Orbital Apex Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Orbital Apex Syndrome (also known as Jacod syndrome)
Disease
Orbital apex syndrome (OAS) involves cranial neuropathies in association with optic nerve dysfunction. Orbital apex syndrome is symptomatically related to superior orbital fissure syndrome and cavernous sinus syndrome with similar etiologies. The distinction is the precise anatomic involvement of the disease process.[1]
Anatomy[1][2]
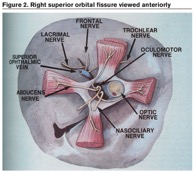
The orbital apex is anatomically the posterior part of the orbit positioned at the craniofacial junction located where the four orbital walls converge. The orbital apex incorporates the optic canal and the superior orbital fissure. The optic canal transmits the optic nerve (surrounded by meninges) and the ophthalmic artery to the cranial fossa. The superior orbital fissure is anatomically lateral to the optic canal which can be divided into the superior, middle, and inferior portions by the common tendinous ring comprised of the thickened periorbita lining the surface of the orbital bones. The contents of the optic canal and the middle portion of the superior orbital fissure course through the common tendinous ring. The superior portion transmits the lacrimal nerve (CNV1), frontal nerve (CNV1), trochlear nerve (CNIV), superior branch of the ophthalmic vein, and recurrent meningeal artery. The middle portion transmits the nasociliary nerve (CN V1), abducens nerve (CNVI), and the superior and inferior branches of the oculomotor nerve (CNIII). The inferior portion transmits the inferior branch of the ophthalmic vein.
Etiology[1]
Variety of etiologies and detailed history is important in narrowing the differential diagnosis.
- Inflammatory
- Sarcoidosis, SLE, Churg-Strauss syndrome, granulomatosis with polyangiitis , Tolosa Hunt Syndrome, Giant cell arteritis, Orbital inflammatory pseudotumor, thyroid orbitopathy, IgG4 related orbital myositis
- Infectious – Most often associated with invasive fungal sinusitis or post-septal bacterial orbital cellulitis.[4] It is also important to recognize the possibility of aggressive bacterial sinusitis without cellulitis causing an OAS.[5]
- Fungi: aspergillosis, Mucormycosis
- Bacteria: streptococcus, staphylococcus, actinomyces, gram-negative bacilli, anaerobes, mycobacterium tuberculosis
- Spirochetes: treponema pallidum
- Viruses: Herpes Zoster
- Neoplastic
- Head and neck tumors: nasopharyngeal carcinoma with extension into the orbit, primary orbital adenoid cystic carcinoma with extension to the orbital apex
- Neural tumors: neurofibroma, meningioma, glioma, ciliary neurinoma, schwannoma
- Metastatic lesions: lung, breast, renal cell, melanoma
- Hematologic: Burkitt lymphoma, non-Hodgkin lymphoma, leukemia
- Perineural invasion of cutaneous malignancy: squamous cell cancer
- Iatrogenic/Traumatic – Traumatic/Iatrogenic causes can lead to orbital apex syndrome via direct or indirect injury. Direct injury typically results from displaced bony fragments leading to anatomic compression of the contiguous nerves and vessels. Indirect injuries result from shearing forces to the anatomic structures of the superior orbital fissure and/or optic nerve from high impact forces. [6]
- Iatrogenic: sinonasal surgery, orbital/facial surgery
- Traumatic: penetrating, nonpenetrating, orbital apex fracture
- Vascular
- Carotid cavernous aneurysm, carotid cavernous fistula, cavernous sinus thrombosis
- Other: Mucocele, fibrous dysplasia, neurofibromatosis
Pathophysiology
In the orbital apex syndrome dysfunction of the optic nerve (II), oculomotor nerve (III), trochlear nerve (IV), abducens nerve (VI), and/or the ophthalmic branch of the trigeminal nerve (V1) may occur. The exact etiology is protean but may be generally divided into inflammatory, infectious, neoplastic, traumatic, and iatrogenic causes.
Signs/Symptoms
- The most common initial manifestation of OAS is visual loss and ophthalmoplegia involving multiple cranial nerves
- Visual loss is due to CNII involvement. Optic disc edema or subsequent optic atrophy may develop within weeks to months.
- Ophthalmoplegia with variable diplopia, mydriasis, and ptosis due to CNIII, IV, VI involvement
- Absence of corneal sensations and corneal reflex
- Pupillary abnormalities: Relative Afferent Pupillary Defect (RAPD)
- Choroidal folds
- Periorbital/facial pain and hypoesthesia of the forehead due to CNV involvement.
