Basal Cell Carcinoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease
Basal Cell Carcinoma (BCC) is a malignant epidermal carcinoma. BCC is the most common eyelid malignancy, accounting for over 90% of malignant eyelid neoplasms.
Etiology
Ultraviolet light (particularly UVB) induced damage to the epidermis.
Risk Factors
BCC tends to occur in lightly pigmented individuals at sites of sun exposure, although it may occur with any skin tone.
Other risk factors include:
- Radiation
- Immunosuppression, including solid organ transplant
- Previous scar
- Inherited syndromes, e.g., xeroderma pigmentosum
General Pathology
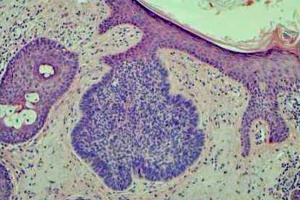
As its names implies, BCC derives from cells of the epithelial basal cell layer. Histologically the tumor has an appearance similar to the normal epithelial basal cell layer (Figure 1). BCC forms strands, cords, and islands of tumor. Palisading of the nuclei at the periphery of the islands of tumor is characteristic (Figure 1). An additional distinguishing feature of the tumor is the clefts or separation artifact, which results from tissue processing. Both nodular and morpheaform tumor growth types are seen in the periocular region.
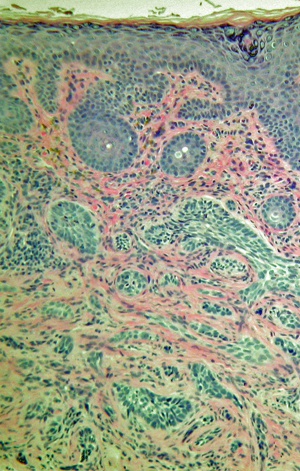
The morpheaform type, also known as sclerosing or fibrosing type, characteristically has small islands of tumor within dense fibrous tissue (Figure 2). The nests and strands of tumor tend to invade the underlying tissue more deeply. The more aggressive pattern of the morpheaform type presents a challenge in determining the extent of the tumor; the variant carries a higher rate of recurrence.
Pathophysiology
Defects of the PTCH gene located on chromosome 9q22.3 have been associated with the development of BCC.
Primary prevention
Minimize sun exposure by use of sun block products, as well as hats, sunglasses, and appropriate clothing.
Diagnosis
The diagnosis of BCC can be suspected clinically and is confirmed histologically following incisional biopsy.
History
The history for any suspicious periocular mass lesion should include assessment for any of the risk factors for BCC. The location of the lesion is noteworthy. Due to a relatively greater amount of sun exposure, BCC has a predilection for the lower eyelid, followed by the medial canthus.[1]
Physical examination
Complete eye examination, including ocular motility and assessment of proptosis to assess for orbital extension. This is especially relevant for medial canthal lesions, as they are more likely to extend into the orbit.
Assessment of facial sensation
Examination of the lesion includes assessment for:
- General appearance and extent of the lesion and periocular skin
- Distortion of eyelid architecture or eyelid malposition
- Presence of skin ulceration
- Madarosis (loss of eyelashes)
- Telangiectasias
Symptoms
- May be asymptomatic
- Ulceration and bleeding
- Non-healing skin lesion
- Skin crusting
- Paresthesia or anesthesia
- Eyelash loss (madarosis)
- Distortion of normal eyelid margin or tissue architecture
Diagnostic procedures
Biopsy (incisional or excisional, depending on the size and location).
Differential diagnosis
The differential diagnosis includes any benign or malignant condition of the eyelid skin, including:
Benign
- Seborrheic keratosis
- Actinic keratosis
- Chalazion
- Cyst
- Squamous papilloma
- Blepharitis
- Xanthelasma
- Nevus
- Verruca
- Sebaceous hyperplasia
Malignant
- Squamous cell carcinoma
- Sebaceous gland carcinoma
- Malignant melanoma
- Lymphoma
- Merkel cell tumor
- Metastasis
Management
BCC is nearly always a locally invasive disease. Treatment is recommended to prevent damage to neighboring tissues.
Medical therapy
Treatment with topical imiquimod 5% cream has been shown to be effective, although not as effective as surgical excision, in several case series.[2] More aggressive BCC has also been successfully treated with medication that targets the sonic hedgehog pathway, including vismodegib. Further studies are needed to evaluate the extent of histopathologic resolution or changes from vismodegib. [3]
Surgery
Complete surgical excision with margin control. Assuring that the surgical margins are without cancerous cells may be accomplished by frozen sectioning or Mohs surgery.
Complications
Recurrence of the tumor.
Prognosis
Five-year cure rates of up to 98% have been reported for BCC. There is a worse prognosis with:
- Lesions greater than 3 cm
- Long-standing lesions
- Deeply invasive tumors
- Inadequate treatment
Additional Resources
- http://emedicine.medscape.com/article/1211925-overview
- http://www.eyecancer.com/patient/Condition.aspx?nID=12&Category=Eyelid+Tumors&Condition=Basal+Cell+Carcinoma
References
- ↑ Cook BE Jr., Bartley GB. Epidemiologic characteristics and clinical course of patients with malignant eyelid tumors in an incidence cohort in Olmsted County, Minnesota. Ophthalmology. 1999 Apr;106(4):746-50.
- ↑ Beutner KR1, Geisse JK, Helman D, Fox TL, Ginkel A, Owens ML. Therapeutic response of basal cell carcinoma to the immune response modifier imiquimod 5% cream. J Am Acad Dermatol. 1999 Dec;41(6):1002-7.
- ↑ Gill HS, Moscato EE, Chang AL, Soon S, Silkiss RZ. Vismodegib for periocular and orbital basal cell carcinoma. JAMA Ophthalmol. 2013 Dec;131(12):1591-4. doi: 10.1001/jamaophthalmol.2013.5018.
- Ophthalmic Pathology and Intraocular Tumors, Section 4. Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 2009.
- Orbit, Eyelids, and Lacrimal System, Section 7. Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 2009.
- Sehu KW, Lee WR. Ophthalmic Pathology. Oxford: Blackwell Publishing, 2005: 25, 27-30.
- Srivastava M, Kelley L. Mohs' Surgery for Eyelid Malignancies. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology, 3rd ed. Philadelphia: W.B. Saunders, 2008;3:248.
- Valenzuela AA, Sullivan TJ. Basal Cell Carcinoma in the Eyelid. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology, 3rd ed. Philadelphia: W.B. Saunders, 2008;3:249.
- Yanoff M, Sassani JW. Ocular Pathology, 6th ed. Philadelphia: Mosby Elsevier, 2009: 197-199.