Eyelid Reconstruction
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
The eyelids play an important role in protecting the globe. They form a barrier for the eyes against trauma, excessive light, and help in maintaining the tear-corneal film and also aid in pumping the tears toward the nasolacrimal duct system. Another important aspect is the beauty and expression of the face that is provided by the muscles in the lid. Defects in the eyelids can occur from surgical resection of tumors, traumatic injuries or congenital anomalies. To undertake reconstruction of the eyelids, it is very important to have knowledge of the basic anatomical features of the eyelid, so as to restore it as close as possible to the presurgical parameters and allow adequate functioning.
Anatomy
Eyelids have a complex anatomy. They comprise an array of skin, muscles, nerves, and blood vessels.
The normal eye has an elliptical shape with its horizontal palpebral fissure measuring 28–30 mm and vertical palpebral fissure measuring 10–11 mm at its widest points. The highest point of upper lid is just medial to the pupil in primary gaze and the lowest point of lower lid being just lateral to the pupil. The lateral canthus is approximately 2 mm higher than the medial canthus. [1]
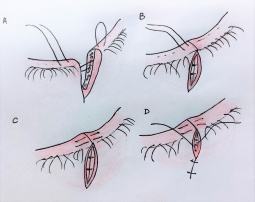
The eyelids are conveniently divided into two anatomical lamellae, the anterior (skin and orbicularis muscle) and the posterior lamellae (tarsal plate and the conjunctiva). A grey line is visible transversely along the middle of each lid margin which marks the junction of these two lamellae. Just posterior to the grey line lies the mucocutaneous junction, at the Meibomian gland openings. The posterior edge of the lid margin is sharper compared to the anterior edge which is rounded.(Figure 1)
Skin
The skin of the eyelid is the thinnest in the body due to an attenuated dermis and very few adnexal structures or sebaceous glands. This limits options for skin graft donor sites, and it's best to match eyelid skin with eyelid skin whenever possible.
Orbicularis oculi
The orbicularis oculi muscle serves as the main protractor of the eyelid. It is innervated by cranial nerve 7, and is divided into orbital (helps in voluntary forced lid closure) and palpebral component (helps in involuntary closure). The orbital portion arises from the medial canthal tendon and laterally inserts into the zygoma. The palpebral portion is subdivided into pretarsal and preseptal components. The pretarsal orbicularis is adherent to the anterior surface of the tarsal plate and attaches medially to the anterior and posterior lacrimal crests. It surrounds the lacrimal sac and aids in the lacrimal pump mechanism. The preseptal orbicularis overlies the orbital septum originating medially from the anterior limb of the medial canthal tendon and from the posterior lacrimal crest. Laterally both condense to form the lateral canthal tendon and inserts on Whitnall’s tubercle.[2][3][4]
Tarsal Plate
The tarsal plate is composed of dense fibrous tissue and form the cytoskeleton of the lids. It is 28–29 mm long and 1 mm thick. The tarsus is 10 mm in height in the upper lid and 3.5 – 5mm in the lower lid, narrowing medially and laterally. These are hinged to the orbital rim by the medial and lateral canthal tendons.
Medial and lateral canthal tendon
The medial canthal tendon (MCT) has an anterior and a posterior limb. The anterior limb inserts anterosuperiorly into the anterior lacrimal crest, while the posterior limb along with the deep head of the pretarsal orbicularis muscle inserts into the posterior lacrimal crest. Similarly the lateral canthal tendon (LCT) has an anterior component that inserts into the orbital rim, while the deeper component passes laterally deep into the orbital septum to insert into the inner side of the lateral orbital rim.
Levator palpebrae superioris
The levator palpebrae superioris elevates the upper eyelid. It arises at the orbital apex from the annulus of Zinn. The muscular portion is approximately 40 mm long and the aponeurosis is 14-20 mm in length. The muscle courses horizontally along the roof of the orbit to end vertically in an aponeurosis which inserts into the anterior surface of the tarsal plate. A few fibers insert into the skin, to help form the lid crease. The capsulopalpebral fascia is analogous to the levator aponeurosis in the lower lid and originates from the inferior rectus muscle encircling the inferior oblique muscle.
