Merkel Cell Carcinoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Overview
Merkel cell carcinoma of the eyelid is a rare, highly malignant neuroendocrine tumor. These tumors originate from sensory Merkel cells, first discovered by Friedrich Merkel in 1875 and found to be associated with light touch and the discrimination of shapes and textures. Merkel cell carcinomas have a predilection for the head and neck area (50% of cases), with 5-10% of lesions occurring on the eyelids. The annual incidence is 0.23 cases per 100,000 persons and has increased significantly in the last few decades, likely secondary to an aging population, increasing number of patients with immunosuppression and enhanced diagnostic techniques.[2]
Risk Factors
- Age > 50
- Immunosuppression (e.g. transplant recipients, lymphoproliferative malignancies, HIV)
- History of sun (UV radiation) exposure
- Caucasian ethnicity[3]
- Polyomavirus (80% of MCC are positive for polyomavirus)[4]
Diagnosis
Physical examination
A complete physical exam should be performed including comprehensive ophthalmic exam to assess the extent of the disease and evaluate for any additional suspicious cutaneous lesions. Palpation of the preauricular and cervical lymph nodes is important to assess for possible lymphatic spread. If there is any evidence of lymphadenopathy or the disease appears to be diffusely involving the eyelid, additional imaging is required to evaluate for systemic spread of the disease. At the time of diagnosis, up to 37% of patients have at least one affected node and 6-12% of patients already have metastatic disease.[5]
Signs and Symptoms
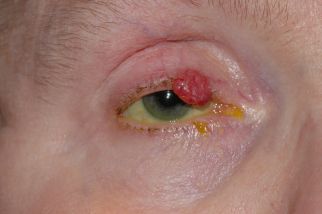
Merkel cell carcinomas often present as a painless solitary nodule with a "violaceous" (purple-red) hue, as seen in Figures 1-3. Occasionally, the tumor may ulcerate and satellite lesions can develop. Heath et al proposed the mnemonic "AEIOU" for assistance with MCC diagnostic clarity: asymptomatic (lack of tenderness), expanding rapidly, immunosuppression, older than 50 years, and UV-exposed site. In their study, 89% of the patients diagnosed with MCC met three or more criteria, 52% of the patients met four or more criteria, and 7% of the patients met all five criteria.[6]
When involving the periocular area, MCC is most commonly located on the upper eyelid, near the eyelid margin. Unlike most benign entities, MCC (and other malignant lesions) often causes partial or complete madarosis (loss of eyelashes), as well as overlying telangiectatic vessels (Fig 1-3).
Diagnostic procedures
Following a thorough skin and lymph node examination, guidelines from the National Comprehensive Cancer Network (NCCN) recommend biopsy for histopathological and immunohistochemical analysis. The skin biopsy may be accompanied by sentinel lymph node biopsy (SLNB) for patients without clinically positive lymph node, fine needle aspiration or lymph node biopsy for patients with clinically positive lymph nodes, and various imaging exams. After the biopsy is performed, samples can be sent for detection of polyomavirus which can help aid in the diagnosis.
Differential diagnosis
The differential diagnosis includes benign skin lesions such as chalazion, lipoma, dermatofibroma, cysts, or vascular lesions, as well as other malignancies, including basal cell carcinoma, squamous cell carcinoma, or sebaceous carcinoma. Unfortunately, many patients with MCC are initially misdiagnosed as having one of the above benign pathologies and only biopsied once rapid growth over the course of weeks to months is noted, contributing to an often significant delay in time to proper diagnosis. One of the most challenging diagnoses to distinguish from MCC is cutaneous metastases from other cancers, especially metastatic small-cell lung cancer given similar morphological features.[3]
General Pathology
Lesions tend to have large subepidermal nests of cells with scant cytoplasm, as well as large round or oval-shaped nuclei with finely dispersed chromatin, a vesicular appearance and numerous mitotic figures. Additional immunohistochemical staining and electron microscopy can be of great value in distinguishing MCC from alternate entities such as sebaceous cell carcinoma or metastatic small-cell lung cancer. Merkel cell carcinoma express cytokeratin polypeptides 8, 18, and 19, which are characteristic of epithelia. It also exhibits a distinct marker profile with dot like co-expression of pancytokeratin with cytokeratin 20. It stains positively for neuron specific enolase and negatively for S-100 protein. Electron microscopy demonstrates dense-core cytoplasmic granules.
Management
Management consists mainly of surgical excision and pathologic nodal staging. Mohs micrographic surgery or frozen sections are used for histopathologic confirmation of disease free margins. For other areas of the body, suggested margins are 1-2 cm, an area that is often not practical for periocular lesions. Rather, for eyelid Merkel cell carcinomas, a more conservative approach with surgical margins as small as 5 mm is acceptable, although the exact recommended margins remain controversial and vary based on patient and tumor characteristics.[7] Sentinel lymph node biopsy may also allow for detecting metastases that spread through the lymphatic system and aid in staging.
