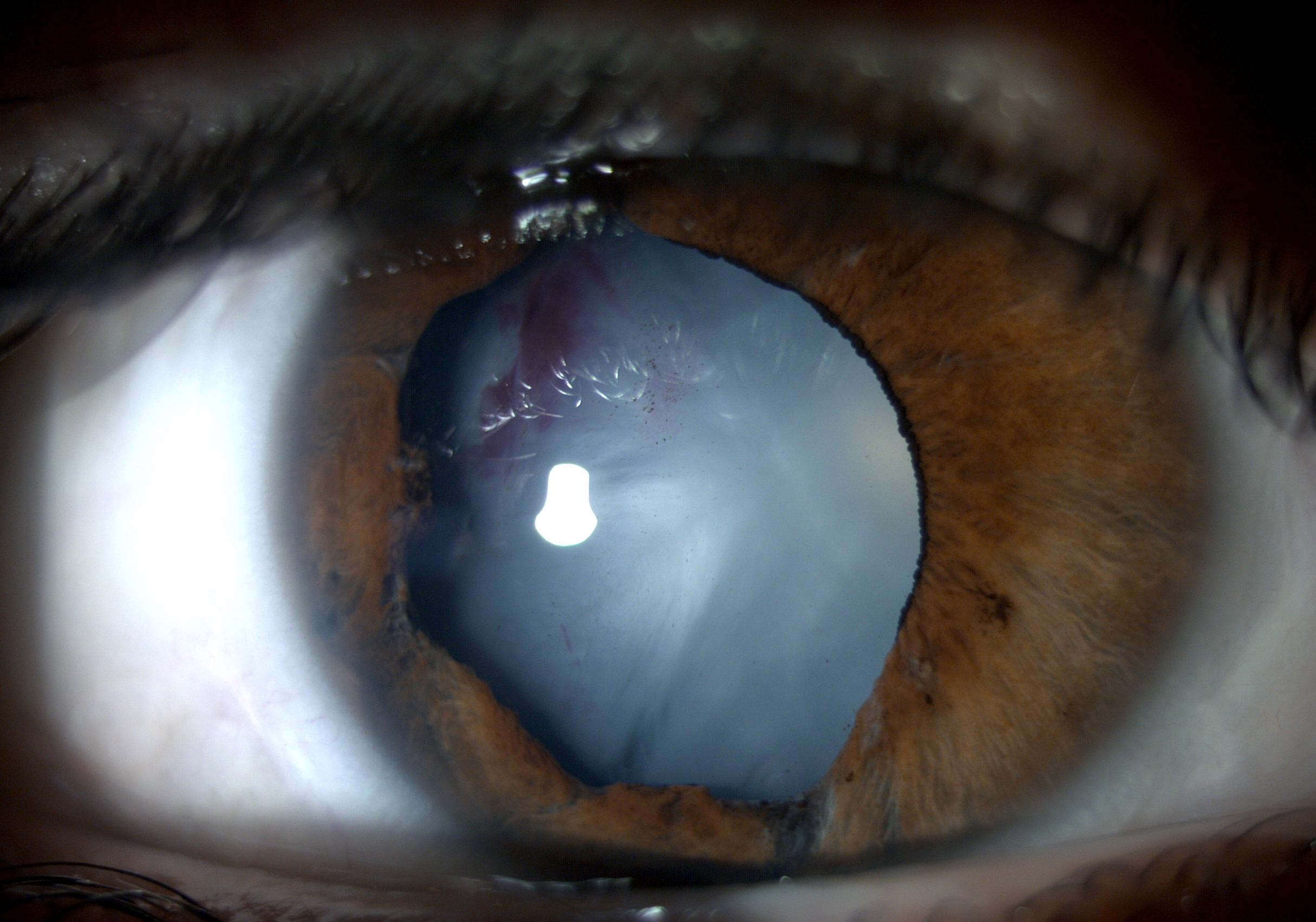
White Cataract
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Cataract is defined as the opacification of the natural crystalline lens. Cataracts are mainly age-related, but may also occur secondary to other causes such as uveitis, trauma, medications, and metabolic diseases as described elsewhere.[1]If left untreated in the long-term, a cataract may advance to become an opaque, mature cataract, often causing extreme visual impairment. . Mature, totally opaque cataracts prevent the organized transmission of light to the retina, rendering the patient completely blind in the affected eye.[2] Mature cataracts can either be dark, such as brown or black, or white. This article will focus on the white cataract subtype. When a white cataract is termed “intumescent”, it is defined as having swelling of the lens because of epithelial impairment and fluid influx, leading to rapid decline in visual function.[3]Given its surgical challenges, it is important to recognize these types of cataracts in order to achieve better outcomes during surgery.[4]
Epidemiology
The normal history of a cataract evolves from lens changes that are minuscule (incipient), immature, intumescent, mature corticonuclear, hypermature Morgagnian, and in its most extreme form, shrunken Morgagnian. Patients usually present when they either have incipient or immature cataracts, so it is relatively rare to see senile intumescent and more severe forms of cataract such as white cataract.[5]it’s higher prevalence in low socioeconomic communities reflects poor or limited access to care.[4]A study in India found that 8% of the total 3634 patients present with white cataract.[4]
Etiologies
Many causes can lead to senile white/intumescent cataracts including:
- Exposure to:
- Long radiation,
- UV rays,
- Heatwaves,
- Infrared lights
- Rupture of the eye [6]
Risk Factors
Notable risk factors include:
- Large EtOH consumption,
- Smoking,
- History of other eye conditions,
- Chronic use of steroid therapies,
- History of radiation treatment,
- UV sun exposure without wearing sunglasses,[6]
- After the use of chemotherapy drugs like MMC,[7]
- After radial keratotomy, [8]
- Thalassemia.[9]
Pathophysiology
White cataracts are characterized as swollen as they are full of cortical material enveloping a hard nucleus. They have weak zonular fibers and fragile capsules.[10] Intumescent cataracts are a type of mature cortical cataract and follow the same pathophysiological progression. In this type, the structure of the mature lens fiber cells is interrupted, leading to loss of the membrane integrity. Lens metabolism is altered that includes loss of lens protective metabolites or alteration of protease activity and other enzymatic activity resulting in protein oxidation and precipitation. In intumescent white cataracts, the swelling of the lens occurs because of accumulation due to lens epithelial cell dysfunction related to protein changes in the Na+-K+ ATPase pump.[11] [12] While the level of calcium is elevated in all cataractous lenses, changes in expression of different Ca2+-ATPase isoforms plays a major role in white cataract formation.