Blood and lymphatic supply
The upper lid is supplied by anastomosis of the superior branch of the medial palpebral artery, which is a branch of the ophthalmic artery, and superior branch of the lateral palpebral artery, which is a branch of the lacrimal artery. It has two arcades. The marginal one lies on the anterior tarsal surface, 2–3 mm from the lid margin, and a peripheral arcade on the anterior surface of the Muller's muscle, just above the superior tarsal border. The lower eyelid is supplied by the inferior palpebral artery, a branch from the ophthalmic artery and inferior branch of the lacrimal artery. It also receives a branch of the maxillary artery.
Most of the upper lid and the lateral half of the lower lid drains into the preauricular lymph node while the medial portion of the upper lid and the medial half of the lower lid drain into the submandibular nodes along the lymphatics which follow the angular and facial vessels.
Indications of eyelid reconstruction
- Congenital
- Colobomas isolated or associated with Goldenhar syndrome, Treacher Collins syndrome, Fraser syndrome
- Acquired
- Post-surgical (e.g. resection of tumor, floppy eyelid repair)
- Trauma
- Burns
- Irradiation
- Following previous complicated surgery
Evaluation of eyelid defect
A proper pre-operative assessment and surgical planning takes one already half way through the surgery. So we need to know: -
- If the defect is full-thickness with eyelid margin involving or just an anterior lamellar defect
- Size of defect - amount of lamella loss
- Location – medial, lateral or central
- Medial or lateral canthus involvement
- Lacrimal drainage system involvement
- Age of the patient - laxity of lids
- Condition of the opposite eyelid
- Contralateral eyelid evaluation
- Mobility of surrounding tissues
General consideration for lid reconstruction
Mustarde writes, “When the eye is still present, reconstruction of an eyelid or even a part of it requires a minimum of three elements: an outer layer of skin; an inner layer of mucosa; and a semirigid skeleton interposed between them.”
The goals are to provide adequate eye closure, preservation of tear film, maintenance of an unobstructed visual field, and to recreate an eye which is aesthetically appealing.
- Both the lamellae needs to be replaced, skin – muscle lamina anteriorly and cartilagenous framework and smooth mucous lining posteriorly.
- In general, one of these two lamellae need to be reconstructed as a flap and the other lamella can then be replaced with a free graft/flap. Flaps help in providing vascular supply. However, there have been attempts to reconstruct the whole lower eyelid with a single thick flap.[5][6]
- The levator palpebrae superioris, orbicularis oculi, and inferior retractors must be respected.
- A Stable mucocutaneous lid margin with good apposition to globe should be achieved.
- Scars are hidden if incisions are made in, or parallel to, skin creases (relaxed skin tension lines)[7] .These are present at right angles to the direction of action of the underlying muscle group. Curved scars are less conspicuous than straight scars. The upper lid crease is to be used for most skin incisions involving the upper eyelid.[8]
- Aim should be to achieve symmetry between the two eyes for better cosmesis.
- Direct tension horizontally and minimize vertical tension. [4]
- Avoid overlapping of wound edges, ensure everted wound margins (Figure 3) and avoid depressed scars. This can be achieved by passing suture loop which is wider in the deeper layers than superficial.
- Sutures should always be placed with any knots on the cutaneous side, to avoid corneal irritation.
- At the end of the surgery, traction sutures may be placed to close the lids and to stabilize the graft/flap during the healing phase.
Anesthesia
A mild sedative may be beneficial for anxious patients having surgery under local anaesthesia. Anaesthetic eye drops such as amethocaine 1% or oxybuprocaine (Benoxinate) 0.4% are given before skin preparation. Lignocaine (xylocaine, lidocaine) 2% with 1 : 80,000 or 1 : 200,000 adrenaline gives excellent anaesthesia for local infiltration or regional block. Onset of action is within 5 minutes and lasts for about an hour. A mixture of equal volumes of lignocaine and bupivacaine (Marcaine) 0.5% prolongs the anaesthesia. The adrenaline improves hemostasis. Warming the anaesthetic to body temperature reduces the discomfort of the injection. When edema of the tissue from a local anesthetic is not desired, such as concominant canalicular repair, regional anesthetic blocks can be utilized. For larger repairs, general anesthesia may be required.
