Limbal Relaxing Incisions
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Entity
Limbal Relaxing Incisions (LRI) are partial thickness incisions made at the corneal periphery for the treatment of corneal astigmatism. LRIs are considered to fall under the spectrum of incisional astigmatism treatments known as Corneal Relaxing Incisions (CRIs). Within this category, arcuate (or sometimes, "astigmatic") keratotomy (AK) can also be included. This latter term generally refers to astigmatic incisions in the cornea that are placed in closer proximity to the visual axis compared to the peripheral placement of LRIs.
Definition of Corneal Astigmatism
Abnormal curvature of the cornea with at least two axes of steeper and flatter curvature, which can result in abnormal focusing of light and impaired vision. Astigmatism typically results from curvature abnormalities of the front (anterior) surface of the cornea. Visit EyeSmart from the American Academy of Ophthalmology for a brief, patient-friendly description of astigmatism.
Classification of Astigmatism
Astigmatism may also be classified as regular and irregular.
Regular
- With-the-rule: Steep axis of the cylinder is within 15 degrees of the 90 degree vertical meridian (75 - 105 degrees)
- Against-the-rule: Steep axis of the cylinder is within 15 degrees of the horizontal meridian (165 - 015 degree)
- Oblique: Steep axis of the cylinder is not within 15 degrees of the horizontal or vertical meridians (16-74 degrees and 106-164 degrees)
Irregular
- Whenever the two main axes of astigmatism are not symmetric and/or do not lie 90 degrees apart (orthogonal), the astigmatism is considered irregular. Causes of irregular astigmatism include corneal dystrophy or degeneration, ocular surface disease, corneal ectatic disease such as keratoconus, or prior corneal surgery.
Diagnosis
History
The patient may present with a long history of astigmatism. Astigmatism, similar to myopia (nearsightedness) or hyperopia (farsightedness), is generally present and correctable at a young age with spectacles or contact lenses. In adults, astigmatism can also be corrected surgically with LASIK, PRK, SMILE, or limbal relaxing incisions (LRI).
Preoperative examination
Important items to note in the preoperative exam include:
- Close examination of the peripheral cornea, particularly in the areas where the incsions will be placed.
- Precise manifest refraction
- Keratometry to confirm diopters of corneal astigmatism
- Corneal topography to confirm axis of corneal astigmatism, and to classify as regular or irregular, symmetric or asymmetric
- Pachymetry at planned incision sites if possible
- Corneal Tomography (Orbscan, Pentacam, Galilei) may be considered
Signs
At least two distinct retinoscopic reflexes in different axes
Symptoms
The most common symptom is decreased visual acuity. The patient might notice that straight lines are not straight. Patients with even small amounts of cylinder may notice halos, glare and shadowing, especially in low light conditions and at distance.
Clinical diagnosis
Astigmatism is also measured during refraction. However, this measurement may include corneal and lenticular astigmatism. Therefore, this measurement cannot be used solely for determination of AK procedures. The next step is to determine how much of the measured astigmatism is a result of corneal irregularity.
Diagnostic procedures
Corneal astigmatism power and axis can be measured in many different ways, including the following:
- Keratometry: Manual Keratometer, Automated Keratometer, IOL Master
- Corneal Topography (Placido-disc based)
- Corneal Tomography (Scanning Slit or Scheimpflug imaging)
Management
Surgical Planning
Defining the astigmatism
The goal of astigmatism management is to leave the patient with as little astigmatism as possible. Some patients can tolerate up to 1.0 diopter in any axis and still maintain 20/40 vision at distance and J1 at near. Typically, with-the-rule and against-the-rule astigmatism are better tolerated than oblique astigmatism.
The most crucial element of surgical planning for astigmatic keratotomy is determining the amount and location of the astigmatism to be corrected. This is also perhaps the most difficult aspect of this procedure. As mentioned above, preoperative astigmatism measurements are done in several ways. It is common for many surgeons to rely on manual keratometry as their measurement; however many use either corneal topography or Scheimpflug imaging. It is important to remember that the manual refraction may include any lenticular-induced cylinder as well, so often times the refraction will be misleading. The manual keratometry axis of astigmatism should match the topographical or Scheimpflug axis.
If the preoperative cylindrical values or axis vary with the several methods of measurements, the surgeon may opt to correct the astigmatism after the postoperative refraction has stabilized. Some surgeons opt to 'split the difference' (ie. 2 diopters @ 90 degrees on IOL master K's and 1 diopter @ 90 degrees on topography, the surgeon may treat 1.5 diopters.)
