Astigmatism Correction at the Time of Cataract Surgery
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
What is astigmatism?
Astigmatism is a common eye condition that exists when the surface of the cornea or crystalline lens is irregularly shaped. It is a form of refractive error that can be present alone or in combination with myopia and hyperopia. Its correction requires the use of cylinder lens power.
The eye’s total refractive astigmatism is a combination of corneal and lenticular astigmatism. Most astigmatism comes from the cornea. The average lenticular astigmatism is 0.5 diopters against-the-rule (ATR). The amount of lenticular astigmatism can be calculated by subtracting corneal astigmatism from the total astigmatism found by refraction. Since lenticular astigmatism is eliminated with extraction of the cataract only the corneal astigmatism is considered when planning cataract surgery [1].
In a meta-analysis that looked at studies around the world from 1990-2016, the prevalence of astigmatism greater than 0.5 D in the world is estimated to be 40.4% (95% CI: 34.3%-46.6%) in adults over 30 years old and 14.9% (95% CI: 12.7-17.1%) in children under 20 years old[2]. This makes astigmatism the most common refractive error in the world. Specifically for patients undergoing cataract surgery, a systematic review from 1996-2015 found there was preexisting astigmatism greater than 1.0 D in 47% of eyes[3]. In this review the prevalence of mild astigmatism (<1.5 D) ranged from 74.6-89.6%, moderate astigmatism ( >1.5- <2.5 D) ranged from 8.1-14.9%, and significant astigmatism (>2.5 D) ranged from 2-6.8% in various countries around the world[3].
Patients with 1.0 D or more of astigmatism are shown to benefit from correction during or after cataract surgery, as visual acuity can decline to 20/25 with 0.75 D and 20/40 with 1.5 D of astigmatism[4]. In general, the goal when correcting astigmatism during cataract surgery should be a post-operative residual astigmatism of 0.5 D or less [4] .Another metric that has been used to evaluate the success of astigmatism correction is independence from spectacles after cataract surgery, as the use of spectacles is correlated with a higher financial burden for the patient[3].
Classifications of Astigmatism
In a spherical cornea or lens the curvature is the same in all meridians. When astigmatism is present there are two principal meridians. One with greatest curvature (steepest) the other with least curvature (flattest)
Regular astigmatism
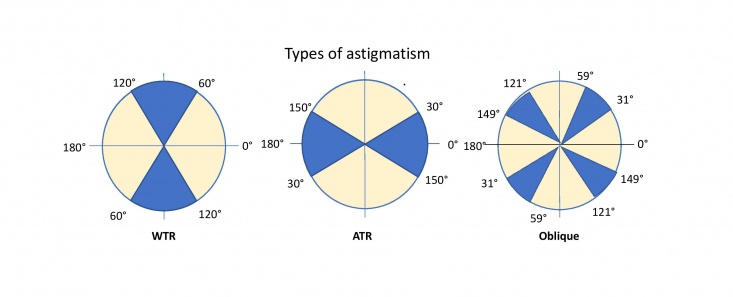
Regular astigmatism exists when the two principal meridians are 90 degrees apart. Regular astigmatism can be fully corrected with a cylindrical lens[4][5]. The great majority of astigmatism in eyes is regular. Regular astigmatism can be further classified into three types based on which meridian is the steepest.
With-the-rule (WTR) astigmatism : The steepest meridian is vertical or within 30 degrees of the 90 degree meridian (between 60 and 120 degrees)[5].
Against-the-rule (ATR) astigmatism: The steepest meridian is horizontal or within 30 degrees of the 180 degree meridian (between 0 to 30 and 150 to 180 degrees)[5]. This type of astigmatism is more common in older patients, due to age related changes[6].
Oblique astigmatism: The steepest meridian is not within 30 degrees of the horizontal or vertical meridians (31 to 59 degrees and 121 to 149 degrees)[5].
Irregular astigmatism
Whenever the two principal meridians are not symmetric and do not lie 90 degrees apart (orthogonal) the astigmatism is considered irregular. It is always a pathologic condition. Causes of irregular astigmatism include corneal epithelial basement membrane dystrophy, corneal degeneration, corneal scarring, pterygium, keratoconus, ocular surface disease, or prior corneal surgery. Unlike regular astigmatism, irregular astigmatism cannot be fully corrected by cylindrical lenses[7].
