Hughes Procedure
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
The Hughes procedure, or tarsoconjunctival flap advancement, is a frequently utilized technique to repair full-thickness lower eyelid defects involving > 50% of the lower eyelid margin.[1] The procedure was first presented and popularized by Dr. Wendel Hughes, a pioneer in oculoplastic surgery, in 1937.[2] The procedure is a dual-stage, “eyelid-sharing” surgery with the first stage involving advancement of a tarsoconjunctival flap from the upper eyelid to the lower eyelid to reconstruct the posterior lamella. Reconstruction of the lower eyelid anterior lamella is done using a skin-muscle advancement flap, local skin, or free full-thickness skin graft.[1][3]
Traditionally, the second stage of the procedure, severance of the flap, occurred 3 to 4 months after the initial stage. In 1989, Silkiss et al through analysis of a rabbit model and in vivo evaluation determined that the flap could be severed as early as one week.[4] Now, the standard time to flap division is frequently 2 weeks, depending on surgeon preference, patient comorbities, and convenience. This second stage involves separating the flap at the new lower eyelid margin and opening the eyelids.[3][4] Some authors advocate that division at 7 days can still lead to a good functional and aesthetic outcome.[5]
The modified Hughes procedure includes sparing of the marginal upper lid tarsus and removal of the levator muscle aponeuorsis from the tarsoconjunctival flap.[3][6] This greatly reduces the rate of upper lid complications, such as upper lid retraction, trichasis, and entropion.[3][7] The Hughes procedure is not the procedure of choice in monocular patients needing lower eyelid reconstruction on their seeing eye as it leads to temporary visual obstruction.[3]
The Hughes procedure differs from the Hewes flap, another technique used to repair lower eyelid defects. The Hewes flap was first described by Eva Hewes in 1976 and is a one-stage technique to reconstruct the lower eyelid using a tarsoconjunctival flap transposed from the upper eyelid and hinged at the lateral canthal tendon. An advantage of the Hewes flap is that occlusion of the eye is unnecessary.[8]
Another notable eyelid sharing procedure is the Cutler-Beard procedure, which is used to repair full thickness upper eyelid defects. However, as compared to the Hughes procedure, the Cutler-Beard flap excludes the tarsal plate, since there is not enough tarsal plate in the lower lid to provide adequate support to the upper and lower lids after the procedure.[9][10]
Indications
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Sebaceous Cell Carcinoma
- Melanoma
- Merkel Cell Carcinoma
- Other Eyelid Malignancy
- Trauma
Procedure
Adopted from the AAO Basic Techniques of Ophthalmic Surgery (2015)[1]
- Under intravenous sedation, a 50:50 mixture of 2% lidocaine with 1: 100,000 epinephrine, 0.5% Marcaine with 1:200,00 epinephrine, sodium bicarbonate, and hyaluronidase is infiltrated into the upper and lower eyelids via the conjunctival surface.
- The patient is prepped and draped in the usual sterile fashion.
- A 5-0 silk suture is placed through the central upper lid margin. A Desmarres retractor is used to evert the upper eyelid.
- A 15 blade is used to incise the conjunctiva and tarsus. This incision should begin approximately 3-4 mm above the eyelid margin and extend parallel to the upper eyelid margin. The length is determined by the horizontal extent of the lower lid defect to be repaired. Care is taken to provide for adequate horizontal tension to avoid post-operative buckling.
- The #15 BP blade is used to extent the cuts vertically superior to the superior edge of tarsus on both sides of the original horizontal incision.
- The flap is elevated using forceps and blunt dissection is performed with the Colorado blade of the monopolar cautery to separate the tarsal-conjunctival flap from the underlying tissues.
- Steven scissors are used to extend the conjunctival incision to the superior fornix, dissecting Muller’s muscle off the conjunctiva as best as possible.
- The Desmarres retractor is removed. The mobilized tarsal-conjunctival flap is rotated inferiorly into the lower eyelid defect. The superior border of the tarsus should be flush with the remaining lower eyelid margins on either side.
- The tarsal-conjunctival flap is then attached to the remaining lower eyelid tarsus on either side and to the remaining lower eyelid retractors inferiorly using interrupted 6-0 polyglactin or vicryl suture.
- The anterior lamella of the lid can then be created by:
- A myocutaneous advancement flap, if sufficient lid laxity
- A myocutaneous transposition flap from the upper eyelid
- A full thickness skin graft using either postauricular, supraclavicular, or upper eyelid skin.
