Iris Trauma Repair
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Trauma to the iris can present in various ways depending on its location and severity. Tears at the pupillary border can damage the sphincter muscle, thus leading to an atonic, mydriatic, or partially reactive pupil. Tears at the iris root lead to iridodialysis. Furthermore, tears can be full thickness through the iris stroma or partial thickness, involving only the posterior pigment epithelium leading to trans-illumination defects. This article will cover the technique to repair full-thickness iris tears as well as to repair atonic and mydriatic pupils.
Anatomy
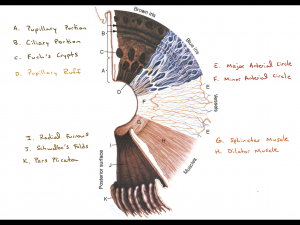
The iris is mostly comprised of a network of connective tissue, blood vessels, and melanocytes. The connective tissue, containing collagen fibrils of hyaluronic acid, creates the stroma of the iris and provides the elasticity and stretch noted during surgical manipulation. The stroma contains multiple crypts to allow for the passage of aqueous humor into the anterior chamber. The vascular network is comprised of the major arterial circle, which is located at the anterior portion of the ciliary body, and the minor arterial circle, which interweaves through the iris stroma. This radial vascular network is responsible for the bleeding seen in the anterior chamber during trauma to the iris.
The posterior aspect of the iris is comprised of a smooth layer of densely pigmented epithelium that wraps around the pupillary border, creating the pupillary ruff. Just anterior to the posterior pigmented epithelium lies the sphincter and dilator muscles. Figure 1 illustrates the structures of the iris.
Pathogenesis & Risk Factors
Penetrating wounds, either via foreign objects lacerating the globe or iatrogenic due to surgical trauma during complex anterior segment surgery, are the primary reasons for full-thickness iris defects. Iris defects may also be seen in hereditary conditions such as iris coloboma, ICE syndrome, and other diseases. Full-thickness iris defects are also created when performing laser peripheral iridotomies for pupillary block glaucoma or prophylactically in preparation for the placement of Intracameral Collamer Lenses (ICLs). However, iridotomies may cause photic symptoms if they are not placed sufficiently peripheral or made too large due to the upper eyelid tear meniscus creating a prismatic effect[1].
Blunt ocular trauma is primarily responsible for iridodialysis, but it may also be present with penetrating injuries.
Patients at high risk for iatrogenic surgical trauma to the iris include those with a history or a predisposition of Intraoperative Iris Floppy Syndrome (IFIS), pseudoexfoliation syndrome, or a history of iritis.
Diagnosis
History
Patients with photic symptoms due to iris defects report glare, haloes in brightly lit conditions, and trouble reading. Those with atonic, mydriatic pupils report worse glare at night and inability to focus at near. Patients should also be assessed for any prior history of ocular trauma, history of uveitis, history of benign prostate hypertrophy, surgical history, as well as a detailed medication history to include the use of alpha-blockers or steroids.
Physical Exam
The slit lamp exam should be performed prior to pupillary dilation. In patients presenting with an ocular laceration and concomitant iris laceration, the primary goal of the surgery should be to perform a water-tight closure of the globe. After successful closure, an assessment should be made regarding the severity of iris laceration, presence of concomitant iridodialysis, traumatic or subluxation of the lens, and vitreous or retina within the anterior chamber. The repair of the iris laceration should be delayed until a definitive assessment of the posterior segment can be performed with indirect ophthalmoscopy and/or a B-scan ultrasound.
Prior to the repair of iris defects, the slit lamp exam should evaluate for instability in the lens-bag-zonule complex if the patient is still phakic, as oftentimes these cases also require removal of the traumatic and subluxated lens and suture fixation of a scleral intraocular lens (IOL)[2][3]. The exam should also note any iris atrophy, trans-illumination defects, synechiae, or exfoliative material in the contralateral eye. The pupillary margin should be assessed for sphincter tears, neovascularization, or ectropion uveae.