- Proptosis with or without orbital congestion
- Chemosis and/or conjunctival injection
Differential diagnosis
- Superior Orbital Fissure Syndrome (SOFS)
- SOFS may involve any of the structures coursing through the superior orbital fissure anterior to the orbital apex which include CNIII, CNIV, CNV1, CNVI, and the ophthalmic veins. While superior orbital fissure syndrome may manifest with dysfunction of multiple oculomotor cranial neuropathies, it is dysfunction of the optic nerve function that differentiates orbital apex syndrome from SOFS.
- Cavernous Sinus Syndrome (CSS)
- Cavernous sinus syndrome may also present with multiple oculomotor cranial neuropathies, including III, IV, VI, and sensory dysfunction from involvement of V1. The internal carotid artery may also be involved with the primary process in CSS. Optic nerve dysfunction should not occur in CSS.
Management
Inflammatory
- Many inflammatory etiologies require treatment of the primary process and reduction of inflammation using systemic immunomodulatory agents which include corticosteroids and steroid-sparing agents.[7] Decompressive surgery to provide an anatomic expansion of the orbit and radiation therapy to alleviate inflammation causing compression of optic nerve in thyroid orbitopathy can be pursued.[8]
Infectious
- Treatment usually entails administration of the appropriate broad-spectrum anti-microbial therapy. Surgical intervention via a direct or endoscopic approach may be necessary in cases of orbital abscess or subperiosteal abscess. [7]
Neoplastic
- Management is dependent on the etiology and can include surgical resection, radiation therapy, or chemotherapy as possible treatment options.
Iatrogenic/Traumatic
- CT may show comminuted fractures.
- Of concern is orbital compartment syndrome which may require corticosteroids and decompressive surgery to alleviate cranial nerve dysfunction.[9] Orbital compartment syndrome may result in optic nerve damage and permanent visual loss depending on the time course of events.[6]
Vascular
- CT and MRI are required to diagnose.
- Generally, CCF and CCA’s can be managed conservatively; however, those that cause significant cranial nerve dysfunction require further intervention which may include endovascular or surgical intervention.[10][11]
- Cavernous sinus thrombosis requires anticoagulation, possible adjunctive corticosteroid therapy, and aggressive broad-spectrum antibiotic therapy if septic.[12]
References
- ↑ Jump up to: 1.0 1.1 1.2 Yeh, S., & Foroozan, R. (2004). Orbital apex syndrome. Current Opinion in Ophthalmology,15(6), 490-498. doi:10.1097/01.icu.0000144387.12739.9c
- ↑ Rai S and Rattan V. Traumatic superior orbital fissure syndrome: Review of literature and report of three cases. Natl J Maxillofac Surg 2012; 3: 222–225.
- ↑ Yeh, S., & Foroozan, R. (2004). Orbital apex syndrome. Current Opinion in Ophthalmology,15(6), 490-498. doi:10.1097/01.icu.0000144387.12739.9c
- ↑ American Academy of Ophthalmology. Orbital Cellulitis. Focal Points - Excerpt. https://www.aao.org/education/focalpoints Accessed 25 September 2024.
- ↑ Pfeiffer, M. L., Merritt, H. A., Bailey, L. A., Richani, K., & Phillips, M. E. (2018). Orbital apex syndrome from bacterial sinusitis without orbital cellulitis. American Journal of Ophthalmology Case Reports,10, 84-86. doi:10.1016/j.ajoc.2018.01.041
- ↑ Jump up to: 6.0 6.1 Warner N and Eggenberger E. Traumatic optic neuropathy: A review of the current literature. Curr Opin Ophthalmol 2010; 21:459–462
- ↑ Jump up to: 7.0 7.1 Robinson, D., Wilcsek, G., & Sacks, R. (2011). Orbit and Orbital Apex. Otolaryngologic Clinics of North America,44(4), 903-922. doi:10.1016/j.otc.2011.06.011
- ↑ Rocca, R. D. (2007). Thyroid-Related Orbitopathy: Concepts and Management. Facial Plastic Surgery, 23(3), 168-173. doi:10.1055/s-2007-984556
- ↑ Chen CT and Chen YR. Traumatic superior orbital fissure syndrome: Current management. Craniomaxillofac Trauma Reconstr 2010; 3: 9–16
- ↑ Ellis, J. A., Goldstein, H., Connolly, E. S., & Meyers, P. M. (2012).Carotid-cavernous fistulas. Neurosurgical Focus,32(5). doi:10.3171/2012.2.focus1223
- ↑ Eddleman, C. S., Hurley, M. C., Bendok, B. R., & Batjer, H. H. (2009). Cavernous carotid aneurysms: To treat or not to treat? Neurosurgical Focus,26(5). doi:10.3171/2009.2.focus0920
- ↑ Coutinho JM and Stam J. How to treat cerebral venous and sinus thrombosis. J Thromb Haemost 2010; 8: 877–883