Preoperative imaging for the treatment of astigmatism during cataract surgery
Accurate biometry is essential for correct IOL selection and the planning of astigmatism correction to achieve targeted visual results. The current generation of optical biometers, such as the Zeiss IOL Master 700, Haag Streit Lenstar and others, programmed with the latest IOL formulas, provide remarkably accurate biometry measurements for IOL selection and astigmatism treatment. These machines, in addition to accurate axial length and anterior chamber depth, provide excellent reproducible keratometric measurements. Many surgeons rely on these machines as their sole method of selecting monofocal, multifocal and toric IOL powers as well as planning for incisional correction of astigmatism. As reliable as these machines are, given the high expectations of today’s cataract patients, most experts recommend verifying keratometric measurements with manual keratometry, corneal topography or corneal tomography. If this testing is not available, biometry can be repeated, optimally on a second visit, to confirm the readings. Some surgeons advocate using the average reading from multiple sources.
Keratometry
Keratometry is the measurement of corneal curvature and the refracting power of the cornea. It determines the degree of astigmatism, if present, as well as the axis of its orientation. The findings are used for IOL calculations as well as to help identify corneal pathology, as a starting point for refraction and as an aide in classifying refractive error as corneal vs axial. The amount of astigmatism is calculated by finding the difference between the two principle meridians.
The manual keratometer, invented over 200 years ago, is still today a reliable method of corneal measurement. It has the advantage of also providing a qualitative assessment of the optical integrity of the corneal surface, but the disadvantage of measuring only the central 3.5 mm of the cornea.
Topography and Tomography
Corneal topography is used to assess the shape of the anterior corneal surface, essentially creating a 2D map. Specifically for cataract surgery it can help verify the degree and axis of corneal astigmatism found with biometry and more importantly how regular or irregular the astigmatism is. Since toric IOLs will only correct regular astigmatism topography is an important tool in determining which astigmatism treatment option is appropriate for the patient [6][7].
Tomography is a more advanced system of corneal measurement creating a 3D model which provides information on the posterior as well as anterior corneal surface[8]. Studies have shown that the posterior corneal astigmatism, while generally small in magnitude compared to the anterior corneal astigmatism, can have a significant effect on total corneal astigmatism and for best post-operative results should be factored into calculations for astigmatism correction. Surprisingly, a study comparing IOL formulas using estimates of posterior corneal power, such as the Barrett Toric Calculator and the Abulafia-Koch formula, yielded better post-op results than formulas using actual posterior corneal measurements[9].
The newest generation of instruments also adds wavefront aberrometry to tomography producing remarkably detailed assessment of the eyes optical state. In addition to the usual topographic information they provide measurements of aberrations such as spherical, coma, trefoil, and many higher order aberrations. They also measure angle kappa, angle alpha and perform a plethora of analytic calculations. Many provide preoperative tools to help with IOL selection and placement and post-op assessment to determine if the lens is correctly positioned or may need to be rotated or exchanged. These machines can aide the surgeon in predicting which patients are and which are not good candidates for toric and multifocal lenses.
Topography, tomography and wavefront aberrometers can all be used to verify keratometric readings obtained through biometry, and since they are creating multidimensional models of the cornea, they can identify corneal pathologies not identifiable with routine biometry.
Methods of correcting astigmatism during surgery
Toric IOLs
How they work
Toric IOLs differ from spherical IOLs as they have different powers in different meridians. When a toric IOL of the appropriate cylinder power is inserted into the eye and rotated into the correct axis it can correct the patient’s corneal astigmatism.
In addition to the cylinder power of a toric IOL it also has a spherical power. As in any spherocylinder spectacle lens it can be thought of as the combination of a spherical lens with a planocylinder lens. The spherical power in a toric IOL is calculated using the axial length, average corneal curvature and in the most current IOL formulas the anterior chamber depth. The spherical power of a toric IOL is the same IOL power that would be used for the eye if astigmatism was not being corrected.
Toric IOLs are currently available with cylinder powers ranging from 1.5 D to 6.0 D. These lenses provide astigmatism correction of 0.75 D to 4.75 D at the corneal plane [8][10][11].
The spherical power and cylinder power of a toric IOL are both indicated in the description of a toric IOL.
