Tattoo-associated Uveitis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Tattoo-associated uveitis is a rare condition in which patients may present with uveitis and granulomatous inflammation of tattoos. The entity was first described in a case series in 1952 by Lubeck and Epstein.[1] In general, cases present with bilateral anterior uveitis or bilateral panuveitis and non-caseating granulomas of the involved skin.
In a 2018 review, Kluger suggests that these uveitis cases may be divided into three categories. The first category includes cases associated with systemic sarcoidosis.[2] In patients with sarcoidosis, 25% to 80% may suffer from ocular involvement.[3] The second category includes cases associated with tattoo granulomas.[2] And the third category includes cases of uveitis after tattooing but without tattoo granulomas.
Tattoo-associated uveitis appears to be a rare condition based on the scarcity of reported cases; however, literature review indicates that reports are increasing, possibly due to the increasing prevalence of tattoos. Some estimates suggest that approximately 25% of adults age 18-50 in the United States have tattoos.[4]
Etiology
Although the etiology is unknown, it is speculated that the condition may represent a delayed hypersensitivity reaction to tattoo pigments, or possibly a limited form of sarcoidosis.[2]
Prevalence
The overall prevalence of tattoo induced uveitis is unknown, likely due to underreporting.[5][6] However, a recent review in literature noted that only 39 patients from 1952-2018 have been documented as suffering from granulomatous tattoo reaction with associated uveitis. [5]
Risk Factors
The main risk factor for this condition is the presence of tattoos. Certain colors of tattoo inks have been implicated in reports; however tattoo inks are unregulated and therefore the composition of tattoo inks is not standardized.[7][8] For yet unknown reasons, patients who present with tattoo associated uveitis tend to be younger and more likely to have black tattoos as opposed to colored tattoos. [2]
Histopathology
Tattoo pigments are a complex mix of heavy metals and organic compounds that can contribute to immune dysfunction. Biopsy of inflamed tattoos may reveal non-caseating granulomas, including granulomas that contain tattoo pigment. The presence of tattoo pigment in granulomas suggests the inflammatory response and lymphocytic activation is likely initiated the pigment.[9] It is difficult to distinguish between foreign body granulomas and the granulomas of sarcoidosis.[9]
Pathophysiology
Pathophysiology of tattoo induced uveitis is not well understood, but two hypotheses have been suggested. [5] The first hypothesis suggests a delayed hypersensitivity reaction to the tattoo ink. Tattoo ink contains compounds that can be toxic, mutagenic and carcinogenic. In susceptible individuals, the large antigenic load found in the ink can trigger a delayed hypersensitivity reaction causing tattoo induced uveitis. [6]The second hypothesis suggests that a chronic mild antigenic response from tattoo ink can lead to a systemic granulomatous reaction consistent with sarcoidosis in susceptible individuals. [10]
Diagnosis
History
All uveitis patients should be questioned about the presence of tattoos and any prior episodes of tattoo inflammation. Additional history should be obtained regarding risk factors for infectious etiologies of uveitis, and personal and family history of autoimmune diseases.
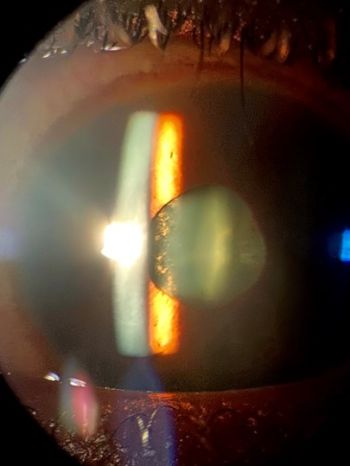
Physical examination
If patients report the presence of tattoos, it is prudent to examine the tattoos for signs of inflammation. A complete ophthalmic examination including dilated fundus examination is warranted to look for evidence of all forms of uveitis - anterior, intermediate, posterior and panuveitis.
Signs
Signs of tattoo-associated uveitis vary depending on the type of uveitis present. In general, tattoos may present with typical signs of inflammation including erythema, edema, induration, pain, warmth, or desquamation. Ocular signs may include conjunctival or scleral injection, tenderness, anterior chamber cell and flare, large keratic precipitates including granulomatous precipitates, posterior synechiae, increased or decreased intraocular pressure, vitreous cell, snowballs or snowbanks, vasculitis, and choroiditis including choroidal granulomas.
