Entropion
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
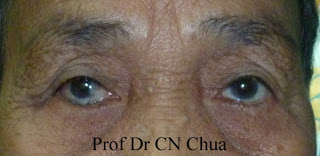
Entropion is an inward turning of the eyelid margin and appendages such that the pilosebaceous unit and mucocutaneous junction are directed posteriorly towards the cornea and ocular surface. It is one of the most common eyelid malpositions seen mainly in the elderly. It may occur either in the upper or lower eyelids, with lower eyelid entropion most likely to be involutional and upper eyelid entropion typically cicatricial. Inward turning of the eyelid margin can cause corneal and conjunctival damage leading to corneal stromal abrasion, scarring, corneal thinning and corneal neovascularization. In advanced cases, there is even a risk of corneal ulcer and perforation hence necessitating prompt management.[1] Specific types of the condition include marginal entropion and Meibomian Gland Inversion(MGI) - typically seen in the upper eyelid.
ICD 9 Code
Entropion ICD 9 374.00
Epidemiology
In a study of nearly 25,000 individuals over 60 years old, involutional entropion was found in 2.1% of patients, lesser than involutional ectropion. Prevalence increased with age: 0.9% for patient 60-69 years old, 2.1% for 70-79, and 7.6% for those over 80. Bilateral disease is three times more common than unilateral. Entropion is more common in women, with prevalence 2.4%, compared to 1.9% in men. Involutional entropion has a reported prevalence of 2.4% in whites and 0.8% in blacks.[2] Likewise in East Asians, involutional entropion is proportionately more common than ectropion relative to the Caucasian population.
Patients with involutional entropion are often elderly and have significant comorbidities. The 4-year mortality for patients with involutional entropion is 30%.[3]
Anatomy and Pathophysiology
Involutional entropion is due to a combination of causative factors: loss of horizontal lid support with canthal tendon laxity; disinsertion, atrophy or dehiscence of lower lid retractors; overriding of the preseptal over pretarsal orbicularis oculi; loss of vertical lid support with tarsal atrophy; and orbital fat atrophy leading to enophthalmos that allows inversion of the lid margin.[4]
An understanding of the relevant anatomy is required to explain and treat this mechanical condition. The lower lid derives stability from the tone of the pretarsal orbicularis oculi, lower lid retractors and integrity of the tarsus and canthal tendons. Loosening of horizontal tension of these structures, especially the lateral canthal tendon, predisposes the lid margin to rotate. The lower lid retractors provide vertical stability and are analogous structures to the levator aponeurosis and Muller's muscle in the upper lid. The capsulopapebral head of the lower eyelid retractors surrounds the inferior oblique and forms part of the Lockwood ligament before fusing with the septum at the inferior border of the tarsal plate.[1] Patients with involutional entropion have on average 1.4mm increased distance between the lower lid retractors and the inferior border of the tarsal plate.[5] The posterior layer of the lower lid retractors provides the most traction on the lid.[6] Loosening of these vertical stabilizing structures allows the lid to rotate inward.[1]
The lower lid retractors have fine extensions to the orbicularis oculi and overlying skin. As these connections weaken or dehisce, the preseptal orbicularis can travel superiorly and override the pretarsal muscle rotating the eyelid margin against the globe.[1] Cadaveric research showed that elderly patients had clear override of the preseptal over the pretarsal orbicularis oculi in the lower lid, with the override sometimes extending up to the eyelid margin. However, 10 of 11 upper eyelids showed no orbicularis override, and the single case of override was mild.[7]
Histologic examination of tarsal plates in patients with involutional entropion showed degenerated and disorganized collagen fibers with abnormal elastogenesis.[8] Collagen fibers provide tensile strength to the tarsus, and elastic fibers give the tarsus resilience.[9][10] With aging, the tarsus shifts from being mainly collagenous fibers to elastic fibers,[8] and the total number of collagen and fibers decrease.[11][12][13] This shift in fiber population is associated with increased horizontal eyelid laxity,[14] and tarsal atrophy has been asociated with entropion.[15] Smaller tarsal plates allow for more horizontal lid laxity[8][14] and orbicularis override.[15] Females have smaller tarsal plates than males,[15] which explains in part why entropion is more prevalent in females.[2]
Orbital fat content and overall volume decreases with age or after trauma, producing enophthalmos. Greater spacing between the globe and eyelid creates relative lid laxity.[1][16] Patients with documented lower lid laxity, shorter axial lengths and lower Hertel measurements are associated with entropion,[2][16][17] but no difference exists between entropion patients and normal controls.[18] Enophthalmos also allows for greater orbicularis override, which can drive entropion.[16] Asians and females are more enophthalmic[19] contributing to higher rates of entropion observed in these populations.
Elderly and Asian patients have increased anterior protrusion of orbital fat, which creates a force vector acting on the lower lid that predisposes for entropion.[7][20][21][22]
Symptoms
Patients with entropion tend to present with complaints of foreign body sensation, redness, tearing and discharge. Symptoms may be intermittent depending on etiology.[1] Dry eye syndrome is present in 72.1% patients, and punctate epithelial erosions are noted in 61.9%.[2] In some patients, visual symptoms in down gaze, from absence of synkinetic lower eyelid margin movement may be the presenting feature.