For more information on specific toric lenses, refer to the Toric IOL wiki page https://eyewiki.aao.org/Toric_IOLs
Additional biometry considerations for toric IOLs
Multiple formulas are available on-line for calculating the appropriate toric IOL power. Popular formulas include the Barrett, Holladay and Abulafia-Koch. Many Lens manufacturers also provide access to formulas such as Alcon’s https://www.acrysoftoriccalculator.com/ and Tecnis’ https://www.tecnistoriccalc.com/
Accurate preoperative and intraoperative marking of the eye is crucial to achieving good outcomes using toric IOLs. Immediately prior to surgery, either in the holding area or the OR, the patient is seated upright and while fixating straight ahead the limbus is marked at the 3:00, 6:00 and 9:00 positions with a fine tip sterile marking pen. This can be done free hand or using specially designed instruments available to aide in accurately marking the eye. This must be done with the patient seated upright due to cyclorotation of the eye that occurs when lying flat. Once the patient is prepped and draped the steep axis of the cornea is marked using a toric axis marker. Many styles of toric axis markers are available. After the cataract is removed the toric lens is then inserted into the eye and rotated into position so the axis marks on the IOL are aligned with the pre-marked axis on the cornea.
Intraoperative aberrometers, such as the Alcon ORA system, can be used during surgery to measure the eye in the aphakic state to determine the correct IOL power and axis. Once the IOL is inserted, measurements can be taken to determine any residual refractive error confirming correct power and axis alignment. The lens power and axis can then be corrected intraoperatively preventing the need to return to the OR for a lens exchange or repositioning [8]. In a study in 2019 Davidson, Makari, and Potvin compared intraoperative aberrometry (IA), preoperative calculations, Barrett’s toric calculator, and the actual toric lens used in cataract surgery. They found that there was no significant difference between spherical power outcomes in the preoperative calculations and IA. However, there was a significant difference between residual astigmatism in the IA, Barrett toric calculator, and the preoperative method, namely 75% of the IA group were expected to have less than 0.5 D of residual astigmatism, 75% of the Barrett calculator group, and 53% of the preoperative calculation group[12]. Another study compared the use of the ORA system with VeriEye+ combined with the VERION Image Guided System to a surgeon’s standard of care in 84 eyes, in which they found that both techniques yielded similar outcomes in terms of post-operative refractive cylinder, UDVA, and CDVA[13]. For more information on how the Alcon ORA works, see this video from the UCLA Stein Eye Institute: https://www.youtube.com/watch?v=wvw_oG3U5U0
Benefits
Toric IOLs can correct higher amounts of astigmatism compared to LRIs and CCRI[14].
Toric IOLs have been found to produce the most reliable results, with the lowest post-operative astigmatism, for pre-operative astigmatism between 1.0-3.0 D[15] . They also provide the best postoperative uncorrected distance visual acuity (UCDVA) when compared to non-toric IOLs and LRIs. In addition, since toric IOLs do not require additional surgical wounds (vs LRIs), the recovery time for patients is generally faster[10].
Choosing a toric IOL may reduce costs for patients by lessening the need for contact lenses and spectacles[16]. They have the best outcome data for this metric, as the percentage of patients who needed spectacles for distance viewing after toric IOL implantation was 29.7% versus 53.2% when compared to the non-toric group[17]. Toric IOLs are now available as multifocal presbyopia correcting designs, so there is greater flexibility for independence from spectacles, depending on the patients’ wishes[8].
Disadvantages
It is possible for a Toric IOL to rotate from its initial position as the eye heals following the surgery and the capsule contracts around the IOL. For every degree the lens is rotated off axis, there is a 3.3% reduction in toric IOL power[18]. The higher the cylinder power the more significant is this effect. If vision becomes unsatisfactory it may become necessary to return to the OR for lens repositioning[14]. However, compared to the implantation of a non-toric IOL, a systematic review in 2016 found no significant difference in the prevalence of post-operative complications (4.2% in the toric group vs. 2.3% in the non-toric group in 1,032 patients)[17]. In addition, according to the review, most toric IOLs rotated less than 5 degrees[17].
The upfront out of pocket cost of toric IOLs is higher than regular IOLs, however the cost effectiveness of toric IOLs has been shown to be superior to other astigmatism correcting techniques when factoring spectacle independence and the potential cost if spectacles are required for satisfactory vision. Long term costs are important to discuss with patients when comparing the price of toric IOLs.
Contraindications
Patients with irregular astigmatism caused by corneal scars or ectasia are not optimal candidates. Zonular instability, posterior capsular dehiscence, poor pupillary dilation, severe dry eye and prior surgeries such as vitreoretinal procedures with buckling or glaucoma implants are all relative contraindications to use of toric IOLs[8] [11].