Symptoms
Symptoms of uveitis may include pain, redness, sensitivity to light, floaters, and decreased visual acuity. Uveitis and the reaction to the tattoo should occur simultaneously and the symptoms are generally present within the first year after tattooing. [2]
Clinical diagnosis
The diagnosis of tattoo-associated uveitis is based on the presence of both tattoos (especially inflamed tattoos) and uveitis. Diagnosis also generally requires the exclusion of other potential etiologies, especially sarcoidosis.
Diagnostic procedures
All patients with tattoo granulomas and uveitis should have an extensive workup performed to look for evidence of sarcoidosis. Chest radiograph and electrocardiogram (EKG) are recommended. If the chest radiograph is abnormal, or if the patient reports cough or dyspnea, then a high-resolution computed tomography (CT) scan of the chest is indicated to further evaluate for pulmonary sarcoidosis. Additional diagnostic procedures may be indicated depending on the history and physical examination.
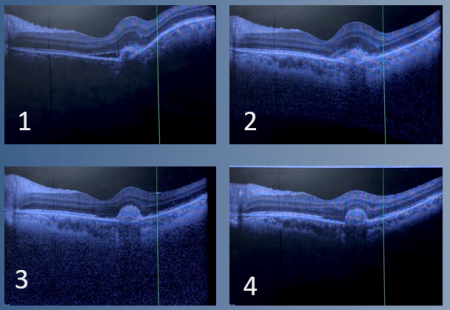
Additionally, OCT-Macula can be obtained if there are signs of posterior involvement. Patients may present with granulomatous lesions which are most effectively visualized with an OCT-Macula, and progression/regression can be objectively seen on follow-up appointments with repeat testing.
Laboratory tests
As above, all patients with tattoo granulomas and uveitis should have an extensive workup performed to look for evidence of sarcoidosis. Laboratory testing should include a complete blood count with differential, a comprehensive metabolic panel, testing for tuberculosis (e.g. Quantiferon or similar test), and screening for syphilis. Some physicians will also obtain serum ACE and/or lysozyme levels as part of the evaluation for sarcoidosis. Additional laboratory tests may be indicated depending on the history and physical examination.
Uveitic Work-Up:
- ESR, CRP – Inflammatory markers
- RPR, FTA-Abs - Syphilis
- PPD or QuantiFERON Gold - Tuberculosis
- ACE, Lysozyme, CXR - Sarcoidosis
- ANA - Systemic Lupus Erythematosus
- ANCA - Granulomatosis with Polyangiitis, Polyarteritis Nodosa
- RF, Anti-CCP - Rheumatoid Arthritis
- HLA-B27 - Ankylosing Spondylitis, Psoriasis
Differential diagnosis
The differential diagnosis of uveitis is extensive. However, given the typical presentation of tattoo-associated uveitis, consideration may be given to infections or inflammatory etiologies. Potential infectious etiologies may include syphilis or tuberculosis. Less likely infectious etiologies may include leptospirosis, toxoplasmosis, toxocariasis, bartonellosis, or Lyme disease. Inflammatory etiologies include most likely sarcoidosis, or less likely Behcet's, VKH[11], or HLA-B27-associated uveitis.
Management
Treatment of tattoo-associated uveitis generally includes topical steroids and often includes systemic steroids. Systemic immunosuppression may be required. For an isolated small tattoo that shows evidence of inflammation, excision could be discussed with the patient as some reports describe resolution after excision.[12][13] Laser tattoo removal is not be advisable, as this could expose additional pigment to the immune system and promote further inflammation. [14][15][16][17] Some physicians may counsel patients against obtaining additional tattoos given the possibility that additional exposure to tattoo ink could worsen or provoke ocular inflammation.[18]
Complications
As with all forms of uveitis, complications of ocular inflammation and steroid treatment of ocular inflammation include peripheral anterior synechiae, posterior synechiae, secondary glaucoma, cataract, retinal detachment, and chorioretinal scarring.
Prognosis
The prognosis of tattoo-associated uveitis is variable, with many patients improving on topical and/or systemic steroids, and some patients requiring systemic immunosuppression. Some patients may require lifelong immunosuppression for severe or recurrent disease.