Eyelid reconstruction of full-thickness lid defects involving margin
Small defect (up to 25% to 50% of lid length)
Small defects (upto 33%) can be reconstructed by direct approximation, as the lid has an inherent stretch ability. The defect is managed by pentagonal wedge excision with direct closure. The defect is first converted it into a pentagon with vertical sides covering height of tarsal plate and the two arms converging at the fornix like an inverted “V”.
To approximate the tarsus, we prefer the use of the buried vertical mattress technique in a “far-far-near-near-near-near-far-far” pattern, originally described by Burroughs et al[9]. The sutures are passed 3mm from the cut edge and at 3mm depth, coming back 1mm from the cut edge and at 1mm depth to complete the vertical mattress sutures. This is done using a 6–0 Vicryl suture. The lash line is then aligned with another simple interrupted 6–0 Vicryl suture, which is crucial for a good cosmetic outcome. Skin is then closed using 6-0 absorbable or non-absorbable sutures depending on surgeon preference.(Figure 5)
If there is some tension (defects of size 33% to 50%), a lateral canthotomy and cantholysis of the LCT of the corresponding lid can be done. The most important aspect of this repair technique is alignment of the lash line and eversion of the lid margin wound edges to prevent a notched appearance.[9] [10](Figure 6,7)
Medium defect (50% to 75% of lid length)
Tenzel semi-circular advancement flap
The Tenzel semi-circular advancement was originally described in 1975 by RR Tenzel. The incision begins at the lateral canthus and curves superiorly and temporally in a semicircular fashion. This is followed by a lateral canthotomy and inferior cantholysis. A musculocutaneous flap is then dissected and advanced medially to cover the eyelid defect using buried vertical mattress technique as described by Burroughs et al.(Figure 8) The vertical extent should not cross the eyebrow for inferior eyelid defects and the flap should stay within the orbital margin or the arc defined by the eyebrow.[11] The orbicularis oculi is sutured to the periosteum of Whitnall’s tubercle to form the lateral canthal angle. The conjunctiva in the lateral fornix is dissected and advanced to the margin. Care should be taken to avoid damage to the lacrimal duct. (Figure 9)
Disadvantage:- The lateral lid would be devoid of cilia. [12][13][14]
McGregor flap
A Z-plasty at the end of a Tenzel flap will recruit more tissue from the vertical temporal area and provide horizontal tissue to the eyelid. This extension is known as McGregor flap (Figure 10) and is useful for both the upper and the lower eyelid reconstruction.[15][16]
Large defects(>75% of lid length)
Upper lid
A reverse tenzel semicircular advancement flap, can be used for upper eyelid defects upto 2/3rd of defect. For larger defect lid sharing procedure (Cutler-Beard), sliding tarsoconjunctival advancement flap or a reverse Hughes flap is the norm.
Cutler–Beard bridge flap
It was first described in 1955 by NL Cutler and C Beard.It is a two-stage full-thickness advancement flap from the lower eyelid[17] .(Figure 11) A full-thickness (cutaneo-myo-conjunctival) incision is made 1 to 2 mm below the inferior portion of the tarsal plate. This preserves the tarsus and also avoids the inferior marginal arcade, maintaining the flaps vascularity. The two vertical limbs of the flap are inferiorly directed to the conjunctival fornix. The flap is then advanced under the bridge of the intact inferior eyelid margin. Complementary structures are sutured to each other using a 6-0 vicryl in a interrupted fashion. Few authors, also describe the use of conchal/ nasal cartilage graft sutured to the remaining tarsus to provide rigidity. The skin is then closed using nonabsorbable suture. Dog ears at the lower end must be taken care of.(Figure 11)
After 6 to 8 weeks, the pedicle is divided and the upper eyelid conjunctiva is advanced anteriorly onto the lid margin for 2 mm, to prevent any corneal erosions.(Figure 12) The skin is incised 1–2 mm below the lid margin to compensate for retraction.