A gonioscopy exam should be performed when permitted, barring the patient not present with an ocular laceration, to check for neovascularization of the angle or tears in the iris root or peripheral anterior synechiae.
Surgical Management
Pre-operative Planning
Repairing iris defects can be challenging; therefore, creating a favorable environment within the anterior chamber (AC) will ensure success. Below are tips that can help facilitate success and avoid complications:
- Repair should be conducted in aphakic or pseudophakic eyes, as the risk of capsular tear is high in phakic eyes.
- It is recommended to block the eye, either via a peribulbar or retrobulbar block.
- Miochol or miostat should be used to pharmacologically constrict the pupil as much as possible.
- Centripetal mechanical pulling of the iris helps to loosen and stretch the tissue in preparation for suturing.
- Ensure the eye has ample viscoelastic to protect the corneal endothelium as well as in the ciliary sulcus to slightly tent up the iris for an easier pass of the suture. Using an AC maintainer or pars plana infusion in vitrectomized eyes is beneficial.
- Docking the needle into a 25-gauge cannula as the needle enters and exits the AC can help to prevent an inadvertent pass through Descemet’s membrane.
Instruments and Supplies
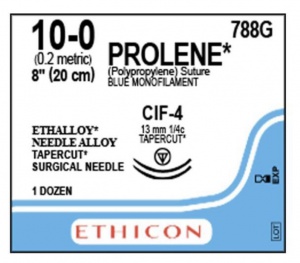
- 10-0 Prolene suture on a 13mm CIF-4 needle or alternatively on a CTC-6L needle
- Micrograsping forceps (MST micrograsping forceps or Alcon Maxgrip forceps)
- Kuglen hook or Sinskey Hook
- Lewicki AC Maintainer
- Viscoelastic
- Angled tying forceps
Techniques for Repair of Iris Tears
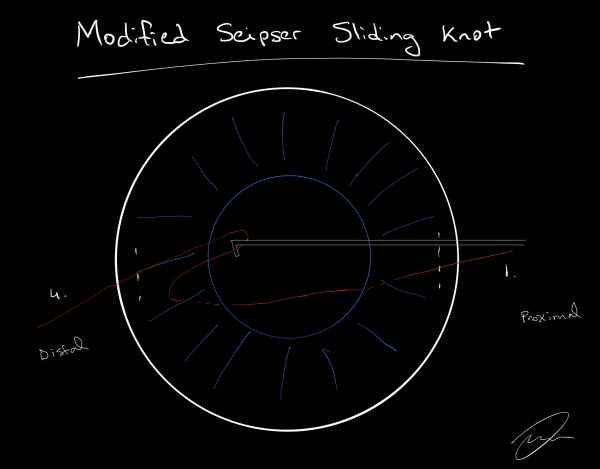
Modified Seipser Sliding Knot[4][5][6]
- Two paracentesis wounds are created across from each other, overlying the iris defect.
- A 10-0 prolene suture on a CIF4 needle is entered through the paracentesis. Care must be taken to avoid passing the needle through the descemet’s membrane while entering and exiting the AC.
- The suture is placed through the iris defect and exited through the opposite paracentesis. Micro-grasping forceps can be used to grasp the iris while making the needle pass.
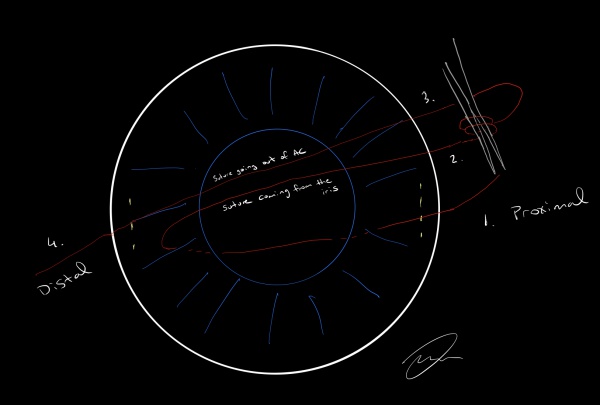
- The distal suture (labeled 4 in Figure 2) is retrieved as a loop with a Kuglen hook and pulled through the paracentesis.