NCCN guidelines recommend adjunctive radiotherapy for all stages of MCC, ideally within 4-6 weeks of surgical excision. Data regarding survival benefit with the use of post-op adjuvant radiation vs surgical excision alone is conflicting; however, most studies agree that adjuvant radiotherapy significantly lowers 5-year risk of local recurrence compared to surgery alone. [8][9][10][11] Radiotherapy can also be considered for primary treatment in patients who are not adequate surgical candidates.
The role of systemic chemotherapy remains more controversial, mostly providing utility in patients not deemed appropriate surgical candidates or those with inoperable disease. Although MCC is considered a chemosensitive tumor and treatment regimens of platinum with etoposide or taxanes and anthracyclines are initially effective, only a short duration of response with no survival benefit has been demonstrated.[3]
The PD-1 (programmed cell death 1) and PD-L1 (programmed cell death protein ligand 1) system, involved in controlling T-cell activation, is a target of new biologic treatment options being studied for the treatment of MCC, including avelumab (anti-PD-L1 antibody), pembrolizumab (anti-PD-1 monoclonal antibody), and nivolumab (anti-PD-1 antibody).
Prognosis
The prognosis of Merkel cell carcinoma is highly-dependent on the extent of disease at that time of diagnosis. Unfortunately, the estimated 3-year mortality rate for all patients with MCC is around 33%, higher than that of even melanoma (approximately 15%). [12] A review of 255 MCC patients found a 97% 5-year survival rate in pathologically node negative patients, dropping to 52% with patients with pathologically positive nodes.[13] If distant metastases are present at the time of diagnosis, expected survival is <10% at three years.[12] Again, early biopsy for suspicious lesions and prompt diagnosis is of utmost importance to maximize ocular and oncologic outcomes for patients with MCC.
References
- ↑ American Academy of Ophthalmology. Merkel cell carcinoma. https://www.aao.org/education/image/merkel-cell-carcinoma-5 Accessed June 3, 2024.
- ↑ Heath M, Jaimes N, Lemos B, Mostaghimi A, Wang LC, Peñas PF, Nghiem P. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008 Mar;58(3):375-81. doi: 10.1016/j.jaad.2007.11.020.
- ↑ Jump up to: 3.0 3.1 3.2 Siqueira SOM, Campos-do-Carmo G, Dos Santos ALS, Martins C, de Melo AC. Merkel cell carcinoma: epidemiology, clinical features, diagnosis and treatment of a rare disease. An Bras Dermatol. 2023 May-Jun;98(3):277-286. doi: 10.1016/j.abd.2022.09.003.
- ↑ Feng H., Shuda M., Chang Y., Moore P.S. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008;319:1096–1100.
- ↑ Schadendorf D., Lebbé C., Hausen A.Z., Avril M.F., Hariharan S., Bharmal M., et al. Merkel cell carcinoma: Epidemiology, prognosis, therapy and unmet medical needs. Eur J Cancer. 2017;71:53–69.
- ↑ Heath M., Jaimes N., Lemos B., Mostaghimi A., Wang L.C., Peñas P.F., et al. Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol. 2008;58:375–381.
- ↑ Merritt H, Sniegowski MC, Esmaeli B. Merkel cell carcinoma of the eyelid and periocular region. Cancers (Basel). 2014 May 9;6(2):1128-37. doi: 10.3390/cancers6021128.
- ↑ Mojica P., Smith D., Ellenhorn J.D.I. Adjuvant radiation therapy is associated with improved survival in Merkel cell carcinoma of the skin. J Clin Oncol. 2007;25:1043–1047.
- ↑ Chen M.M., Roman S.A., Sosa J.A., Judson B.L. The role of adjuvant therapy in the management of head and neck Merkel cell carcinoma: an analysis of 4815 patients. JAMA Otolaryngol Head Neck Surg. 2015;141:137–141.
- ↑ Takagishi S.R., Marx T.E., Lewis C., Tarabadkar E.S., Juhlin I.D., Blom A., et al. Postoperative radiation therapy is associated with a reduced risk of local recurrence among low risk Merkel cell carcinomas of the head and neck. Adv Radiat Oncol. 2016;1:244–251.
- ↑ Jouary T., Leyral C., Dreno B., Doussau A., Sassolas B., Beylot-Barry M., et al. Adjuvant prophylactic regional radiotherapy versus observation in stage I Merkel cell carcinoma: a multicentric prospective randomized study. Annals of Oncology. 2012;23:1074–1080.
- ↑ Jump up to: 12.0 12.1 Allen PJ, Bowne WB, Jaques DP, Brennan MF, Busam K, Coit DG. Merkel cell carcinoma: prognosis and treatment of patients from a single institution. J Clin Oncol. 2005;23(10):2300–9
- ↑ Agelli M, Clegg LX. Epidemiology of primary Merkel cell carcinoma in the United States. J Am Acad Dermatol. 2003;49(5):832–41.