Disadvantages:- Healing is slow because of lymphedema. Lower eyelid ectropion is common because of denervation. Upper eyelid entropion is a problem in many patients. Skin and lanugo hairs of the new eyelid rub on the cornea because the levator tends to pull the new posterior lamella more than the new anterior lamella. It is not suitable for monocular patients or infants because risk of amblyopia. Adding to all of the above, the new lid margin lacks lashes.
Mustarde lid switch flap
This flap transfers full-thickness lower lid, together with the lashes, into the upper lid defect. The height depends on the height of the defect. Leave at least 2 mm between the flap and the lacrimal punctum. Cut the flap starting at the end opposite to the pedicle, taking care not to damage the vascular supply in the pedicle. A quarter of the lid length is marked from the lateral end of the defect. [18]This forms the hinge. The flap is marked on the medial side of the hinge. The size should be the size of the defect minus one-fourth of the lid length. The flap is incised full- thickness except at the hinge where it is stopped 4 mm from the lid margin[19].(Figure 13)
The pedicle can be divided 2 to 3 weeks later. Freshen the exposed edges to allow accurate closure of the pedicle end of the flap to the upper lid. Close the upper lid in layers as usual.
So, when neither of the above is preferred, a sliding tarsoconjunctival flap from the adjoining area / free tarsoconjunctival graft from the other lid is a good option for replacing the posterior lamella. The anterior lamella is fashioned with either a rotational flap(Fricke's flap, glabellar flap or midline forehead flap) or using a full-thickness skin graft. This avoids the need for a two staged procedure and limitations of lid sharing procedures, while still achieving an aesthetically pleasing result and restoring function.[20]
Glabellar flap
The glabellar flap was first described by McCord and Wesley[21] and involves an inverted V incision in the median forehead area between the eyebrows, which is partly closed as a Y and the rest of the flap is rotated into the adjacent medial canthal defect. It can also be seen as a combination of a V-Y and a rhomboid flap. This is not an axial flap, so the length cannot be as long as a median forehead flap. The loose glabellar tissues are incised and undermined The flap is rotated 90–120 degrees into position. Good results occur because the thickness, colour, and texture match well and is single staged.(Figure 14)[22][23]
Disadvantages:- It does not give a natural depth to the medial canthus, results in a bulky nasal bridge and draws the eyebrows together. This flap is best used for small defects above the medial canthal tendon. As the defect becomes larger or more inferior, there is considerable tension at the nose where the flap is rotated, giving unsatisfactory results.
Lower Lid
Large defects involving more than half of the lower lid requires a different calibration than the upper lid. Here, the posterior lamella can be formed either by using Hughes flap or a free mucoperichondrial flap (nasal septum or palate) and the anterior lamella is formed using a myocutaneous advancement flap like Mustarde cheek rotation transposition flap, lateral or median forehead flap, Tripier flap or a Fricke flap, or a skin graft.
Hughes tarsoconjunctival flap
Wendell Hughes first described a tarsoconjunctival flap in 1937[24],which was based on an earlier procedure described by Dupuy-Dutemps, who had also described the dacryocystorhinostomy flaps[5]. It is also a two-staged lid sharing procedure.
Regardless of the location of the lower eye lid defect, the flap is raised from the central part of the upper lid where the tarsal plate has the largest vertical dimension. The leading edge of the flap is 4 mm superior to the eyelid margin, leaving a strip of tarsal plate for structural support. The vertical limbs of the flap are made perpendicular to the leading edge with the incision carried superiorly toward the fornix. The flap is then advanced across the palpebral aperture, and the edges are sutured to the remaining lower eyelid tarsus or canthal tendons using 6–0 Vicryl suture, and the leading edge is sutured to the lower eyelid retractors using 6-0 or 7-0 Vicryl suture.(Figure 15)
Disadvantages: - Two-staged lid sharing procedure has similar problems like that of Cutler Beard flap. It may also result in upper eyelid retraction, therefore, careful dissection of the levator muscle complex from the tarsoconjunctival flap is to be done before advancing to the lower eyelid defect. In some patients, conjunctiva will heal slightly over the edge of the new lid margin, which can create erythema as a result of drying of the conjunctiva. However, as compared to Cutler Beard flap, the results are very good, as lashes in the lower lid are normally less appreciated.