- The portion of the loop coming from the iris (2) is wrapped around the angled ties twice and grasped to the proximal suture (1).
- While holding the proximal suture with the angle ties (1), the distal suture (4) is pulled to allow the knot to slip into the AC and approximate the iris edges.
- Steps 4-6 are then repeated, but the loop is only wrapped around once to place the locking knot.
- The knot is cut with micro-scissors close to the iris.
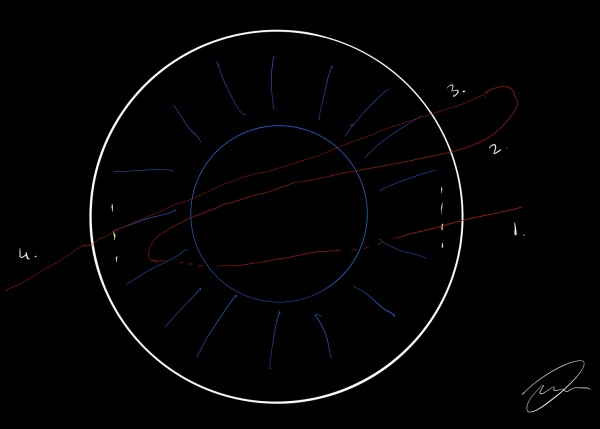
Single Four-Throw (SFT) Pupilloplasty This technique, introduced by Dr. Amar Agarwal, is an efficient way to close an iris defect as it only requires a single loop of suture to secure the defect[7]. In this technique, the suture (labeled 2 in the image) is wrapped 4 times around the angled ties (instead of twice) and grasped to the proximal suture (labeled 1 in the image). The distal suture (4) and the proximal suture (1) are tied together to advance the knot into the AC and secure the iris. The ends of the sutures are then cut with micro scissors leaving a small suture tail. There is no need to create a second loop of suture, as the knot is self-retaining due to the formation of a helical structure of thread that presses across itself. The suture material has to be wrapped around itself at least 4 times in order to create a self-retaining knot[8].
Source: https://theophthalmologist.com/subspecialties/sft-are-you-in-the-loop
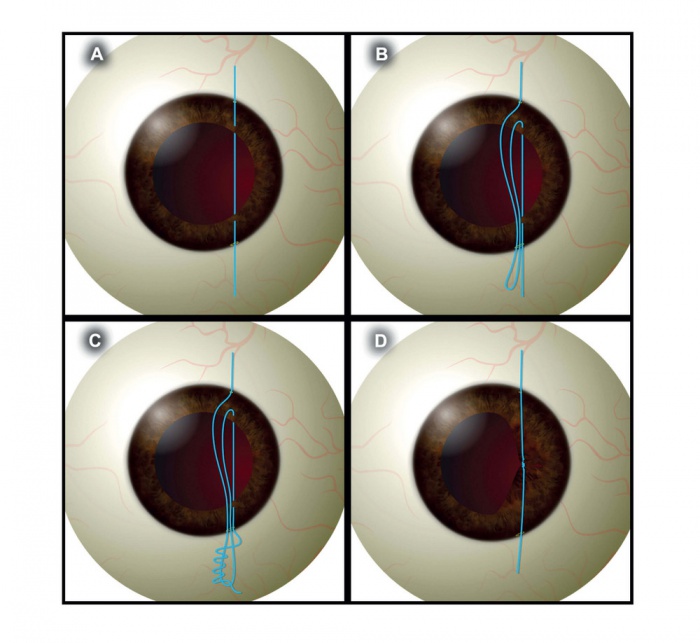
Iris Cerclage This technique is used to surgically constrict an atonic mydriatic pupil and involves creating a running baseball-like stitch along the pupillary border[9]. Three paracentesis wounds are created. Multiple small (~1-2mm) bites are taken at the pupillary border to secure around 90 degrees of the iris. The needle is externalized through the para wound and redirected to complete the next quadrant. This is repeated until the iris has been sutured for 360 degrees. The suture can then be tied utilizing the McCannel technique. However, this technique has fallen out of favor, given the speed at which multiple SFT iris sutures can be placed to constrict the pupil[10].
