Arlt's Triangle
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
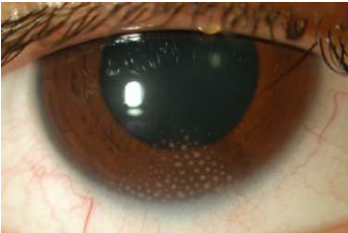
Arlt's triangle is a clinical sign indicative of granulomatous uveitis.[1]
Disease Entity
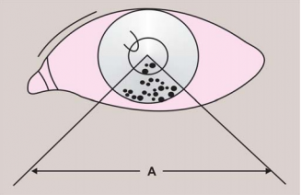
Arlt's triangle is a distribution pattern of mutton-fat keratic precipitates, which deposit as an inverted triangle on the central to inferior cornea , forming a wedge-shaped region on the inferior corneal endothelium.[2] The white-yellowish greasy precipitates of inflammatory cells (macrophages and epithelioid cells) are clumped in triangular fashion in the lower part of the anterior chamber[1] due to gravity and convection current. It is a clinical sign characteristic of granulomatous inflammation in the anterior chamber and is commonly found in several types of anterior uveitis. Arlt’s triangle distribution is a general finding and not suggestive of any specific uveitis etiology.[2]
History
Arlt's triangle is named after Carl Ferdinand Ritter von Arlt (1812-1887) , an Austrian ophthalmologist who was also the first physician to prove that myopia is a consequence of excessive axial length of the eye.[3]
Etiology
Arlt's triangle distribution pattern of mutton fat keratic precipitates is suggestive of chronic granulomatous inflammatory process. [4] The differential diagnosis should include anterior uveitis associated with sarcoidosis, syphillis, and tuberculosis. Clusters of large, fluffy, lardaceous KPs with greasy appearance forming Arlt's triangle may also occur in other unusual chronic infections e.g. leprosy, brucellosis, coccidiomycosis.[4]
Pathophysiology
Arlt's triange distribution occurs as a result of convection currents within the anterior chamber and the cooler temperature in the inferior cornea. [5][6]The larger granulomatous KPs will pigment and then shrink as inflammation abates or is controlled by steroid therapy.[5] They often fail to disappear completely, and they may alter the endothelium where they rest, leaving a halo on the endothelium.
Diagnosis
Clinical Diagnosis
Arlt's triangle sign is typically observed during slit-lamp biomicroscopy. The keratic precipitates forming an inverted ttriaon the inferior corneal endothelium can be visualized during slit-lamp examination in diffuse illumination, as well as direct focal illumination or an optic section.
However, in some cases, this collection of sticky inflammatory cells on the central and inferior cornea is so large in size, that it's visible with the naked eye.
Differential Diagnosis
Artl's triangle is suggestive, but not pathognomonic, of granulomatous inflammation. Differential diagnosis should also include unusual chronic inflammatory conditions including :
- Sarcoidosis
- Syphilis
- Tuberculosis
- Vogt-Koyanagi-Harada disease
- Sympathetic ophthalmia
- Lens-induced uveitis
- Brucellosis
- Lyme disease
- Leprosy
- Presumed ocular histoplasmosis syndrome (POHS)
- Toxocariasis
- Coccidioidomycosis (Valley Fever)
Diagnostic Work-Up
- Venereal Disease Research Laboratory (VDRL) test, FTA-ABS (or similar treponemal specific serology) test for syphilis A specific antitreponemal test must be obtained, as RPR or VDRL can provide false-negative results on RPR or VDRL.
- CBC with differential
- Angiotensin-converting enzyme (ACE) test for sarcoidosis may be obtained but is not very sensitive or specific, especially in children.
- Anergy evaluation for sarcoidosis (rarely done)
- Lyme serology if Lyme disease is suspected (eg, endemic area, tick bite, systemic manifestations)
- Toxoplasmosis enzyme-linked immunosorbent assay (ELISA) if posterior uveitis associated
- Antineutrophil cytoplasmic autoantibodies: c-ANCA with PR3 specificity is most specific for granulomatosis with polyangiitis (GPA; formerly Wegener's granulomatosis). c-ANCA is found in 80-95% of active cases. An isolated anterior uveitis (without orbital, scleral, or corneal involvement) is a very rare presentation of GPA.
- Cytology, polymerase chain reaction, and cultures of intra-ocular fluid when infection or masquerade suspected
- In cases of suspected acute retinal necrosis, anterior chamber fluid and/or vitreous should be examined via polymerase chain reaction (PCR) for HSV and herpes zoster virus nucleic acid.
Management
General treatment
Cycloplegia
Use a long-acting cycloplegic agent, such as cyclopentolate or homatropine, to relieve both pain and photophobia (if present) and to prevent the formation of posterior synechiae. However, this may not always be necessary in chronic disease, especially if the inflammation is well controlled. In any case, allowing for some pupil movement is helpful to prevent posterior synechiae formation in the dilated position.
Corticosteroids
- Topical corticosteroids are the mainstay of therapy and should be used aggressively during the initial phases of therapy.
- Subconjunctival injection of shorter-acting or depot steroids may be used if the patient poorly complies with topical therapy or if the inflammation is not responding to topical corticosteroids. Betamethasone (Celestone) is short and intermediate acting and can be used for exacerbations, whereas triamcinolone acetate is longer acting and is used more often for associated cystoid macular edema or vitritis. Depot steroids should be avoided in cases of uveitis secondary to any suspected infectious process because of their potentially severe adverse effects.
- Oral steroids in severe cases may be added to the treatment regimen (after ruling out the infectious etiology or after under coverage of medication, which treats the infectious etiology).
References
- ↑ 1.0 1.1 Mutton-fat keratic precipitates. Mutton-fat keratic precipitates | Columbia Ophthalmology. (n.d.). https://www.columbiaeye.org/education/digital-reference-of-ophthalmology/cornea-external-diseases/non-infectious/mutton-fat-keratic-precipitates.
- ↑ 2.0 2.1 Goldstein, D. A., Patel, S., & Tessler, H. H. (n.d.). Classification, Symptoms, and Signs of Uveitis. Ento Key. https://entokey.com/classification-symptoms-and-signs-of-uveitis/.
- ↑ Ernst Ziegler (1897). A text-book of special pathological anatomy. Macmillan. Retrieved 13 May 2012.
- ↑ 4.0 4.1 "Arlt's triangle." Millodot: Dictionary of Optometry and Visual Science, 7th edition. 2009. Butterworth-Heinemann 2 Jun. 2021 https://medical-dictionary.thefreedictionary.com/Arlt%27s+triangle
- ↑ 5.0 5.1 Atlas of Ophthalmology. Anterior Uveitis with Keratic Precipitates in Arlt's Triangle hppts://www.atlasophthalmology.net/folder.jsf;jsessionid=B7E3841DDE6D280139F29E4BD4F43F80?node=8816&locale=en.
- ↑ Sangwan, V. (2005). Ch. 159 : Clinical Approach to a Patient with Uveitis. In 1203454149 897930590 N. Dutta (Ed.), Modern Ophthalmology (3 Volumes) (3rd ed., Vol. 3, pp. 1263-1264). Aypee Brothers Medical (P). doi:https://doi.org/10.5005/jp/books/10535_160