Coccidioidomycosis (Valley Fever)
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Coccidioidomycosis is a systemic fungal disease that rarely presents with ocular manifestations. When present, ocular Coccidioidomycosis can affect any anatomic area of the eye. Due to the potentially devastating outcomes of this disease, there should be a high index of suspicion if a patient presents with systemic and/or pulmonary symptoms in the setting of ocular complaints, especially if the patient is immunocompromised or has recently traveled to areas in which the fungus is endemic. Ocular involvement can potentially be subclinical; thus, further evaluation should be considered in patients with pulmonary Coccidioidomycosis alone.[1] [2] Prognosis is guarded, especially with meningeal involvement; however, with prompt diagnosis via serology, skin testing, or biopsy, treatment with systemic and potentially intravitreal antifungals can be initiated to ideally prevent enucleation.
Disease
Coccidioidomycosis, or San Joaquin Valley Fever, is a systemic fungal disease with many potential clinical manifestations.[3] The condition results from the inhalation of spores of the Coccidioides species, which include C. immitis and C. posadasii.[3][4]
Etiology
Coccidioides species are endemic to southern Arizona, California, southern New Mexico, and west Texas.[5] Coccidioidomycosis infection is reportable to the CDC, and 15,611 cases were recorded in 2018, most of which occurred in these areas where the fungus is endemic.[6] True cases of Coccidioidomycosis may be underreported due to low testing rates. Ocular Coccidioidomycosis is uncommon and occurs in the setting of dissemination from the primary site of infection, most commonly the lung, making the incidence of this manifestation difficult to determine.[1]
Signs and Symptoms
Half to two-thirds of infections are subclinical, and if patients do experience symptoms, the most common presentation is self-limited pneumonia.[5] Extrapulmonary manifestations have been well-documented and are more commonly seen in immunocompromised patients. Coccidioidomycosis has been known to involve the skin, lymph nodes, and bones.
Ocular manifestations usually involve the anterior segment; however, both intraorbital and extraorbital diseases have been reported.[1] Anterior segment findings include phlyctenular conjunctivitis, granulomatous conjunctivitis, necrotic conjunctivitis, episcleritis, scleritis, and keratoconjunctivitis.[2][7] These findings are considered secondary to a hypersensitivity response and tend to co-occur with erythema nodosum.[1][8] Anterior chamber and iris nodules can be seen concomitantly with anterior uveitis.[7]
Intraocular findings include iridocyclitis, choroiditis, chorioretinitis, and endophthalmitis.[1][7] The uvea is the most commonly involved intraocular structure but rarely are both the anterior and posterior segments affected, rather, either the anterior or posterior segment is typically involved.[1][7][9] The iridocyclitis is granulomatous with "mutton fat" keratic precipitates.[7] There are several ways in which posterior involvement can present, including diffuse choroiditis sparing the retina, juxtapapillary chorioretinitis with hemorrhage, edema, and exudate, whitish-yellow opacities at Bruch's membrane with a propensity to involve the macula and posterior pole, and finally, peripheral chorioretinal scarring, more likely indicating inactive disease.
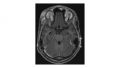
Extraocular findings include lid granulomas and inflammation, lesions of the orbit, optic nerve granulomas and atrophy, and cranial nerve paralysis.[1] Abducens nerve paralysis specifically has been seen as a complication of central nervous system coccidioidomycosis, likely secondary to increased intracranial pressure.[10] Figure 1 shows a magnetic resonance imaging (MRI) of osteomyelitis from Coccidioidomycosis in the superotemporal orbital rim.
Patient-reported symptoms of ocular Coccidioidomycosis depend on the involved anatomy, including redness, foreign body sensation, photophobia, lid inflammation, swelling, tearing, and floaters. Systemic symptoms suggestive of Coccidioidomycosis include fever, fatigue, shortness of breath, cough, chest pain, weight loss, headache, migratory arthralgias, maculopapular rash, and night sweats.[3] [6]
Diagnosis
Numerous options are available to diagnose Coccidioidomycosis, including serological testing, fungal cultures, and histopathology.[3][11] Skin testing is once again available in the United States since 2014.[6] Serological tests can be positive in patients exposed to the fungus without disease, and those with the disease may have negative serology. Thus, the utility of these tests is somewhat limited.[3] Early on during infection, these markers can be negative as well.[11] Tissue biopsy provides a definitive diagnosis, which would ideally be performed at extraocular locations, such as the skin if lesions are present. Aqueous and vitreous biopsies can be performed, as well as biopsies of iris nodules and chorioretinal biopsies; however, these are generally considered invasive.[7] Additional ophthalmologic testing is unlikely to assist in diagnosis aside from fluorescein angiography, which may help characterize retinal lesions.