Mustarde cheek rotation flap
This is a very useful flap for reconstructing the anterior lamella in larger vertical defects of lower lid. The flap is marked lateral to the defect extending to the lateral canthal area. It should then curve upward and carried down in front of the ear.
Some quick tips include staying in the subcutaneous cheek plane (“fat up and fat down” when dissecting the flap) and using wide areas of undermining to allow the cheek to be rotated with minimal tension. In some patients, a small back-cut or notch at the inferior extent of the incision helps in easy closure.[25][26]The medial end of the defect should be vertical. This helps in reducing the dog-ear. The medial end of the skin flap should be anchored to the medial wall of the orbit. Laterally, it also must be anchored to the lateral wall. Skin is closed using 5-0 or 6-0 suture depending on surgeon preference. (Figure 16)
Disadvantages: - Lower lid retraction, dog-ear, dissection of a large area, sacrifice of the orbicularis of the lower lid and a lack of surgical expertise, all prove to be disadvantageous. Lacrimal drainage has to be potentially reconstructed in second sitting if involved. Also, the preauricular hairline gets distorted.
Myocutaneous flaps useful for both upper and lower lid defects
There are certain specialized flaps which can be used for either of the lids for reconstruction.
Fricke’s flap
It is a lateral forehead flap for large defect including the lateral canthus. It was first described by Jochim Fricke in 1829[27]. The flap should be shaped along the curve of the eyebrow up to the medial end. A laterally based skin flap above the eyebrow is raised and sutured using 5-0 or 6 -0 suture to the defect area. The donor area is closed directly. (Figure 17) Posterior lamella may now be constructed using a reverse Hughes tarsoconjunctival flap or free mucous membrane graft. After 2 weeks, the flap is divided.(Figure 18)
Disadvantage: - Thick skin hinders proper excursion of upper lid. Donor site results in a raised eyebrow.
Paramedian forehead flap
A versatile flap that can be used to reconstruct medial canthal defects below the level of the canthus, involving the nose, cheek, or lower eyelid. The flap is a long axial flap with its base centered on its blood supply, the supratrochlear artery. These flaps are typically created contralaterally to the side of the medical canthal defect to reduce torsion on the pedicle base. is raised from the centre of the forehead depending on the width needed. The plane of dissection is deep, extending to the loose areolar tissue anterior to the periosteum of the frontal bone. The tip of the flap is thinned to the subcutaneous tissue plane. The flap is rotated 120–180 degrees into position covering the defect. A wide area of undermining is necessary to close the forehead wound. The second-stage operation is performed 6 weeks post-operatively. The redundant tissues at the base of the flap are incised and removed.[4]
Tripier flap
In 1889, Tripier first described the use of an innervated myocutaneous flap in the form of a bipedicle flap (with lateral and medial pedicles) from the upper lid, for reconstruction of a lower lid defect[28]. It is like a bucket handle and is possible only if there is lax skin available. It is mainly used in reconstructing smaller defects that don't involved the posterior lamella, but skin grafting can be added to the flap for larger defects. (Figure 19)
Eyelid reconstruction in anterior lamellar defects
Primary closure with or without undermining
Primary closure can be done in periocular areas that have redundant skin like the glabella, the upper lid skin fold, and the temple. There is normally little redundant skin in the lower eyelid or medial canthus. If required, tissue surrounding the defect must be undermined to decrease any tension in wound closure. Within the orbital rims, any tissue undermining should be done in the preseptal plane, while for areas outside the rim in the subcutaneous tissue plane .
When reconstructing the lower lid, minimize any vertical traction on the eyelid by closing wounds to leave a vertical scar and avoid ectropion or lid retraction. Avoid danger areas for the facial nerve, especially over the zygomatic arch and areas more than 1cm lateral to the brow.