[12] Dysfunction of these pump systems may result in the osmotic pressure changes which do not normally occur in nuclear cataracts.[3] On slit-lamp biomicroscopy, the first sign of these cataracts is the presence of vacuoles with cortical spokes/cuneiform opacities (appear white in slit-lamp biomicroscopy, while in retro-illumination they are brown) that can appear in progressed cases. These cortical spokes can spread to adjacent fibers and cover the whole of the capsule, in which case the cataract is classified as mature/intumescent cortical cataract. In these cases, the entire cortex from the nucleus to the capsule adopts a white color. If there is leakage of cortical material in the lens capsule, it makes the capsule appear shrunken and wrinkled, which is then termed a hypermature cataract. If this liquefaction persists and leads to such significant loss of material in the capsule that the nucleus is no longer stabilized, then the nucleus floats around freely in the capsular bag, constituting a Morgagnian cataract.[10] Although, the typical presentation may be due to senile intumescent cataract, it can also present in the younger population due to underlying systemic diseases such as diabetes mellitus (producing snowflake cortical opacities), myotonic dystrophy (Christmas tree cortical cataract that can evolve to appear like a star), atopic dermatitis (shield-appearing dense anterior subcapsular plaques), and neurofibromatosis type 2.[13] If the pupil of the eye affected by cataract is black, then that suggests the presence of a cataract nigra (black cataract).[5] Intumescent cataracts have vacuoles which can present with severe vision impairment esp. when compared to brunescent (brown) cataracts which have good vision especially at near.[10]
Classification
There are many classifications systems that have been described in the literature from the characterization of the white cataract preoperatively on slit-lamp biomicroscopy or A-scan and, more recently, intra-operative OCT classification.[14] The first classification involves looking at three factors with the use of a standardized method of biomicroscopy: intra-lenticular pressure, the status of the cortex, and color of the nucleus of the lens. If the intra-lenticular pressure is increased, it is classified as intumescent. If the status of the cortex is milky, it is characterized as hypermature.[14] The second classification uses A-scan ultrasonography and categorizes white cataracts into three types. Type 1 is characterized by intumescence with cortex liquefaction and high internal acoustic reflections. Type 2 is characterized by voluminous nuclei, low acoustic reflections, and a small amount of whitish solid cortex. Type 3 has a fibrosed anterior capsule with low internal echospikes.[15]