Limbal relaxing incisions (See: https://eyewiki.aao.org/Limbal_Relaxing_Incisions)
How they work
Limbal Relaxing Incisions (LRIs) are a subset of astigmatic keratotomies that can be used to correct astigmatism at the time of cataract surgery. They work by flattening the steep curvature of the cornea and allowing the eye to heal into a more spherical shape [19] [20].
LRIs can be either single or paired, with paired LRIs generally providing more astigmatism correction. In the case of irregular astigmatism, LRIs can be customized to the corneal topography since the lengths of the paired incision can differ[21].
In addition, femtosecond laser assisted cataract surgery (FLACS) technology can be used in the place of manual incisions for LRIs. A systematic review in 2016 showed the benefits of using FLACS over manual incisions including increased precision, predictability, and use in difficult cataract cases such as shallow anterior chamber, subluxated cataracts, white cataracts, and traumatic cataracts [22]. For treatment in astigmatic patients, the femtosecond laser can make the incisions to accurate depths and lengths, decreasing the chance of corneal perforation[22]. A study in South Korea found that overall, changes in astigmatism were more predictable in the femtosecond laser group than the conventional phacoemulsification, and patients were significantly more satisfied [23]. Femtosecond lasers are especially helpful when they include iris and limbus registration since they can account for cyclotorsion, which is a common cause of error in laser assisted surgery [22].
LRIs can correct up to 3.0 D of astigmatism, but are most predictably used to correct up to 1.5 D[8] [24]. As with the other methods of astigmatism correction, target outcomes of LRIs should be within .5 D or less of residual astigmatism.
Preoperative management
An LRI calculator such as Johnson and Johnson’s http://www.lricalculator.com can be used to determine arc length and number of incisions[20]. Based on the nomograms of Eric Donnenfeld and Skip Nichamin the calculator takes into account age, the distance the incisions are placed from the limbus, and corneal thickness [19] [20].
A preoperative slit lamp exam and peripheral corneal pachymetry should be performed to determine whether there is peripheral thinning, degeneration, or dellen formation near the limbus of the cornea. Since LRIs should be at 90% of corneal depth, it is important to take this into consideration to reduce the risk of corneal perforation[21].
Benefits
LRIs can be combined with toric lenses for patients with high astigmatism (greater than the IOL alone can correct )[25]. They can also be used when toric IOLs are contraindicated, such as with capsular break or zonular instability[25]. They are a great option in patients with pre-existing astigmatism who desire presbyopia correction with a multifocal or accommodating IOL although toric versions of these lenses are now available [8][14].
LRIs also have less tendency to cause axis shift than toric IOLs, which will be discussed in the “Flipping the Axis” section[20]. A 1:1 coupling ratio in bilateral incisions means there is no need to change the spherical IOL power after LRIs. Unlike toric IOLs, LRIs can be used to treat irregular astigmatism. LRIs can also be performed in the office post-operatively to address under correction. Over-correction of astigmatism can be corrected with suturing of the incision, after the refraction has stabilized[19].
Contraindications
Use with caution in patients with corneal ectasia, peripheral thinning, and advanced dry eye especially when associated with rheumatoid disease [15][25].
Potential complications
Epithelial defects can occur with LRI and increase post-op dry eye[9]. The incisions will need to be examined at the time of placement to ensure there is no corneal perforation. If there is, determine whether or not the perforation is self-sealing and suture with a 10-0 nylon as necessary[19]. Due to the extra incisions, post-operative patient discomfort is possible and the risk for infection is increased compared to a non-LRI cataract surgery[20].
Clear Corneal Incision (CCI) on the steepest meridian
How it works
The main surgical incision is aligned with the steep axis of cornea leading to a decrease in the astigmatism[10].
Historically, a single incision along the steep axis had the potential to correct a small, but clinically significant amount of astigmatism: 0.5 D according to Eyerounds and 1.0 D according to Kaufmann et al[14][24]. In recent years, as cataract surgery has evolved, phaco incisions have gotten progressively smaller, from 3.2 mm to 2.4 and even as small as 1.4mm. In a study comparing 2.2 mm and 3.0 mm on axis incisions, researchers found that the mean change in astigmatism between the two were significantly different, with the 2.2 mm incision inducing only 0.10 +/- 0.08 D and the 3.0 mm incision producing 0.32 +/- 0.20 D[26]. While microincisions are good for patients with little to no preexisting astigmatism, as they reduce the amount of surgically induced astigmatism, their usefulness as a technique to reduce astigmatism is also minimized[26].