Choosing the procedure
Corneal Relaxing Incisions (CRIs) can be divided into 2 groups: limbal relaxing incisions (LRIs) and arcuate keratotomy (AK). The surgeon must evaluate the pros and cons of each in conjunction with the needs of each individual patient.
The pros of LRIs include:
- Easier to perform, less dependent on pachymetry, less likely to result in overcorrections, quicker post-op stabilization of refraction, postoperative topography is smoother/more homogenous (coupling).
- LRIs are best for low to moderate amounts of astigmatism (< 3 diopters).
The cons of LRIs include:
- A larger incision (typically one or two incisions 1-3 clock hours in arc length)
The pros of AKs include:
- Shorter incision, more powerful (correct a larger amount of astigmatism), placement in smaller optical zone (therefore low coupling ratio), 'multifocal' effect (better depth of focus)
The cons of AKs are:
- More discomfort, greater risk of corneal perforation (more dependent on accurate pachymetry), may cause more corneal irregularity and irregular astigmatism
- AKs have been noted to have a higher risk of overcorrection so they are more often performed on patients with higher amounts of astigmatism.
- AKs may also risk a loss of best-corrected spectacle acuity
Relative Contraindications for CRIs
- Keratoconus
- Autoimmune disease
- Peripheral corneal disease
- Terrien's or furrow degeneration
- Prior corneal surgery, particularly incisional procedures
Other considerations
Either LRIs or AK may be used in conjunction with toric intraocular lenses (IOLs) and strategic cataract incision placement to treat high astigmatism.
Astigmatism may also be managed with Toric IOLs alone.
The surgeon should consider the age of the patient as the effect of the relaxing incision have been found to increases with age.
A simple breakdown of treatment options
Astigmatism less than 1.0 diopter can typically be adequately treated with CRIs.
Astigmatism ranging from 1.0 diopter to 3.0 diopters can be corrected with a toric IOL or CRIs, although toric IOLs are regarded to give more reliable results.
Astigmatism greater than 3.0 diopters may corrected with a combination of toric IOL or CRIs and/or strategic cataract incision placement.
The surgeon may opt to utilize an online calculator (See Additional Resources section below for link) for guidance. Online LRI calculator results are based on the preoperative keratometry measurements and anticpated surgeon induced astigmatism.
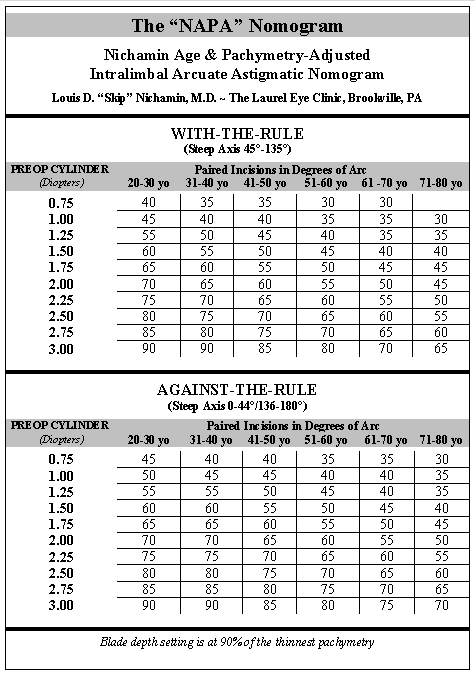
Many surgeons have developed nomograms. Table 1 is a representative nomogram. (Courtesy of Louis D. "Skip" Nichamin, M.D.)
Surgery
Corneal relaxing incisions may be done independently or in conjunction with cataract surgery.
CRIs may be done manually with a set-depth blade or by using a femtosecond laser. A comparative study found that both femtosecond and manual CRIs were effective in reducing astigmatism, but that manual CRIs tended to undercorrect astigmatism relative to femtosecond CRIs[1]. A systematic review similarly concluded that both femtosecond and manual CRIs were safe and moderately effective for treating corneal astigmatism during cataract surgery. The authors also noted that both methods have similar visual and refractive outcomes, despite the increased precision and greater cost of femtosecond CRIs. [2]
Treatment Planning
The first step of surgery is treatment planning. Nomograms are widely available for planning CRI depth, length, location, and number. Ideally, each surgeon develops their own by monitoring their outcomes. Surgeons may elect to use an existing nomogram (such as those reviewed in this article) as a starting point.
Manual CRIs
Manual CRIs may done independently or in conjunction with cataract surgery.
When done in conjunction with cataract surgery, beginning surgeons may find it easiest to perform CRIs at the beginning of the case when the eye is still firm.
Prior to draping, with the patient in a sitting position, the cornea is marked. There are many strategies for marking the cornea such as 3:00 and 9:00, or 12:00 and 6:00. Most CRI corneal marking sets have an instrument designed for making preoperative orientation marks.