The third classification system and the newest one to have been published stratifies white cataracts into 4 types based on morphology and intraoperative dynamics on OCT. Type 1 has lamellar cortical fibers that exhibit minimal intra-lenticular clefts and no elevation in the convexity of the anterior lens capsule. Type 2 has increased convexity of the anterior lens capsule with hyperreflective bundles of cortical fibers and is associated with increased intra-lenticular pressure. Type 3 has a convex anterior lens capsule with swollen hyperreflective bundles of cortical fibers and intra-lenticular clefts that have hydrated intumescent cortical fibers with elevated intra-lenticular pressure. Type 4 has a convex anterior lens capsule with a homogenous ground-glass looking anterior lens cortex representing complete liquefaction of the anterior lens cortex.[14]
Management
White cataracts present a high risk for complications even in experienced surgeons. One of the greatest challenges in managing a white cataract is the creation of a continuous circular capsulorhexis (CCC).[10] Studies have shown that capsulorhexis that was not totally successful in the management of white cataract may be observed in 3.85% to 28.3% of cases with an increased incidence of posterior capsular rupture and vitreous loss.[15][16] These difficulties are mainly driven by two factors. First, the high lens density results in poor visibility given loss of red reflex making it difficult to differentiate the edge of the anterior capsule from the white lens matter.[17] This can be partially mitigated by using trypan staining dye, but is still worse than the visibility provided when a red reflex is present. Second, the raised intralenticular pressure causes liquified cortex escape as soon as the capsule is compromised which results in capsular tears extending to the periphery in addition to making visibility even worse.[18] Depending on the classification, different surgical techniques may be advised. As the OCT-based classification system was the most common, the treatments discussed will be based on those subtypes. For Type I, it is advised that the surgeon uses a single-stage forceps/needle cystotome capsulorhexis. For Type 2, the forceps-assisted 2-stage capsulorhexis technique should be used followed by bimanual irrigation and aspiration to lower the elevated intra-lenticular pressure. For Type 3, aspiration of the turbid fluid with needle aspiration and forceps-assisted capsulorhexis should be used. For the last type, anterior chamber decompression is needed to take out the milky fluid present with forceps-assisted capsulorhexis.[14]
References
- ↑ Feldman MD B, Heersink MD S. Cataract - EyeWiki. Eyewiki.org. https://eyewiki.org/Cataract. Accessed January 16, 2022.
- ↑ Devgan MD U. Understanding subtypes key to removing white cataracts. Healio.com. https://www.healio.com/news/ophthalmology/20121122/10_3928_1081_597x_20120101_01_953476. Published 2012. Accessed January 16, 2022.
- ↑ Jump up to: 3.0 3.1 Brown N, Bron A. Lens disorders. Oxford: Butterworth-Heinemann; 1996.
- ↑ Jump up to: 4.0 4.1 4.2 Rewri P, Lohan A, Aggarwal S, Chodhary P, Singhal A. Cataract surgical reach: Falling short to catch white cataracts!. Indian J Ophthalmol. 2021;69(6):1575. doi:10.4103/ijo.ijo_2560_20
- ↑ Jump up to: 5.0 5.1 Intumescent cataract. EyeRounds.org: Online Ophthalmic Atlas. Webeye.ophth.uiowa.edu. https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/intumescent-cataract.html. Published 2022. Accessed January 21, 2022.