Additional Resources
- Watch for Tattoo-Related Uveitis: An Emerging Concern. https://www.aao.org/eyenet/article/watch-for-tattoo-related-uveitis
References
- ↑ Lubeck G, Epstein E. Complications of tattooing. Calif Med. 1952 Feb;76(2):83-5. PMID: 14905289; PMCID: PMC1521348.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 Kluger, N. (2018). Tattoo‐associated uveitis with or without systemic sarcoidosis: A comparative review of the literature. Journal of the European Academy of Dermatology and Venereology, 32(11), 1852-1861. doi:10.1111/jdv.15070
- ↑ Ostheimer TA, Burkholder BM, Leung TG, Butler NJ, Dunn JP, Thorne JE. Tattoo-associated uveitis. Am J Ophthalmol. 2014 Sep;158(3):637-43.e1. doi: 10.1016/j.ajo.2014.05.019. Epub 2014 May 27. PMID: 24875002
- ↑ Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol. 2006 Sep;55(3):413-21. doi: 10.1016/j.jaad.2006.03.026. Epub 2006 Jun 16. PMID: 16908345.
- ↑ Jump up to: 5.0 5.1 5.2 Carvajal Bedoya G, Caplan L, Christopher KL, Reddy AK, Ifantides C. Tattoo Granulomas With Uveitis. Journal of investigative medicine high impact case reports. 2020;8:2324709620975968. doi:10.1177/2324709620975968
- ↑ Jump up to: 6.0 6.1 Wenzel S, Rittmann I, Landthaler M, Bäumler W. Adverse reactions after tattooing: review of the literature and compar- ison to results of a survey. Dermatology. 2013;226:138-147.
- ↑ Ostheimer, T. A., Burkholder, B. M., Leung, T. G., Butler, N. J., Dunn, J. P., & Thorne, J. E. (2014). Tattoo-Associated Uveitis. American Journal of Ophthalmology, 158(3). doi:10.1016/j.ajo.2014.05.019
- ↑ Think Before You Ink: Are Tattoos Safe? Retrieved on November 10, 2020 from https://www.fda.gov/consumers/consumer-updates/think-you-ink-are-tattoos-safe.
- ↑ Jump up to: 9.0 9.1 Saliba, N., Owen, M. & Beare, N. Tattoo-associated uveitis. Eye 24, 1406 (2010). https://doi.org/10.1038/eye.2010.17
- ↑ Sepehri M, Hutton Carlsen K, Serup J. Papulo-nodular reactions in black tattoos as markers of sarcoidosis; study of 92 tattoo reactions from a hospital material. Dermatology. 2016;232:679-686.
- ↑ Kesav NP, Kaplan AJ, Hwang CK, Okeagu C, Sen HN. TATTOO-ASSOCIATED CASES OF POSTERIOR SEGMENT UVEITIS WITH VOGT-KOYANAGI-HARADA DISEASE-LIKE FEATURES. Retin Cases Brief Rep. 2022;16(4):457-460. doi:10.1097/ICB.0000000000001007
- ↑ Rorsman H, Brehmer-Andersson E, Dahlquist I et al. Tattoo granuloma and uveitis. Lancet 1969; 2:27–28.
- ↑ Barabasi Z, Kiss E, Balaton G, Vajo Z. Cutaneous granuloma and uveitis caused by a tattoo. Wien Klin Wochenschr 2008; 120: 18.
- ↑ Hibler BP, Rossi AM. A case of delayed anaphylaxis after laser tattoo removal. JAAD Case Rep 2015;1:80-1.
- ↑ Zemtsov A, Wilson LA. Case study of a systemic allergic reaction following CO2 laser tattoo removal. Dermatitis. 1997;8:64.
- ↑ Izikson L, Avram M, Anderson RR. Transient immunoreactivity after laser tattoo removal: Report of two cases. Lasers Surg Med 2008;40:231-2.
- ↑ Meesters AA, De Rie MA, Wolkerstorfer A. Generalized eczematous reaction after fractional carbon dioxide laser therapy for tattoo allergy. J Cosmet Laser Ther 2016;18:456-8.
- ↑ Morales-Callaghan AM Jr, Aguilar-Bernier M Jr, Martinez-Garcia G, Miranda-Romero A. Sarcoid granuloma on black tattoo. J Am Acad Dermatol. 2006;55(5 Suppl):S71-73.