Physical Examination
A patient suspected to have entropion should undergo a thorough ophthalmologic exam. On gross exam, one should note any blepharo or facial spasm, signs of skin irritation or infection and ocular surface disturbance including cicatricial changes. The physician should pay close attention to the lid margin structures to evaluate for associated trichiasis, distichiasis and epiblepahron. These conditions can mimic entropion but do not have improper position of the eyelid margin and have different management.
One should examine the cornea with fluorescein for abrasions, corneal scarring or thinning, and neovascularization of the cornea.[1] Careful examination of the conjunctiva is important, as partial lid entropion of the lateral or medial lid may not affect the cornea. The examiner should make note of symblepharon, forniceal shortening, and margin abnormalities if present, as these findings may indicate an inflammatory process.[1][23] Additionally, histologic studies have shown chronic mechanical injury can induce chronic inflammation that can lead to squamous metaplasia of the conjunctiva. [8][24]
Special Tests
Horizontal lid laxity can be evaluated with the snap back test. The examiner pulls the lower lid down and observes the lid returning to its original position without allowing the patient to blink. Normally, the lid returns promptly without a blink, but in cases of increased laxity, a blink may be needed to reestablish proper position. The examiner can also pull the lower lid anteriorly away from the globe. In involutional entropion, the lower lid can be displaced 6-15mm from the globe, compared to only 2-3mm in a normal lid occasionally even up to the inferior orbital rim.[23][25]
Resistance to traction and persistence of entropion with horizontal lid traction can indicate cicatricial component. Eyelid eversion tends to be difficult in cicatricial patients, but is usually easy to achieve in involutional cases.[1]
Lower lid retractor function is evaluated by measuring lower lid excursion in downgaze. Normally, lower lid retractors supply 3-4mm inferior movement of the lower lid margin then the patient moves from primary position to downgaze. If this is absent or decreased, it may be a sign of lower lid retractor weakness, dehiscence or disinsertion. In some cases of lower lid retractor disinsertion, slit lamp examination of the inferior fornix reveals a white line 3-4 mm inferior to the inferior tarsal border representing the disinserted retractor band.[1][23] Increased distance between the lower lid retractors and inferior tarsal plate is often present in entropion.[5]
Spastic entropion can be elicited by forcefully closing the eyelids, causing override of the pretarsal orbicularis oculi by the preseptal orbicularis. Faria-e-Sousa described a method to induce override. After application of topical anesthetic, the patient is instructed to look down. The central lower eyelid is pinched, and skin is rolled over the superior tarsal border and pressed against the globe. The eyelid skin is then spread against the globe and released. The patient remains in downgaze for the entire test. If the entropion persists with eye movements and blinking for at least 3 minutes, a diagnosis of spastic or intermittent entropion can be made.[25]
Differential Diagnosis
Trichiasis
Trichiasis is a condition in which eyelashes grow in a posterior direction toward the corneal surface. It can present similar to entropion, but management is different, as the problem is the direction of lash growth and not a margin malposition.[26]
Distichiasis
Another diagnosis that can be confused with entropion is distichiasis. Distichiasis is the growth of lashes from the meibomian gland orifices, which can irritate and damage the cornea.[1]
Epiblepharon
Epiblepharon is a horizontal fold of redundant skin and orbicularis at the eyelid margin causing the lashes to be directed vertically or invert to a small degree. This condition is common in Asian populations and is present in 46-52.5% of Asian children less than a year old.(Kim) This condition usually asymptomatic and resolves with age, but in extreme and persistent cases surgical management may be indicated if corneal injury is imminent.[23]
Types
There are four main categories of entropion, each with a different pathophysiology: involutional, spastic, cicatricial and congenital. Treatments are aimed specifically at the particular causes for the condition.
Involutional Entropion
Involutional entropion is the most common type of entropion. Management should be directed at the specific mechanical failures of horizontal and vertical lid laxity, lower lid retractor weakness, and orbicularis oculi override. Addressing more contributing factors has a greater chance at achieving resolution.[23]
Management strategies range from conservative, noninvasive measures to more complex surgeries requiring tissue grafts. The approach depends on disease severity, patient comorbidities and goals of care. Numerous repair techniques are described in the literature, each with a slightly different approach to the mechanical issues underlying involutional entropion and various combinations of the strategies discussed below.[27][28][29][30][31][32][33][34][35][36][37][38]
Noninvasive Treatment
Patients can achieve temporary relief with taping of the lower lid to the malar eminence[39] or with application of a cyanoacrylate liquid bandage to evert the lid margin.[4] These treatments are beneficial as temporizing measures until the patient can have surgery for definitive repair, or if the patient is too ill to be a candidate for surgical intervention. Temporary relief from involutional entropion can also be achieved with botulinum toxin injections to the preseptal orbicularis, to combat override.[40]
Carbon dioxide laser skin resurfacing has been proposed as a conservative means of managing involutional entropion. This method was described with success in four of five patients followed for 21 months.[41]
Surgical Treatment
General principles of management include either addressing one of the factors alone or whenever possible addressing the 2 main causative factors : lower eyelid laxity and reattachment of lower eyelid retractors. In the elderly and debilitated patients, minimally invasive and brief procedures may be attempted first albeit with reduced success rates.