- ↑ Jump up to: 6.0 6.1 Intumescent Cataract - Symptoms, Causes, Diagnosis, Treatment & Prevention. Dr. Agarwals. https://www.dragarwal.com/diseases-conditions/cataract/intumescent-cataract/. Published 2022. Accessed January 21, 2022.
- ↑ Sacu S, Ségur-Eltz N, Horvat R, Lukas J, Zehetmayer M. Intumescent cataract after topical mitomycin-C for conjunctival malignant melanoma. Am J Ophthalmol. 2003;136(2):375-377. doi:10.1016/s0002-9394(03)00207-1
- ↑ Gelender H, Gelber E. Cataract Following Radial Keratotomy. Archives of Ophthalmology. 1983;101(8):1229-1231. doi:10.1001/archopht.1983.01040020231014
- ↑ Athanasiadis I, Konstantinidis A, Kyprianou I, Robinson R, Moschou V, Kouzi-Koliakos K. Rapidly progressing bilateral cataracts in a patient with beta thalassemia and pellagra. J Cataract Refract Surg. 2007;33(9):1659-1661. doi:10.1016/j.jcrs.2007.05.011
- ↑ Jump up to: 10.0 10.1 10.2 10.3 American Academy of Ophthalmologists Basic Science & Clinical Science Book Lens & Cataract
- ↑ Hightower K. The role of the lens epithelium in development of UV cataract. Current Eye Research. 1995;14(1):71-78.
- ↑ Jump up to: 12.0 12.1 Delamere N, Tamiya S. Expression, regulation and function of Na,K-ATPase in the lens. Progress in Retinal and Eye Research. 2004;23(6):593-615.
- ↑ Nizami A, Gulani A. Cataract. Ncbi.nlm.nih.gov. https://www.ncbi.nlm.nih.gov/books/NBK539699/. Published 2022. Accessed January 21, 2022.
- ↑ Jump up to: 14.0 14.1 14.2 14.3 Titiyal J, Kaur M, Shaikh F, Goel S, Bageshwar L. Real-time intraoperative dynamics of white cataract—intraoperative optical coherence tomography–guided classification and management. J Cataract Refract Surg. 2020;46(4):598-605. doi:10.1097/j.jcrs.0000000000000086
- ↑ Jump up to: 15.0 15.1 Brazitikos P, Tsinopoulos I, Papadopoulos N, Fotiadis K, Stangos N. Ultrasonographic classification and phacoemulsification of white senile cataracts. Ophthalmology. 1999;106(11):2178-2183. doi:10.1016/s0161-6420(99)90502-x
- ↑ Jacob S, Agarwal A, Agarwal A, Agarwal S, Chowdhary S, Chowdhary R, Bagmar AA. Trypan blue as an adjunct for safe phacoemulsification in eyes with white cataract. J Cataract Refract Surg 2002;28:1819–1825
- ↑ Jain A, Balyan M, Malhotra C, Ram J, Dhingra D. Achieving successful capsulorhexis in intumescent white mature cataracts to prevent Argentinian flag sign - A new multifaceted approach to meet the challenge. Indian Journal of Ophthalmology. 2021;69(6):1398.
- ↑ Gimbel HV, Willerscheidt AB. What to do with limited view: the intumescent cataract. J Cataract Refract Surg. 1993 Sep;19(5):657-61. doi: 10.1016/s0886-3350(13)80021-1. PMID: 7980732.
- Marian MJ, Mukhopadhyay P, Borchman D, Paterson CA (2008) Plasma membrane Ca-ATPase isoform expression in human cataractous lenses compared to age-matched clear lenses. Ophthalmic Res 40:86–93
- Basti S. Different faces of the white cataract: A phaco surgeonâs perspective. Aust N Z J Ophthalmol. 1999;27(1):53-56. doi:10.1046/j.1440-1606.1999.00150.x
- Chakrabarti A, Singh S. Phacoemulsification in eyes with white cataract. J Cataract Refract Surg 2000;26:1041–1047