Laissez faire
This is a method of healing by secondary intention/granulation formation. Fox and Beard were the first to describe it. It is applicable for relatively small medial canthal defects, as the region is concave and therefore, heals well[29]. Superficial surgical defects of the eyelid or shallow anterior lamellar defects also heal well by this method. In poor surgical candidates who are not fit for surgery, this option may be tried.[29][30]
Skin grafts
Skin grafts are either full- thickness (both epidermis and dermis along with some subcutaneous fat) or partial thickness (entire epidermis and part of dermis). Full- thickness grafts provide better cosmesis and are therefore, preferred in reconstruction in the periocular area. However, when the areas are extensive and the nearby areas also have to be resurfaced, a split skin graft becomes the choice. Donor sites for full-thickness skin grafts include upper eyelid skin, retroauricular skin, preauricular skin, supraclavicular skin, and upper arm skin. Grafts taken from the contralateral eyelid provide the best tissue match, however, the most practical donor site is retroauricular skin. [10][31]
Grafts for pretarsal defects, need not be oversized; however, if being used in the medial canthal location or preseptal location, then the graft should be oversized by 10% and 30%, respectively, to prevent secondary complications from contracture. [10]After harvesting, graft debulking must be done, to remove excess fat. The graft is sutured at the recipient site depending on surgeon preference. Silk sutures can tied down over a xeroform petroleum gauze to act as a pressure dressing (bolster) as well. If a bolster is used, it's usually left in place for about 5 to 7 days for proper integration. (Figure 20)
The stages of skin graft take are plasmatic imbibition (24-48hours), inosculation (3rd to 5th day) - donor and recipient capillaries are aligned and revascularization – graft revascularized through 'kissing' of capillaries.
Flaps
Myocutaneous flaps in the periocular area are formed of skin and orbicularis muscle. They have many advantages over free skin grafts: a) available local tissue b) good match for color and texture, c) near normal innervation, d) blood supply allows use over bare bone, e) high rate of successful healing and f) excellent function. [32]
The various flaps used in periocular area can be divided into 5 types:
- Sliding flap (Fig 21A): Undermining is done surrounding a ellipse to close the defect.[7]
- Advancement flap (Fig 21 B,C): The surrounding skin is converted into a three sided flap, which is dissected and advanced on its own long axis to close the defect. It can be single or double advancement flap (H plasty).[7]
- Rotation flap (Fig 21 D1,2,3): These flaps are commonly used in the periocular area, where the directly adjacent skin is lifted and rotated on itself to fill the defect.[7]
- Transposition flap (Fig 21 E): In these flaps, the skin not directly adjacent, but close to the defect, is lifted over the intervening skin and fitted into the defect. The angle of rotation should be small so as to prevent any compromise of blood supply to the tip.[7]
Special Transposition flap
a)Limberg rhomboid flap (Fig.22): Originally described by Alexander Limberg in 1946, it is one of the most useful flaps in periocular area.[33] A rhomboid defect is created with the vertical long axis or two triangles touching the base at the midway point of the defect and using a triangular flap drawn in a rhomboid shape, which can be rotated into the adjacent defect.
b)Bilobed flap (Fig. 23): The bilobed flap was originally described by Esser in 1918 for reconstruction of defects of the nasal tip[34][35]. This flap is widely used for circular defects of the nose, cheek, forehead and medial canthal defects. It consists of 2 adjacent transposition flaps on a common pedicle, wherein the original defect is filled by the first larger flap and the second smaller flap fills in the defect left by the first. The angle between the two lobes can be varied from 30° to 120°.[35]
- Island flap (Fig 21 F): This flap consists of a free island of skin and muscle, where the flap is freed from all sides, but remains attached to a central subcutaneous pedicle; and then advanced in any direction to fill in the defect.
Lateral canthal defects
Lateral canthus can be reconstructed by anchoring the remnant tarsal plate to a periosteal flap raised from the lateral wall of the orbit of a recommended 4mm width. A fascial graft from temporalis fascia or palmaris longus tendon can also be used instead and anchored to the lateral wall of the orbit via drill holes made in the bone. The fixation of the lateral tendon should be 3 mm above the level of medial canthus.[36]
A skin graft, Hewes tarsoconjunctival transposition flap or an island flap based on superficial temporal artery branch can be used for filling the skin defect.