Rotational or everting Sutures
Full-thickness eyelid sutures (Quickert sutures) can be placed at the bedside or in the office as a quick procedure to offer patients immediate relief from entropion symptoms.[29] The procedure takes an average of 15 minutes to complete and requires only local anesthesia.[42] A double-armed 4-0 chromic or vicryl sutures are placed from the deep inferior fornix below the inferior tarsal border, through the lower lid retractors, and exits through the skin superior to the level of insertion. Exiting more superiorly causes more lid eversion. This procedure indirectly tightens the lower lid retractors and forms scarring between the retractors, orbicularis and skin to prevent override.[1] Recurrence is common, with Jand et al observing over 21% recurrence at 6 months and nearly 50% by two years.[43] Tsang et al encountered better results with 33% recurrence at 14-40 months.[42]
Horizontal lid tightening
This may be performed by traditional procedures through a lateral canthototmy, eg, lateral Tarsal Strip or through canthotomy sparing procedures such as the Modified suture canthoplasty/pexy with or without lateral canthal tendon release through the upper eyelid crease incision.
Lateral Tarsal Strip
Horizontal lid laxity can be addressed surgically with a tarsal strip. A lateral canthotomy and inferior cantholysis is performed to release the lower lid. The mucocutaneous junction is removed from the lid margin, and the anterior lamella is excised off the tarsus. Conjunctiva is debrided from the posterior tarsus. A horizontal incision through the superior tarsal plate creates a strip that is trimmed to achieve the desired amount of tightening. The strip is attached to the internal aspect of the lateral orbital rim.[44]
A small case series of 15 patients treated with tarsal strip only showed no recurrence of entropion at an average of 13 months follow-up.[45] A series of 42 eyelids with involutional entropion without canthal tendon laxity used full-thickness excision and repair to treat entropion. This study reported 8% recurrence at 14 months, with average time to failure of 13 months.[38] As an independent measure, addressing the horizontal dimension of the lower lid is more successful in correcting entropion than targeting lid rotation.
There is only one randomized control trial comparing entropion repair techniques,[44][46] examining everting sutures against everting sutures with tarsal strip. This study found 21% recurrence by 18 months with only everting sutures and no recurrences in the combined group.[44]
Modified Suture Canthoplasty
An lateral upper eyelid incision may be employed to gain access to the superotemporal orbital rim and overlying periosteum. The Lateral canthal tendon may be released based on the degree of laxity and tightening desired. A lateral lower eyelid margin suture (4-0 Maxon) may be placed through a scratch incision with the double armed suture engaging the lateral tarsus, lateral canthal tendon which is then anchored to the superotemporal orbital periosteum. The upper eyelid wound is then closed.
Lower Lid Retractor Reinsertion
Lower lid retractor disinsertion can be reversed surgically with posterior advancement of the retractors. This may be performed through the posterior (transconjunctival) or anterior (transcutaneous) approach. These may be performed with or without a lateral canthotomy.
Transconjuncitval approach: An incision is made through the conjunctiva and lower lid retractors spanning from the lateral canthus to just lateral to the inferior punctum, taking advantage of the bloodless plane just below the inferior tarsal border. The conjunctiva and retractors are then separated from the anterior lamella to expose the orbital septum overlying orbital fat.
Transcutaneous approach: More easily a subciliary incision with dissection below the pretarsal orbicularis oculi exposes the orbital septum. Once this layer is opened up , the preaponeurotic fat of the lower eyelid helps identify the lower eyelid retractors, aided by the patient being asked to look up and down.The lower lid retractor which is immediately posterior to the fat compartments and adherent to the conjunctiva is identified with the patient asked to look up and down.
Regardless of approach above, a strip of orbicularis may be excised or ablated inferior to the tarsus, to reduce the preseptal orbicularis override. The retractors may be separated from the conjunctiva with cautery, and sharp dissection allows for exposure of the anterior surface of the inferior tarsal plate.[23] A single or multiple 6-0 vicryl sutures are then used to reattache the lower eyelid retractor to the anterior inferior tarsus to evert the lid margin.