A second phaco incision can be placed on the opposite side of the same axis increasing the astigmatic effect, up to 1.5 D[8]. Extending the width of the incision may provide greater astigmatic results, although this may necessitate suturing of the wound[10].
Advantages
CCIs are technically less complex and less calculations compared to toric IOLs and LRIs [10]. For single incisions no additional surgical manipulation of the corneal tissue is required. CCIs are the least expensive option for astigmatism correction.
Disadvantages
Depending on location of the steep axis the patient’s brow or nose can interfere with incision placement requiring repositioning of the patient or microscope making surgery more difficult[14].
Compared to toric IOLs and LRIs, significantly less astigmatism can be corrected. The reliability and degree of astigmatism that can be corrected are the biggest limitations to this technique.
Two-stage procedure with excimer laser ablation
How it works
Just as LASIK and PRK are used to correct myopia, hyperopia and astigmatism in the phakic eye, they can also be used to correct post cataract surgery residual refractive error[14].
Benefits
In addition to residual astigmatism, any unplanned residual spherical error can also be addressed. Specifically, it is good for patients with unexpected refractive errors after cataract surgery who desire greater spectacle independence[14]. Both LASIK and PRK have good evidence for use in correcting residual refractive errors after cataract surgery. Compared to lens based correction techniques, such as piggyback IOL or IOL exchange, LASIK correction was found to be safe, had higher cylinder reduction, and was the most reliable[27] .
Disadvantages
Due to the high cost of LASIK and PRK they are not used often for primary astigmatism correction unless there are contraindications to toric IOLs and LRIs.
Treatment considerations: Flipping the axis
Flipping the axis refers to changing the direction of the steep axis of astigmatism and usually occurs as a result of over-correction (with any of the above techniques). This can lead to residual astigmatism on the opposite meridian of the original axis. While many studies have shown that the magnitude of astigmatism is more important than the axis of astigmatism in terms of visual perception, the decision to over-correct astigmatism, thereby flipping the axis, or under-correct astigmatism is not straightforward[4].
The cornea tends to drift from WTR astigmatism to ATR astigmatism over adolescence to adulthood, although the degree of astigmatism varies from person to person[28]. According to Goto et al. ATR astigmatism is the most common type of astigmatism in adults greater than 40 years of age [29]. The amount of ATR change per decade is about 1/3 D, and occurs at a greater rate in men[4]. For more information about age-related corneal changes over time see https://eyewiki.aao.org/Physiology_of_Astigmatism#Natural_course_of_astigmatism_in_normal_eyes
Due to the change in the cornea over time, some surgeons may choose to leave up to 0.5 D of WTR astigmatism, which will theoretically shift towards 0 in the years following surgery[30]. This is especially appropriate to consider when performing cataract surgery on younger patients (<50)[30].
In a patient with clinically significant astigmatism who has used spectacles for treatment, their brains might be accustomed to correcting for a certain plane of astigmatism[31]. It may be necessary to decide whether to over-treat, leading to flipping the axis, or to under-treat, keeping residual astigmatism at the same axis. Most toric IOL calculators, by default, do not suggest an axis flip when determining which lens to use [32]. The Johnson & Johnson, Alcon, and Hoya calculators do permit axis flips, but will make note of it for the surgeon to ultimately decide[32].
The benefit of flipping the axis in older patients who already have ATR astigmatism is that they are more likely to have independence from spectacles if the lowest amount of residual astigmatism is targeted[32]. However, occasionally patients with small amounts of myopic, ATR astigmatism actually have an increased depth of focus that may counteract presbyopia increasing their near visual acuity[33]. It is possible that these patients may be dissatisfied with loss of this increased depth of focus if all astigmatism is corrected[30].
Summary
Toric lenses currently have the most predictable results, are the most cost-effective in the long term, can correct the highest amounts of astigmatism and are relatively easy to use. This method of correcting astigmatism is well-studied and has become more reliable with current technologies and algorithms that allow for accurate, intraoperative measurements.
LRIs have less predictability and efficacy compared to toric lenses, but they can be used effectively in patients with lower levels of astigmatism.
