittent-exotropia-2
References
- ↑ American Academy of Ophthalmology. Exotropia, right eye (adult). https://www.aao.org/image/exotropia-right-eye-adult-2 Accessed July 01, 2019.
- ↑ Wright KW, Spiegel PH. Pediatric Ophthalmology and Strabismus- The Requisites in Ophthalmology.1st ed.1999. Pp 246-252. Mosby.
- ↑ Burian HM. Exodeviations: their classification, diagnosis and treatment. Am Ophthalmol. 1966;62(6):1161-1166.
- ↑ 4.0 4.1 Kushner BJ. Conservative management of intermittent exotropia to defer or avoid surgery. J AAPOS. 2019 Oct;23(5):256.e1-256.e6
- ↑ Buck D, Hatt SR, Haggerty H, Hrisos S, Strong NP, Steen NI, Clarke MP. The use of the Newcastle Control Score in the management of intermittent exotropia. Br J Ophthalmol. 2007 Feb;91(2):215-8.
- ↑ Freeman RS, Isenberg SJ. The use of part-time occlusion for early onset unilateral exotropia. J Pediatr Ophthalmol Strabismus 26:94. 1989.
- ↑ Pediatric Eye Disease Investigator Group; Writing Committee, Mohney BG, Cotter SA, Chandler DL, Holmes JM, Wallace DK, Yamada T, Petersen DB, Kraker RT, Morse CL, Melia BM, Wu R. Three-Year Observation of Children 3 to 10 Years of Age with Untreated Intermittent Exotropia. Ophthalmology. 2019 Sep;126(9):1249-1260
- ↑ Pediatric Eye Disease Investigator Group; Writing Committee, Mohney BG, Cotter SA, Chandler DL, Holmes JM, Wallace DK, Yamada T, Petersen DB, Kraker RT, Morse CL, Melia BM, Wu R. Three-Year Observation of Children 3 to 10 Years of Age with Untreated Intermittent Exotropia. Ophthalmology. 2019 Sep;126(9):1249-1260.
- ↑ Pediatric Eye Disease Investigator Group; Writing Committee, Donahue SP, Chandler DL, Holmes JM, Arthur BW, Paysse EA, Wallace DK, Petersen DB, Melia BM, Kraker RT, Miller AM. A Randomized Trial Comparing Bilateral Lateral Rectus Recession versus Unilateral Recess and Resect for Basic-Type Intermittent Exotropia. Ophthalmology. 2019 Feb;126(2):305-317.