Combining tarsal strip with retractor advancement takes an average of 13 minutes more than retractor advancement alone,[47] and gives a 96.7% success rate.[48] The dual procedure is more effective in treating involutional entropion with horizontal lid laxity than retractor advancement alone.[47] External approach can be used if there is absent lid laxity, significant festoons or prominent lower lid dermatochalasis.[23]
Everting sutures can also be placed along with tarsal strip and retractor reinsertion with recurrence rate of 2.2% at 22.6 months, much less than the rate of 29% for everting sutures alone.[49]
Spastic Entropion
Spastic entropion is thought by some to be a subset of involutional entropion[1] often intermittent, and may be a precursor to persistent lower eyelid malposition. Muscle spasm of the orbicularis can induced by local irritation, infection or recent ocular surgery can unmask asymptomatic involutional changes resulting in intermittent entropion.[25]
Treatment
First line treatment is to relieve the instigating condition by treating underlying condition.[25] Hubbard and Kanski in 1973 described injecting 80% alcohol into the orbicularis oculi to quell spasm with high rates of success.[50] Presently, botulinum toxin injection to the orbicularis and full thickness eyelid sutures have been used to treat this entity.[51]
Cicatricial Entropion


Cicatricial entropion results from chronic inflammation leading to fibrosis, scarring and shortening of the posterior lamella. These cases are associated with other stigmata of chronic inflammation such as symblepharon, forniceal shortening, keratinization, and loss of normal margin structures. This is unique from other causes of entropion because it is usually secondary to a systemic and progressive inflammatory condition such as ocular cicatricial pemphigoid, Stevens-Johnson syndrome, trachoma, and herpetic disease.[1][23] An early form of cicatricial entropion is Meibomian Gland Inversion(MGI) commonly encountered in chronic meibomitis or aggressive electroepilation with scarring of the posteior lamella.
Cicatricial entropion may also be the result of trauma and can be iatrogenic from surgery or radiation therapy.[23][52][53][54] It has also been noted following chronic antiglaucoma medications, especially miotic agents, prostaglandin analogues and some chemotherapy drugs.[52][54][55]
Due to its progressive nature and difficulty in managing the underlying condition, cicatricial entropion is considered the most difficult type of entropion to treat.[1] Recurrence rate following surgery ranges from 12-71% regardless of technique used, with higher rates in more severe cases.(Wu)[53][56][57][58][59][60]
Treatment
Treatment of cicatricial entropion should always include medical control of the underlying pathologic condition when present. Surgical technique depends on the severity of disease and etiology of symptoms.[23]
If there is mild disease with symptoms from lashes abrading the corneal surface, skin resection may be sufficient to rotate the margin. If offending lashes are arranged in a sectoral pattern, eyelid margin splitting with lash root, cryotherapy may be considered.[23] Lash follicle excision can also be considered for segmental lash malpositions. Follicle excision is achieved by splitting the lamella posterior to the lashes and excising the lashes with sharp Westcott scissors. The base of the lash follicles may be cauterized to prevent regrowth.[23] Functional success of 90% has been demonstrated with no return of trichiasis at 6-24 months.[60]
In moderate disease affecting the upper lids, tarsal fracture is a viable surgical option that preserves the lashes with acceptable cosmesis. An external partial tarsectomy is performed through a lid crease incision. A double-armed 6-0 vicryl is placed partial thickness through the tarsus and externalized. A full-thickness tarsotomy is then performed to direct the lid margin away from the globe. Everting sutures are placed to keep the lid margin rotated anteriorly, and the skin is closed.[23]
Transverse blepharotomy and marginal rotation has also been used to treat cicatricial entropion. In this procedure a full-thickness incision is made 4mm from the lid margin and 5-0 absorbable suture is passed partial-thickness through the anterior tarsus and lower lid retractors of the proximal lid and then through the orbicularis and skin of the distal lid. The suture is tied in horizontal mattress fashion over a bolster near the lash line, and skin is closed. The sutures and bolster remain in place for 10 days. This procedure has an 85% success rate for upper and lower lid cicatricial entropion repair.[54]
For severe cicatricial disease, the posterior lamella must be lengthened while releasing scar tissue and lid retractors. In these instances the posterior lid retractors can be weakened by recession or lysis with a spacer.[61] Hard palate graft, other mucous membrane graft or allograft can be used to support and bolster the posterior lamella. Graft choice is especially important when operating on the upper lid, as the graft will be in constant contact with the cornea. Free tarsoconjunctival grafts may provide good results.[23]
Lamellar splitting procedures
Lamellar splitting procedures involve separation of skin and orbicularis oculi muscle from tarsus/conjunctiva and recessing/repositioning the anterior lamella with or without posterior lamella advancement. This principle is particularly beneficial in conditions where operating on the tarsoconjunctiva may trigger conjunctival inflammation and additional cicatrization.[62]

Anterior lamellar recession (ALR)
ALR entails complete splitting of the eyelid with subsequent recession of anterior lamella several millimeters away from the lid margin. Interlamellar separation can be performed through an eyelid crease [63] or a lid margin approach.[64] Complete lamellar separation allows the anterior lamella to be recessed on the posterior lamella without tension. This gives a potentially long lasting correction . The bare tarsal margin can be left to granulate spontaneously or covered with a graft such as buccal mucous membrane[65] or amniotic membrane.
Anterior lamellar repositioning
ALR should be differentiated from anterior lamellar repositioning that does not entail complete lamellar division. This procedure should be reserved for mild cases only such as marginal entropion or meibomian gland inversion.[66]
Anterior lamellar repositioning with partial lid margin split
Concurrent lid margin split helps augment lid margin eversion.