- Prophylactic antibiotic ointment is placed on the incision at the close of the procedure and up to twice times until the sutures dissolve or the flap severed.
- Separation of the eyelids takes place generally anywhere beyond 2 weeks after the first stage of the procedure. This is done by cutting across the flap at the level of the intended lower eyelid margin beveling the scissor to avoid future conjunctival creep onto the anterior surface of reconstructed eyelid.
Outcomes and Complications
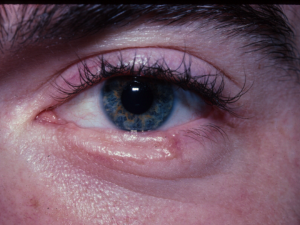
The Hughes procedure has high functional and aesthetic success. In a recent study by Hishmi et al, surgical success, defined as normal lid function and satisfactory cosmesis without the need for additional surgery was achieved in 39 of 45 cases (87%).[3]
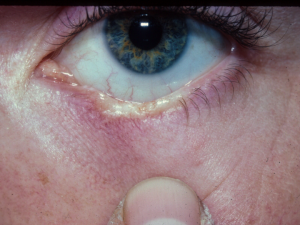
The complication rate after Hughes tarsoconjunctival flap advancement is low. Common complications include lower lid margin erythema, lower lid ectropion, eyelid retraction, entropion, trichiasis, lagophthalmos, pyogenic granuloma, infection, and flap suture dehiscence.[1][3][6] Conjunctival creep onto the lid margin, as well as buckling may occur, requiring revision. Eyelid retraction may be avoided by ensuring dissection of the advanced Mueller’s muscle back into the superior cul de sac after flap severance.
McKelvie et al published long-term outcomes of 122 consecutive cases of lower eyelid repair using the Hughes tarsoconjunctival flap advancement. They reported an overall complication rate of 14% (17 cases), with only 5 cases out of 122 requiring surgical revision.[11]
In summary, the Hughes procedure should be considered for any full thickness lower eyelid defect involving a significant portion of the lower eyelid margin.
Additional Resources
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 Hausheer JR. Basic techniques of ophthalmic surgery. San Francisco: American Academy of Ophthalmology; 2015.
- ↑ McClellan WT, Rawson AE. Wendell L. Hughes' life and contributions to plastic surgery. Plastic and reconstructive surgery. 2011;128(6):765e-772e
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Hishmi AM, Koch KR, Matthaei M, Bölke E, Cursiefen C, Heindl LM. Modified Hughes procedure for reconstruction of large full-thickness lower eyelid defects following tumor resection. European Journal of Medical Research. 2016;21.
- ↑ Jump up to: 4.0 4.1 Silkiss RZ, Glasgow BJ, Baylis HI. Revascularization studies of an opposing eyelid pedicle flap. Ophthalmic plastic and reconstructive surgery. 1989;5(2):110-117
- ↑ Leibovitch I, Selva D. Modified Hughes flap: division at 7 days. Ophthalmology. 2004;111(12):2164-2167
- ↑ Jump up to: 6.0 6.1 Rohrich RJ, Zbar RI. The evolution of the Hughes tarsoconjunctival flap for the lower eyelid reconstruction. Plastic and reconstructive surgery. 1999;104(2):518-522; quiz 523; discussion 524-516.
- ↑ Cies WA, Bartlett RE. Modification of the Mustarde and Hughes methods of reconstructing the lower lid. Annals of ophthalmology. 1975;7(11):1497-1502.
- ↑ Hewes EH, Sullivan JH, Beard C. Lower eyelid reconstruction by tarsal transposition. American journal of ophthalmology. 1976;81(4):512-514.
- ↑ Mandal SK, Fleming JC, Reddy SG, Fowler BT. Total Upper Eyelid Reconstruction with Modified Cutler-Beard Procedure Using Autogenous Auricular Cartilage. Journal of Clinical and Diagnostic Research : JCDR. 2016;10(8):Nc01-04.
- ↑ Cutler NL, Beard C. A method for partial and total upper lid reconstruction. American journal of ophthalmology. 1955;39(1):1-7
- ↑ McKelvie J, Ferguson R, Ng SGJ. Eyelid reconstruction using the "Hughes" tarsoconjunctival advancement flap: Long-term outcomes in 122 consecutive cases over a 13-year period. Orbit (Amsterdam, Netherlands). 2017;36(4):228-233