Video of iris cerclage: https://www.aao.org/annual-meeting-video/surgical-repair-of-atonic-pupil-with-iris-cerclage
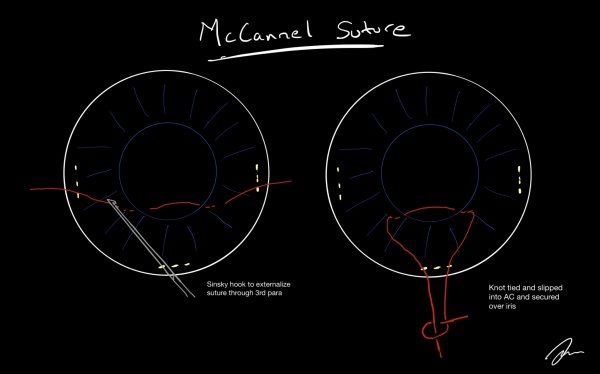
McCannel Suture Technique[6][11]
Below is a depiction of McCannel suture technique. The suture pass is made just as described previously, but both arms of the suture are externalized through a third paracentesis wound. The suture is then tied in a normal fashion and slipped into the AC, and secured over the iris.
Complications
- Hyphema
- Iridodialysis
- Endophthalmitis
- Corneal Edema
- Vitreous Loss
- Cystoid Macular Edema
- IOL decentration or dislocation
- Glaucoma
- Retinal Tear or Detachment
References
- ↑ Spaeth GL, Idowu O, Seligsohn A, et al. The effects of iridotomy size and position on symptoms following laser peripheral iridotomy. J Glaucoma. 2005;14:5:364-367.
- ↑ Carlson A. Repairing the Iris during Cataract Surgery. CRST. Apr 2014. https://crstoday.com/articles/2014-apr/repairing-the-iris-during-cataract-surgery/
- ↑ Wagoner MD, Cox TA, Ariyasu RG, Jacobs DS, Karp CL. American Academy of Ophthalmology. Intraocular lens implantation in the absence of capsular support: A report by the American Academy of Ophthalmology. Ophthalmology. 2003;110:840–59.
- ↑ Siepser SB. The closed-chamber slipping suture technique for iris repair. Ann Ophthalmol.1994:26:71-72.
- ↑ Osher RH, Snyder ME, Cionni RJ. Modification of the Siepser slip-knot technique. J Cataract Refract Surg. 2005;31:1098–1100. doi:10.1016/j.jcrs.2004.11.038
- ↑ Jump up to: 6.0 6.1 Lian RR1, Siepser SB2, Afshari NA1. Iris Reconstruction Suturing Techniques. Curr Opin Ophthalmol. 2020 Jan;31(1):43-49. doi: 10.1097/ICU.0000000000000628.
- ↑ Narang, P., & Agarwal, A. (2017). Single-Pass Four-Throw Technique for Pupilloplasty. European Journal of Ophthalmology, 27(4), 506–508. https://doi.org/10.5301/ejo.5000922
- ↑ Narang P. Agarwal A. Single-Pass Four-Throw Pupilloplasty Knot Mechanics. Journal of Refractive Surgery. 2019;35(3):207-208.
- ↑ Ogawa GS. The iris cerclage suture for permanent mydriasis: a running suture technique Ophthalmic Surg Lasers. 1998 Dec;29(12):1001-9.
- ↑ Agarwal A. Narang P. Single Four Throw Pupilloplasty - Are You in the Loop. The Ophthalmologist. Feb 2019. https://theophthalmologist.com/subspecialties/sft-are-you-in-the-loop
- ↑ Weissbart SB1, Ayres BD. Management of aniridia and iris defects: an update on iris prosthesis options. Curr Opin Ophthalmol. 2016 May;27(3):244-9. doi: 10.1097/ICU.0000000000000253.