The five-step procedure
Diab and Allen [67]described a five-step approach for treating recurrent entropion. The described technique helps restore the lamellar balance and address the pathophysiological changes in the diseased eyelid . The 5 steps include ; 1- Small blepharoplasty which helps lessen skin redundancy , 2- Complete lamellar splitting with meticulous dissection at the lid margin, peeling the entire anterior lid margin, 3- Upper lid retractor disinsertion from the tarsus with dissection free of the conjunctiva for at least 5 mm, allowing posterior lamellar advancement and correction of any coexisting lid retraction and lagophthalmos, 4- Anterior lamellar recession for at least 3 mm on the advanced posterior lamella. Complete anterior lamellar separation as a bipedicle flap helps unrestrained upward repositioning, 5- Lid crease incision closure including bites through the edge of levator aponeurosis- Muller’s muscle flap. This technique redirects the pull of the upper eyelid retractors from the tarsal plate to the recessed anterior lamella. This has a dual effect; first, it maintains an upward vector of traction on the anterior lamella with effective lash eversion preventing downward migration of the anterior lamella during healing. Second, it allows free advancement of the posterior lamella inferiorly compensating for the shortened tarsoconjunctiva.
Congenital Entropion

Congenital entropion is a rare condition in which the lower lid margin is rotated inward since birth. This results from disinserted lower lid retractors, posterior lamella vertical insufficiency or kinking of the tarsal plate.[23] Children may also develop entropion following facial paralysis, a condition that typically leads to ectropion in adults. In pediatric patients, the orbicularis acts to counter the inturning force of the lower lid retractors, and facial paralysis results in unchecked retractor function rotating the eyelid margin toward the globe surface.[68] Eyelid retraction may be confused with congenital entropion.[69]
Treatment
Treatment include lubrication to limit mechanical trauma, taping the lower lid to the malar prominence, or injecting low doses of botulinum toxin into the orbicularis to weaken the muscle and prevent override. Surgical therapy provides definitive treatment.[40][69][70]
Complications
The most common complication following entropion repair especially cicatricial entropion[54][60], is recurrence. Transconjunctival involutional entropion repair has a recurrence of 3.3%.[48] While involutional entropion should be optimally corrected, recurrence in cicatrial entropion may be minimized by aiming for mild overcorrection. Excessive overcorrection may result in an ectropion however. Ectropion can also result from repairs that attach the inferior lid retractors to the anterior surface of the tarsus rather than the inferior aspect especially when lower eyelid laxity has not been adequately addressed[1]. Overly aggressive shortening of the lower lid retractors or excessive skin removal can produce lower lid retraction and inferior scleral show. Using local anesthesia allows the surgeon to assess lid height, motility and contour during the procedure and make any necessary adjustments promptly to prevent induction of ectropion.[48]
Lid-splitting surgical approaches risk fistula formation. If encountered, these should be excised and repaired.[1]
The surgeon should be cognizant of the marginal arcade during entropion repair , especially in recurrent cases, to prevent necrosis at the lid margin. Any full-thickness incisions through the lid should be made inferior to the inferior margin of the tarsus, at least 4mm inferior to the lid margin, to avoid vascular compromise.[1]
Overall, transconjunctival entropion repair has a low rate of complications, with Erb et al noting a 4% rate: stitch abscess and conjunctivochalasis 0.7% each and lateral tarsal strip dehiscence and lateral canthal dystopia.[48]
Additional Resources
- American Society of Ophthalmic Plastic and Reconstructive Surgery. Entropion - Eyelids that turn in.
- Eyeplastics.com. Entropion.
- Patient.co.uk. Entropion.
- Medscape. Entropion.
- Turbert D, Ninel Z Gregori. Eyelashes. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/eyelashes-list. Accessed March 12, 2019.
- Eyelid. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/eyelid-5. Accessed March 12, 2019.
- American Academy of Ophthalmology Basic and Clinical Science Course. Section 7. Orbit, Eyelids, and Lacrimal System.
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 Nowinski TS. 2011. Entropion. In: Tse DT, editor. Color Atlas of Oculoplastic Surgery. 2nd ed. Philadelphia (PA): Lippincott Williams & Wilkins. p 44-53.
- ↑ 2.0 2.1 2.2 2.3 Damasceno RW, Osaki MH, Dantas PE, Belfort R Jr. Involutional entropion and ectropion of the lower eyelid: prevalence and associated risk factors in the elderly population. Ophthal Plast Reconstr Surg. 2011 Sep-Oct;27(5):317-20.
- ↑ Wright M, Bell D, Scott C, Leatherbarrow B. Everting suture correction of lower lid involutional entropion. Br J Ophthalmol. 1999 Sep;83(9):1060-3.
- ↑ 4.0 4.1 Osaki T, Osaki MH, Osaki TH. Temporary management of involutional entropion with octyl-2-cyanoacrylate liquid bandage application. Arg Bras Oftalmol. 2010 Mar-Apr;73(2):120-4.