Differential diagnosis
The differential will vary depending on the ocular manifestation of the disease.
Management
Treatment
In 2016, the Infectious Disease Society of America (IDSA) released clinical practice guidelines for the treatment of Coccidioidomycosis.[12] Treatment decisions are based on the severity of illness and whether the patient is immunocompromised. In general, options for systemic medical therapy include oral azoles and/or intravenous amphotericin B. No specific guidelines were given for ocular Coccidioidomycosis; however, given that the ocular manifestations are often present in the setting of dissemination, intravenous amphotericin B would likely be indicated, followed by maintenance azole therapy once stabilized. Itraconazole is not recommended for intraocular involvement as this agent does not cross the blood-eye barrier.[8] Fluconazole and voriconazole are preferred, as these agents have better ocular penetration.[13] Management should be done in consultation with an infectious disease specialist to determine regimens and length of therapy.[7] Intravitreal voriconazole and/or amphotericin B have been used successfully; however, amphotericin B carries a greater risk of retinal toxicity.[7][14]
Surgery
Vitrectomy is a consideration depending on the degree of vitreoretinal involvement.[7] [13]
Prognosis
Patient outcomes depend on the degree of ocular involvement, the involved structures, time to diagnosis, therapy initiation, initial visual acuity, and adherence to medical therapy.[7] Patients will likely receive long-term suppressive azole therapy to prevent relapses. Final visual acuity ranges from 20/20 to no light perception. Anterior segment coccidioidomycosis carries a worse prognosis than posterior segment involvement, with a significant proportion of those with anterior segment involvement requiring enucleation.[15]
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Rodenbiker H and Ganley J. Ocular coccidioidomycosis. Surv Ophthalmol. 1980; 24(5): 263-290.
- ↑ Jump up to: 2.0 2.1 Maguire LJ, Campbell RJ, and Edson, RS. Coccidioidomycosis with necrotizing granulomatous conjunctivitis. Cornea. 1994; 13(6): 539-542.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 Akram, SM and Koirala J. Coccidiomycosis. StatPearls. 2020. https://www.ncbi.nlm.nih.gov/books/NBK448161/. Accessed 30 November 2020.
- ↑ Galgiani JN., et al. Coccidioidomycosis. Clin Infect Dis. 2005; 41(9): 1217- 1223.
- ↑ Jump up to: 5.0 5.1 Blair, Janis E., et al. Characteristics of patients with mild to moderate pulmonary Coccidioidomycosis. Emerg Infect Dis. 2014; 20(6): 983-990.
- ↑ Jump up to: 6.0 6.1 6.2 Centers for Disease Control and Prevention. Valley Fever Statistics. Fungal Diseases. https://www.cdc.gov/fungal/diseases/coccidioidomycosis/statistics.html. Accessed 30 November 2020.
- ↑ Jump up to: 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 Gowtham J and Agarwall A. Coccidioidomycosis. In: Gupta V, Nguyen Q, LeHoang P, Agarwal A. The Uveitis Atlas. New Delhi: Springer; 2019.
- ↑ Jump up to: 8.0 8.1 Ryan ET and Durand M. Ocular disease. In: Guerrant RL, Walker DH, Weller PF. Tropical infectious diseases: principles, pathogens, and practice, 3rd ed. Philadelphia: Churchill Livingstone; 2011.
- ↑ Cunningham ET, Seiff SR, Berger TG, Lizotte PE, Howes EL, and Horton JC. Intraocular Coccidioidomycosis Diagnosed by Skin Biopsy. Arch Ophthalmol. 1998;116(5):674–677.
- ↑ Davis CN. Coccidioidomycosis: report of a fatal case. Arch Neurol Psychiatry. 1947; 58(5):637-639.
- ↑ Jump up to: 11.0 11.1 Stockamp NW and Thompson GR. Coccidioidomycosis. Infect Dis Clin North Am. 2016; 30(1): 229-246.
- ↑ Galgiani JN et al. 2016 Infectious Diseases Society of America (IDSA) Clinical Practice Guideline for the Treatment of Coccidioidomycosis. Clin Infect Dis. 2016; 63(6): e112–e146.
- ↑ Jump up to: 13.0 13.1 Riddell J, Comer GM., and Kauffman CA. Treatment of endogenous fungal endophthalmitis: focus on new antifungal agents. Clin Infect Dis. 2011; 52(5): 648-653.
- ↑ Cheng ML, Leibowitz M, and Ha E. Coccidioidal endophthalmitis in immunocompetent person, California, USA. Emerg Infect Dis. 2012; 18(6): 1015-1016.
- ↑ Tamesis RR. Coccidioidomycosis. In: Foster CS, Vitale AT. Diagnosis and treatment of uveitis. New Delhi: Jaypee Brothers Medical Publishers; 2013.