Medial canthal defects
Medial canthal defects are typically repaired using full-thickness skin grafts, glabellar flaps, or forehead flaps or allowed to heal by secondary intention. If a full-thickness defect is present, medial canthal attachments should be fixed to the peristeum or bone with heavy permanent sutures such (Prolene, Mersilene), wire, or titanium miniplates. Transnasal wiring may also be done in certain cases.(Figure 24)
Canalicular Repair
Canalicular injury are commonly seen associated with lower lid avulsion. The most widely accepted approach is to find the torn ends and place a well tolerated stent temporarily in the system. Stents can be mono or bi canalicular depending on surgeon preference. In cases of unavailability, a 22 or 24 gauge IV cannula or a silicone rod can be put in situ. The stents are typically left in place for at least 2-3 months to allow for proper healing.
Identification of proximal end of canaliculus is done under high magnification. It appears paler than the surrounding area and often is described as looking like calamari. If the end is difficult to find, you can pool sterile saline in the wound and watch for air bubbles while injecting air from the other intact canaliculus. Another method described is the use of fluorescein dye injection from intact canaliculus coming out through the proximal cut end. A pigtail catheter can be used with extreme caution in order to not create a false passage during repair(Figure 25).
Conclusion
Eyes are the focal point for facial cosmesis and accordingly acceptable cosmesis in reconstruction becomes a major requisite. There are a variety of techniques available for periocular reconstruction. While choosing a method, the specific function of the area of the eyelid has to be kept in mind. The upper eyelid should be reconstructed with lightweight, pliable tissue as it is for mobility. The lower eyelid is for stability along with the canthii, hence, it must be stabilized well. A thorough knowledge of the complex eyelid anatomy and familiarity with the numerous reconstructive techniques is, therefore, imperative.
Video
Cutler Beard flap repair for upper lid full thickness defect in a case of abortive cryptophthalmos. https://youtu.be/T7mG3MAeDQQ (Surgeon - Prof. Neelam Pushker MD, AIIMS, New Delhi)
References
- ↑ HowardG. Eyelidretraction. In:YanoffM, DukerJ, eds. Ophthalmology. 4th ed. Philadelphia, PA: Elsevier Health Sciences; 2013:1268.
- ↑ Sand JP, Zhu BZ, Desai SC. Surgical anatomy of the eyelids. Facial Plast Surg Clin North Am 2016;24(02):89–95.
- ↑ Burkat CN, Lemke BN. Anatomy of the orbit and its related structures. Otolaryngol Clin North Am 2005;38(05):825–856.
- ↑ Jump up to: 4.0 4.1 4.2 Korn, Bobby S et al. “BCSC Section 7: Oculofacial Plastic and Orbital Surgery.” San Francisco, CA. American Academy of Ophthalmology 2023
- ↑ Jump up to: 5.0 5.1 Porfiris E et al. Upper eyelid orbicularis oculi flap with tarsoconjunctival island for reconstruction of full-thickness lower lid defects. Plast Reconstr Surg 1999; 103:186-91.
- ↑ Cannon PS, Madge SN, Kakizaki H, Selva D. Composite grafts in eyelid reconstruction: the complications and outcomes. Br J Ophthalmol. 2011 Sep;95(9):1268-71. doi: 10.1136/bjo.2009.170548. Epub 2010 Dec 22. PMID: 21183515.
- ↑ Jump up to: 7.0 7.1 7.2 7.3 7.4 Patrinely JR, Marines HM, Anderson RL. Skin flaps in periorbital reconstruction. Surv Ophthalmol 1987; 31:249-61.
- ↑ Bowman PH, Fosko SW, Hartstein ME. Periocular Reconstruction. Semin Cutan Med Surg 2003; 22:263-72.
- ↑ Jump up to: 9.0 9.1 Morley AM, deSousa JL, Selva D, Malhotra R.Techniques of upper eyelid reconstruction. Surv Ophthalmol 2010; 55(03):256–271.
- ↑ Jump up to: 10.0 10.1 10.2 DiFrancesco LM,Codner MA, McCord CD. Upper eyelid reconstruction. Plast Reconstr Surg 2004; 114(07):98e–107e.
- ↑ Tenzel RR, Stewart WB. Eyelid reconstruction by the semicircle flap technique. Ophthalmology 1978; 85:1164-9.
- ↑ TenzelRR. Reconstruction of the central one half of an eyelid. Arch Ophthalmol 1975; 93(02):125–126.