- ↑ 5.0 5.1 Hawes MJ, Dortzbach RK. The microscopic anatomy of the lower eyelid retractors. Arch Ophthalmol. 1982 Aug;100(8):1313-8.
- ↑ Kakizaki H, Zhao J, Nakano T, Asamoto K, Zako M, Iwaki M, Miyaishi O. The lower eyelid retractor consists of definite double layers. Ophthalmology. 2006 Dec;113(12):2346-50.
- ↑ 7.0 7.1 Kakizaki H, Chan WO, Takahashi Y, Selva D. Overriding of the preseptal orbicularis oculi muscle in Caucasian cadavers. Clin Ophthalmol. 2009;3:243-6.
- ↑ 8.0 8.1 8.2 8.3 Kocaoglu FA, Katircioglu YA, Tok OY, Pulat H, Omek F. The histopathology of involutional ectropion and entropion. Can J Ophthalmol. 2009 Dec;44(6):677-9.
- ↑ Montes GS. Structural biology of the fibres of the collagenous and elastic systems. Cell Bio Int. 1996 Jan;20(1):15-27.
- ↑ Kielty CM, Sherratt MJ, Shuttleworth CA. Elastic fibres. J Cell Sci. 2002 Jul 15;115(Pt 14):2817-28.
- ↑ Imayama S, Braverman IM. A hypothetical explanation for the aging of skin. Chronologic alteration of the three-dimensional arrangement of collagen and elastic fibers in connective tissue. Am J Pathol. 1989 May;134(5):1019-25.
- ↑ Varani J, Dame MK, Rittie L, Fligiel SE, Kang S, Fisher GJ, Voorhees JJ. Decreased collagen production in chronologically aged skin: roles of age-dependent alteration in fibroblast function and defective mechanical stimulation. Am J Pathol. 2006 Jun;168(6):1861-8.
- ↑ Stefanyszyn MA, Hidayat AA, Flanagan JC. The histopathology of involutional entropion. Ophthalmology. 1985 Jan;92(1):120-7.
- ↑ 14.0 14.1 Damasceno RW, Osaki MH, Dantas PE, Belfort R Jr. Involutional ectropion and entropion: clinicopathologic correlation between horizontal eyelid laxity and eyelid extracellular matrix. Ophthal Plast Reconstr Surg. 2011 Sep-Oct;27(5):321-6.
- ↑ 15.0 15.1 15.2 Bashour M, Harvey J. Causes of involutional ectropion and entropion - age-related tarsal changes are the key. Ophthal Plast Reconstr Surg. 2000 Mar;16(2):131-41.
- ↑ 16.0 16.1 16.2 Heimmel MR, Enzer YR, Hofmann RJ. Entropion-ectropion: the influence of axial globe projection on lower eyelid malposition. Ophthal Plast Reconstr Surg. 2009 Jan-Feb;25(1)7-9.
- ↑ Jyothi SB, Seddon J, Vize CJ. Entropion-ectropion: the influence of axial globe length on lower eyelid malposition. Ophthal Plast Reconstr Surg. 2012 May-Jun;28(3):199-203.
- ↑ Kersten RC, Hammer BJ, Kulwin DR. The role of enophthalmos in involutional entropion. Ophthal Plast Reconstr Surg. 1997 Sep;13(3):195-8.
- ↑ Tsai CC, Kau HC, Kao SC, Hsu WM. Exophthalmos of patients with Graves' disease in Chinese of Taiwan. Eye. 2006 May;20(5):569-73.
- ↑ Carter SR, Chang J, Aguilar GL, Rathbun JE, Seiff SR. Involutional entropion and ectropion of the Asian lower eyelid. Ophthal Plast Reconstr Surg. 2000 Jan;16(1):45-9.
- ↑ Beigi B. Orbicularis oculi muscle stripping and tarsal fixation for recurrent entropion. Orbit. 2001 Jun;20(2):101-105.
- ↑ Carter SR, Seiff SR, Grant PE, Vigneron DB. The Asian lower eyelid: a comparative anatomic study using high-resolution magnetic resonance imaging. Ophthal Plast Reconstr Surg. 1998 Jul;14(4):227-34.
- ↑ 23.00 23.01 23.02 23.03 23.04 23.05 23.06 23.07 23.08 23.09 23.10 23.11 23.12 23.13 23.14 Iyengar SS, Dresner SC. 2012. Entropion. In: Black EH, Nesi FA, Calvano CJ, Gladstone GJ, Levine MR editors. Smith and Nesi's Ophthalmic Plastic and Reconstructive Surgery. 3rd ed. New York (NY):Springer. p. 311-315.
- ↑ Kim C, Shin YJ, Kim NJ, Khwarg SI, Hwang JM, Wee WR. Conjunctival epithelial changes induced by cilia in patients with epiblepharon or entropion. Am J Ophthallmol. 2007 Oct;144(4):564-9.