A diamond knife is most commonly utilized for the CRI incision. Disposable and reusable, metal CRI knives are also available. Both often have preset depths for surgeon convenience. The usual depth is 600 microns but may range from 450 to 650 microns. It is helpful to have handy a print out of the patient's topography and/or CRI calculator print out to ensure appropriate orientation of the CRI. An arc-shaped incision is made in the clear cornea close to the limbus (approximately 0.5 mm). The episclera is grasped with 0.12 forceps. The arc incision is drawn towards the surgeon for best control. It is important to press the CRI blade firmly against the cornea to ensure consistent depth of the incision and to create the incision with one pass to avoid irregularities.
Depending the amount of astigmatism to be corrected, paired incisions may be employed. For asymmetrical regular astigmatism, the paired incisions may be different lengths, greater in the axis with the larger amount of cylinder.
Alternatively, some surgeons prefer to do the CRI upon completion of the cataract surgery.
Femtosecond Laser CRIs
CRIs may be done by 'Femtosecond Lasers' as part of femtosecond laser-assisted cataract surgery (FLACS). The laser can be used to create the capsulotomy, side-port, and main incisions, and assist in nuclear fragmentation. The surgeon can elect to have laser-created astigmatic keratotomies at the time of the procedure as well. Pre-operative planning may be done with the aid of a nomogram, which differs from the manual CRI nomogram. One such nomogram is the Lindstrom nomogram.[3] CRIs done with the femtosecond laser may be opened at the time of surgery or opened post-operatively to titrate the patient's astigmatic correction.
Adjunctive Technologies
Alcon ORA system Intraoperative Aberrometer utilizes Talbot-Moire's interferometry, a form of wavefront analysis which has a dynamic range of -20 to +20 D. The device is attached to the surgical microscope. At any point in the surgery, the ophthalmologist may take a measurement. The monitor will display the refractive error of the eye. Surgeons who have this technology available in their operating room are able to complete the cataract extraction portion of the procedure. Intraoperative measurements are taken and the appropriate lens and ancillary techniques (LRIs or CRIs/AKs) can be employed. Alternatively, this diagnostic tool may be used to confirm preoperative calculations.
Surgical follow up
Postoperative follow up should be per routine for cataract surgery when done together. Manifest refractions should be performed. Postoperative corneal topography is also helpful to identify treatment effect.
Complications
Possible complications of CRIs include infection, overcorrection, undercorrection, perforation of the cornea, induced astigmatism, discomfort and decreased corneal sensation.
Overcorrection: Wait for the refraction to stabilize. The incision may be cleaned (with Sinskey hook or similar instrument). Then the wound is sutured with a 10-0 nylon. Placing CRIs perpendicular to the original incisions may induce irregular astigmatism so this method of correction is discouraged.
Undercorrections may be corrected by enlarging the original incision.
Incisions should be examined carefully at time of placement for corneal perforation. If a perforation is noted, it should be sutured with a 10-0 nylon if it is not self-sealing. This will limit the effect of the procedure, but the suture may be removed several weeks later and the effect of the CRI should be apparent after suture removal.
Prognosis
The vast majority of patients do exceedingly well. Even routine cataract surgeries are transitioning into 'refractive' procedures. As patient expectations for improved refractive outcomes increase, cataract surgeons will find CRIs are a useful and easy to master tool to achieve optimal postoperative results.
Additional Resources
- AMO online LRI calculator:
- EyeLRI.com
- Boyd K, Mendoza O, Turbert D. What Is Astigmatism? Symptoms, Causes, Diagnosis, Treatment. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/astigmatism-4. Accessed March 03, 2023.
References
- ↑ Roberts HW, Wagh VK, Sullivan DL, Archer TJ, O'Brart DPS. Refractive outcomes after limbal relaxing incisions or femtosecond laser arcuate keratotomy to manage corneal astigmatism at the time of cataract surgery. J Cataract Refract Surg. Aug 2018;44(8):955-963. doi:10.1016/j.jcrs.2018.05.027
- ↑ González-Cruces T, Cano-Ortiz A, Sánchez-González MC, Sánchez-González JM. Cataract surgery astigmatism incisional management. Manual relaxing incision versus femtosecond laser-assisted arcuate keratotomy. A systematic review. Graefes Arch Clin Exp Ophthalmol. Nov 2022;260(11):3437-3452. doi:10.1007/s00417-022-05728-0
- ↑ 1. Vickers LA, Gupta PK. Femtosecond laser-assisted keratotomy. Curr Opin Ophthalmol. Jul 2016;27(4):277-84. doi:10.1097/ICU.0000000000000267