- ↑ Tenzel RR, Stewart WB. Eyelid reconstruction by the semicircle flap technique. Ophthalmology 1978; 85(11):1164–1169.
- ↑ Levine MR, Buckman G. Semicircular flap revisited. Arch Ophthalmol 1986;104(06):915–917.
- ↑ Chandler DB, Gausas RE. Lower eyelid reconstruction. Otolaryngol Clin North Am 2005;38(05):1033–1042.
- ↑ Almeida, Augusto C. et al. “McGregor flap: an alternative for lower eyelid and periorbital region reconstruction.” Revista brasileira de cirurgia 33 (2018): 229-235.
- ↑ Cutler NL, Beard C. A method for partial and total upper lid reconstruction. Am J Ophthalmol 1955;39(01):1–7
- ↑ Mustarde JC. 2nd ed. Philadelphia: Churchill Livingstone; 1991. Repair And Reconstruction in the Orbital Region.
- ↑ Tyers AG, Collin JRO. Colour Atlas of Ophthalmic Plastic Surgery. 4th ed. Elsevier Health Sciences,2018.Chapter 17: Eyelid reconstruction – anterior and posterior lamella combined; p.449-50.
- ↑ Malik A, Shah-Desai S. Sliding tarsal advancement flap for upper eyelid reconstruction. Orbit 2014;33(02):124–126.
- ↑ Meadows AE, Manners RM. A Simple Modification of the Glabellar Flap in Medial Canthal Reconstruction. Ophthal Plast Reconstr Surg 2003; 19:313-5.
- ↑ Maloof AJ, Leatherbarrow B. The glabellar flap dissected. Eye (Lond) 2000;14(Pt 4):597–605.
- ↑ Field LM. The glabellar transposition “banner” flap. J Dermatol Surg Oncol 1988;14(04):376–379.
- ↑ Rohrich RJ, Zbar RI. The Evolution of the Hughes Tarsoconjunctival Flap for Lower Eyelid Reconstruction. Plast Reconstruct Surg 1999; 104:518-22.
- ↑ Mustardé JC. The use of flaps in the orbital region. Plast Reconstr Surg 1970;45(02):146–150.
- ↑ Mustardé JC. Major reconstruction of the eyelids: functional and aesthetic considerations. Clin Plast Surg 1981;8(02):227–236.
- ↑ Wilcsek G, Leatherbarrow B, Halliwell M, FrancisI. The ‘RITE’ use of the Fricke flap in periorbital reconstruction. Eye 2005; 19:854-60.
- ↑ Elliot D, Britto JA. Tripier’s innervated myocutaneous flap1889.Br J Plast Surg 2004;57(06):543–549.
- ↑ Jump up to: 29.0 29.1 Fox SA, Beard C. Spontaneous lid repair. Am J Ophthalmol 1964; 58:947–952.
- ↑ Harrington JN. Reconstruction of the medial canthus by spontaneous granulation (Laissez-Faire): a review. Ann Ophthalmol 1982;14(10):956–960, 963–966, 969–970.
- ↑ Madge SN, Malhotra R, Thaller VT et al. A systematic approach to the oculoplastic reconstruction of the eyelid medial canthal region after cancer excision. Int Ophthalmol Clin 2009;49(04): 173–194.
- ↑ Nerad JA. Techniques in Ophthalmic Plastic Surgery.1st ed. Elsevier Health Sciences,2010. Chapter 12: Lid Reconstruction;p.332.
- ↑ Turan T, Kuran I, Ozcan H, Bas L. Geometric Limit of Multiple Local Limberg Flaps: A Flap Design. Plast Reconstr Surg 1999;104:1675-8.
- ↑ Iida N, Ohsumi N, Tonegawa M, Tsutsumi K. Simple method of designing a bilobed flap. Plast Reconstr Surg 1999; 104:495-9.
- ↑ Jump up to: 35.0 35.1 Sullivan TJ, Bray LC. The bilobed flap in medial canthal reconstruction. Aust NZJ Ophthal 1995; 23:42-8.
- ↑ Subramanian N. Reconstruction of eyelids. Indian J Plast Surg. 2011 Jan-Apr; 44(1): 5–13.