- ↑ 25.0 25.1 25.2 25.3 Faria-E-Sousa SJ, de Paula Gomes Vieira M, Silva JV. Uncovering intermittent entropion. Clin Ophthalmol. 2013;7:385-8)
- ↑ Cahill KV, Foster JA. 2012. Trichiasis. In: Black EH, Nesi FA, Calvano CJ, Gladstone GJ, Levine MR editors. Smith and Nesi's Ophthalmic Plastic and Reconstructive Surgery. 3rd ed. New York (NY): Springer. p.317-321.
- ↑ Wies FA. Spastic entropion. Trans Am Acad Ophthalmol Otolaryngol. 1955 Jul-Aug;59(4)503-6.
- ↑ Wheeler JM. Spastic entropion correction by orbicularis transplantation. Trans Am Ophthalmol Soc. 1938;36:157-62.
- ↑ 29.0 29.1 Quickert MH, Rathbun E. Suture repair of entropion. Arch Ophthalmol. 1971 Mar;85(3):304-5.
- ↑ Rainin EA. Senile entropion. Arch Ophthalmol. 1979 May;97(5):928-30.
- ↑ Bick MW. Surgical management of orbital tarsal disparity. Arch Ophthalmol. 1966 Mar;75(3):386-9.
- ↑ Leone CR. Internal tarsus-orbicularis resection for senile spastic entropion. Ann Ophthalmol. 1975 Jul;7(7):1004-6.
- ↑ Jones LT, Reeh MJ, Wobig JL. Senile entropion: a new concept for correction. Am J Ophthalmol. 1972 Aug;74(2):327-9.
- ↑ Carroll RP, Allen SE. Combined procedure for repair of involutional entropion. Ophthal Plast Reconstr Surg. 1991;7(2):123-7.
- ↑ Nowinski TS. Orbicularis oculi muscle extirpation in a combined procedure for involutional entropion. Ophthalmology. 1991 Aug;98(8):1250-6.
- ↑ Dresner SC, Karesh JW. Transconjunctival entropion repair. Arch Ophthalmol. 1993 Aug;111(8):1144-8.
- ↑ Nakauchi K, Mimura O. Combination of a modified Hotz procedure with the Jones procedure decreases the recurrence of involutional entropion. Clin Ophthalmol. 2012;6:1819-22.
- ↑ 38.0 38.1 Roberts MA, Baddeley P, Sinclair N, Lane CM. The lower lid diamond: a simple entropion repair to correct both horizontal and lower-lid retractor laxity. Ophthal Plast Reconstr Surg. 2012 Jan-Feb;28(1):44-6.
- ↑ Stevens S. Tape correction for lower eyelid entropion. Comm Eye Health. 2012;25(78):36.
- ↑ 40.0 40.1 Steel DH, Hoh HB, Harrad RA, Collins CR. Botulinum toxin for the temporary treatment of involutional lower lid entropion: a clinical and morphological study. Eye. 1997;11(Pt 4):472-5.
- ↑ Babuccu O. An alternative approach for involutional entropion: a preliminary study. Lasers Med Sci. 2012 Sep;27(5):1009-12.
- ↑ 42.0 42.1 Tsang S, Yau GS, Lee JW, Chu AT, Yuen CY. Surgical outcome of involutional lower eyelid entropion correction using transcutaneous everting sutures in Chines patients. Int Ophthalmol. 2014 Aug;34(4):865-8.
- ↑ Jang SY, Choi SR, Jang JW, Kim SJ, Choi HS. Long-term surgical outcomes of Quickert sutures for involutional lower eyelid entropion. J Craniomaxillofac Surg. 2014 May 14.
- ↑ 44.0 44.1 44.2 Scheepers MA, Singh R, Ng J, Zuercher D, Gibson A, Bunce C, Fong K, Michaelides M, Olver J. A randomized controlled trial comparing everting sutures and a lateral tarsal strip for involutional entropion. Ophthalmology. 2010 Feb;117(2):352-5.
- ↑ Balaji K, Balaji V, Kummararaj G. The correction of involutional entropion of eyelid by lateral strip procedure. J Surg Tech Case Rep. 2010 Jul;2(2):64-6.
- ↑ Boboridis K, Bunce C. Interventions for involutional lower lid entropion. Cochrane Database Syst Rev. 2002;(1):CD002221.
- ↑ 47.0 47.1 Lee H, Takahashi Y, Ichinose A, Kakizaki H. Comparison of surgical outcomes between simple posterior layer advancement of lower eyelid retractors and combinatin with a lateral tarsal strip procedure for involutional entropion in a Japanese population. Br J Ophthalmol. 2014 May 30.
- ↑ 48.0 48.1 48.2 48.3 Erb MH, Uzcategui N, Dresner SC. Efficacy and complications of the transconjunctival entropion repair for lower eyelid involutional entropion. Ophthalmology. 2006 Dec;113(12):2351-6.
- ↑ Serin D, Buttanri IB, Karslioglu S, Sevim MS, Buttanri B, Akbaba M. The efficacy of the combined procedure in involutional entropion surgery; a comparative study. Korean J Ophthalmol. 2013 Dec;27(6):405-8.