Clear corneal incision placement on the steepest meridian is the least expensive option for patients with low levels of astigmatism. However, smaller phaco incisions have made this option less effective since only small amounts of astigmatism can be corrected.
Two-stage procedure with excimer laser ablation is a good option for treating residual astigmatism and spherical error post cataract surgery, however the cost can be prohibitive.
References
- ↑ Shankar S, Bobier WR. Corneal and Lenticular Components of Total Astigmatism in a Pre-school Sample. Invest Ophthalmol Vis Sci. December 2002.
- ↑ Hashemi H,Fotouhi A, Yekta A, Pakzad R, Ostadimoghaddam H, Khabazkhoob M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. Journal of Current Ophthalmology. 2018;30(1):3-22. doi:10.1016/j.joco.2017.08.009
- ↑ 3.0 3.1 3.2 Anderson DF, Dhariwal M, Bouchet C, Keith MS. Global prevalence and economic and humanistic burden of astigmatism in cataract patients: a systematic literature review. Clin Ophthalmol. 2018;12:439-452. doi:10.2147/OPTH.S146829
- ↑ 4.0 4.1 4.2 4.3 4.4 Sigireddi RR, Weikert MP. How much astigmatism to treat in cataract surgery. Curr Opin Ophthalmol. 2020;31(1):10-14. doi:10.1097/ICU.0000000000000627
- ↑ 5.0 5.1 5.2 5.3 Sinjab MM. Introduction to astigmatism and corneal irregularities. In: Sinjab MM, Cummings AB, eds. Customized laser vision correction. Cham: Springer International Publishing; 2018:1-64. doi:10.1007/978-3-319-72263-4_1
- ↑ 6.0 6.1 American Academy of Ophthalmology (AAO). Corneal topography and astigmatism. https://store.aao.org/basic-and-clinical-science-course-section-13-refractive-surgery.html Accessed 25 September 2024.
- ↑ 7.0 7.1 Anderson D. Understanding Corneal Topography. Paraoptometric Resource Center.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Núñez MX, Henriquez MA, Escaf LJ, et al. Consensus on the management of astigmatism in cataract surgery. Clin Ophthalmol. 2019;13:311-324. doi:10.2147/OPTH.S178277
- ↑ 9.0 9.1 Goggin M, van Zyl L, Caputo S, Esterman A. Outcome of adjustment for posterior corneal curvature in toric intraocular lens calculation and selection. J Cataract Refract Surg. 2016;42(10):1441-1448. doi:10.1016/j.jcrs.2016.10.004
- ↑ 10.0 10.1 10.2 10.3 10.4 Mohammad-Rabei H, Mohammad-Rabei E, Espandar G, et al. Three Methods for Correction of Astigmatism during Phacoemulsification. J Ophthalmic Vis Res. 2016;11(2):162-167. doi:10.4103/2008-322X.183924
- ↑ 11.0 11.1 Toric IOLs - EyeWiki. https://eyewiki.aao.org/Toric_IOLs. Accessed April 27, 2020.
- ↑ Davison JA, Makari S, Potvin R. Clinically relevant differences in the selection of toric intraocular lens power in normal eyes: preoperative measurement vs intraoperative aberrometry. Clin Ophthalmol. 2019;13:913-920. doi:10.2147/OPTH.S205352
- ↑ Solomon KD, Sandoval HP, Potvin R. Correcting astigmatism at the time of cataract surgery: Toric IOLs and corneal relaxing incisions planned with an image-guidance system and intraoperative aberrometer versus manual planning and surgery. J Cataract Refract Surg. 2019;45(5):569-575. doi:10.1016/j.jcrs.2018.12.002
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 Brinton J, Oetting T. Phacoemulsification: Considerations for Astigmatism Management. EyeRounds.org. https://eyerounds.org/tutorials/phaco-astigmatism-management.htm. Published June 2011. Accessed April 27, 2020.
- ↑ 15.0 15.1 Mingo-Botín D, Muñoz-Negrete FJ, Won Kim HR, Morcillo-Laiz R, Rebolleda G, Oblanca N. Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg. 2010;36(10):1700-1708. doi:10.1016/j.jcrs.2010.04.043
- ↑ Pineda R, Denevich S, Lee WC, Waycaster C, Pashos CL. Economic evaluation of toric intraocular lens: a short- and long-term decision analytic model. Arch Ophthalmol. 2010;128(7):834-840. doi:10.1001/archophthalmol.2010.127
- ↑ 17.0 17.1 17.2 Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric Intraocular Lenses in the Correction of Astigmatism During Cataract Surgery: A Systematic Review and Meta-analysis. Ophthalmology. 2016;123(2):275-286. doi:10.1016/j.ophtha.2015.10.002
- ↑ Vukich J. Magnitude, axis of astigmatism vital to toric IOL alignment, but no consensus on best measure. Ophthalmology Times. https://www.ophthalmologytimes.com/modern-medicine-feature-articles/magnitude-axis-astigmatism-vital-toric-iol-alignment-no-consensus-best-measure. Accessed April 30, 2020.