- ↑ Hubbard IH, Kanski JJ. A simple treatment for spastic entropion. Proc R Soc Med. 1973 Feb;66(2):173-4.
- ↑ Winterhoff J, Köhler S, Laskawi R. Botulinum toxin for the treatment of spastic entropion. Case report. HNO. 2013 Jul;61(7):665-7.
- ↑ 52.0 52.1 Hatton MP, Raizman M, Foster CS. Exacerbation of undiagnosed ocular cicatricial pemphigoid after repair of involutional entropion. Ophthal Plast Reconstr Surg. 2008 Mar-Apr;24(2):165-6.
- ↑ 53.0 53.1 Milliman AL, Katzen LB, Putterman AM. Cicatricial entropion: an analysis of its treatment with transverse blepharotomy and marginal rotation. Ophthalmic Surg. 1989 Aug;20(8):575-9.
- ↑ 54.0 54.1 54.2 54.3 Bleyen I, Dolman PJ. The Weis procedure for management of trichiasis or cicatricial entropion of either upper or lower eyelids. Br J Ophthalmol. 2009 Dec;93(12):1612-5.
- ↑ Cetinkaya A, Hudak D, Kulwin D. Cicatricial entropion following docetaxel (Taxotere) therapy. Ophthal Plast Reconstr Surg. 2011 Sep-Oct;27(5):e113-6.
- ↑ Sodhi PK, Yadava U, Pandey RM, Mehta DK. Modified grey line split with anterior lamellar repositioning for treatment of cicatricial lid entropion. Ophthalmic Surg Lasers. 2002 Mar-Apr;33(2):169-74.
- ↑ Sodhi PK, Yadava U, Mehta DK. Efficacy of lamellar division for correcting cicatricial lid entropion and its associated features unrectified by the tarsal fracture technique. Orbit. 2002 Mar;21(1):9-17.
- ↑ Cheung D, Sandramouli S. Consecutive ectropion after the Wies procedure. Ophthal Plast Reconstr Surg. 2004 Jan;20(1):64-8.
- ↑ Yorston D, Mabey D, Hatt S, Burton M. Interventions for trachoma trichiasis. Cochrance Database Syst Rev. 2006 Jul 19;(3):CD004008.
- ↑ 60.0 60.1 60.2 Wu AY, Thakker MM, Wladis EJ, Weinberg DA. Eyelash resection procedure for severe, recurrent, or segmental cicatricial entropion. Ophthal Plast Reconstr Surg. 2010 Mar-Apr;26(2):112-6.
- ↑ Kakizaki H, Malhotra R, Madge SN, Selva D. Lower eyelid anatomy: an update. Ann Plast Surg. 2009 Sep;63(3):344-51.
- ↑ Diab MM, Allen RC, Gawdat TI, Saif AS. Trachoma elimination, approaching 2020. Curr Opin Ophthalmol. 2018;29(5):451-457. doi:10.1097/ICU.0000000000000504
- ↑ Gawdat TI, Kamal MA, Saif AS, Diab MM. Anterior lamellar recession for management of upper eyelid cicatricial entropion and associated eyelid abnormalities. Int J Ophthalmol 2017; 10:1830–1834.
- ↑ Pandey N, Jayaprakasam A, Feldman I, Malhotra R. Upper eyelid levator-recession and anterior lamella repositioning through the grey-line: Avoiding a skin-crease incision. Indian J Ophthalmol. 2018;66(2):273-277. doi:10.4103/ijo.IJO_774_17
- ↑ Singh S, Narang P, Mittal V. Labial mucosa grafting for lid margin, anterior lamellar, and posterior lamellar correction in recurrent cicatricial entropion. Orbit. 2021;40(4):301-305. doi:10.1080/01676830.2020.1782439
- ↑ Samia-Aly E, Barua AR, Patel RP, Mehta P. Anterior Lamellar Repositioning in the Management of Meibomian Gland Inversion Secondary to Meibomian Gland Dysfunction. Ophthalmic Plast Reconstr Surg. 2021;37(6):560-563. doi:10.1097/IOP.0000000000001948
- ↑ Diab MM, Allen RC. Recurrent upper eyelid trachomatous entropion repair: long-term efficacy of a five-step approach. Eye (Lond). 2021;35(10):2781-2786. doi:10.1038/s41433-020-01306-y
- ↑ Pasco NY, Kikkawa DO, Korn BS, Punja KG, Jones MC. Facial nerve paralysis: an unrecognized cause of lower eyelid entropion in the pediatric population. Ophthal Plast Reconstr Surg. 2007 Mar-Apr;23(2):126-9.
- ↑ 69.0 69.1 Maman DY, Taub PJ. Congenital entropion. Ann Plast Surg. 2011 Apr;66(4):351-3.
- ↑ Christiansen G, Mohney BG, Baratz KH, Bradley EA. Botulinum toxin for the treatment of congenital entropion. Am J Ophthalmol. 2004 Jul;138(1):153-5.