- ↑ 19.0 19.1 19.2 19.3 Limbal Relaxing Incisions - EyeWiki. https://eyewiki.aao.org/Limbal_Relaxing_Incisions. Accessed April 27, 2020.
- ↑ 20.0 20.1 20.2 20.3 20.4 Johnson & Johnson Vision. Limbal Relaxing Incision Calculator . LRIcalculator.com. https://www.lricalculator.com/. Published 2017. Accessed April 27, 2020.
- ↑ 21.0 21.1 American Academy of Ophthalmology (AAO). Management of Astigmatism in Lens-Based Surgery: Intraoperative Treatment Options. Focal Points - Excerpt. https://www.aao.org/education/focalpoints Accessed 25 September 2024.
- ↑ 22.0 22.1 22.2 Agarwal A, Jacob S. Current and effective advantages of femto phacoemulsification. Curr Opin Ophthalmol. 2017;28(1):49-57. doi:10.1097/ICU.0000000000000333
- ↑ Lee JA, Song WK, Kim JY, Kim MJ, Tchah H. Femtosecond laser-assisted cataract surgery versus conventional phacoemulsification: Refractive and aberrometric outcomes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2019;45(1):21-27. doi:10.1016/j.jcrs.2018.08.032
- ↑ 24.0 24.1 Kaufmann C, Peter J, Ooi K, et al. Limbal relaxing incisions versus on-axis incisions to reduce corneal astigmatism at the time of cataract surgery. J Cataract Refract Surg. 2005;31(12):2261-2265. doi:10.1016/j.jcrs.2005.08.046
- ↑ 25.0 25.1 25.2 Ngoei E. Fixing astigmatism: Toric lens or LRI? EyeWorld. https://www.eyeworld.org/article-fixing-astigmatism--toric-lens-or-lri. Accessed April 27, 2020.
- ↑ 26.0 26.1 Masket S, Wang L, Belani S. Induced astigmatism with 2.2- and 3.0-mm coaxial phacoemulsification incisions. J Refract Surg. 2009;25(1):21-24. doi:10.3928/1081597X-20090101-04
- ↑ Jin GJC, Merkley KH, Crandall AS, Jones YJ. Laser in situ keratomileusis versus lens-based surgery for correcting residual refractive error after cataract surgery. J Cataract Refract Surg. 2008;34(4):562-569. doi:10.1016/j.jcrs.2007.11.040
- ↑ EyeWiki. Physiology of Astigmatism. https://eyewiki.aao.org/Physiology_of_Astigmatism. Accessed May 1, 2020.
- ↑ Goto T, Klyce SD, Zheng X, Maeda N, Kuroda T, Ide C. Gender- and age-related differences in corneal topography. Cornea. 2001;20(3):270-276. doi:10.1097/00003226-200104000-00007
- ↑ 30.0 30.1 30.2 Brennan K. Astigmatism: How Low Can You Go? Review of Ophthalmology. https://www.reviewofophthalmology.com/article/astigmatism-how-low-can-you-go. Published October 2018. Accessed May 1, 2020.
- ↑ Binder S. How to interpret your toric IOL biometry. EyeWorld.https://www.eyeworld.org/article-how-to-interpret-your-toric-iol-biometry. Published June 2015. Accessed April 28, 2020.
- ↑ 32.0 32.1 32.2 Beheregaray S, Goggin M, LaHood B. Astigmatic overcorrection and axis flip for targeting minimal remaining refractive astigmatism with toric intraocular lenses. J Cataract Refract Surg. 2018;44(1):109-110. doi:10.1016/j.jcrs.2017.11.004
- ↑ Leube A, Ohlendorf A, Wahl S. The influence of induced astigmatism on the depth of focus. Optom Vis Sci. 2016;93(10):1228-1234. doi:10.1097/OPX.0000000000000961