Paracentral Acute Middle Maculopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Paracentral acute middle maculopathy (PAMM) is an optical coherence tomography finding seen in patients with retinal capillary ischemia and unspecific persistent scotomas. PAMM occurs as an isolated phenomenon or as complicating feature of an underlying retinal vasculopathy or systemic disease.
Disease Entity
Paracentral Acute Middle Maculopathy.
Disease
Parecentral Acute Middle Maculopathy (PAMM) is a spectral-domain optical coherence tomographic (SD-OCT) finding first reported in 2013 by Sarraf et al and interpreted as a possible more superficial variant of Acute Macular Neuroretinopathy (AMN).
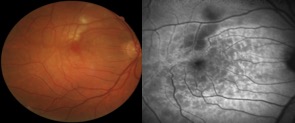
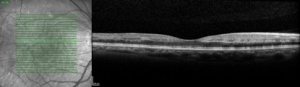
It is characterized by hyperreflective band-like, multiple or isolated focal or diffuse lesions visible at the level of the inner nuclear layer (INL) in patients presenting with acute onset of negative scotoma. It is descriptively termed PAMM due to parafoveal position of the causative grey lesions with near-infrared reflectance imaging, and the SD-OCT localization of involvement to the middle layer (INL) of the retina.
Etiology
The etiology is unknown. A vascular etiology is hypothesized.
Risk Factors
Environmental risk factors such as vasopressor exposure (e.g., caffeine, vasopressors, oral contraceptives) has been proposed and PAMM has recently been associated with numerous retinal vascular diseases including Diabetic Retinopathy, Hypertensive Retinopathy, Sickle Cell Retinopathy, Purtscher Retinopathy, Central Retinal Vein Occlusion, and Retinal Artery Occlusion. A single case of PAMM in uncomplicated pregnancy has been described.
Pathophysiology
PAMM is an SD-OCT abnormality that may herald the presence of a secondary underlying condition predisposing to microvascular ischemic injury. Localized retinal capillary ischemia at the level of intermediate plexus is proposed as the mechanism underlying the development of these lesions.
Primary Prevention
None.
Diagnosis
Clinical diagnosis is based on patient’s history of acute onset negative scotoma with no other visual or ocular symptoms. Funduscopic examination may not reveal significant abnormalities. PAMM lesions appear as subtle whitish parafoveal lesions deeper within the retina, smoother in contour and greyer than cotton wool spots. Emboli may be present at the base of a focal PAMM lesion or along retinal arterial branches and may be visible on high-magnification fundoscopy. As the clinical appearance can be quite subtle by funduscopic examination, reliance on supplemental diagnostic imaging techniques is critical. To date, near-infrared reflectance, fundus autofluorescence and SD-OCT imaging remain the most sensitive modalities. En-face OCT and OCT-angiography have recently emerged as promising tools in the diagnosis and management of these patients.
History
The average age of presentation is in the late 50’s and 60’s, particularly when PAMM is a complicating feature of an underlying retinal vasculopathy or systemic disease (see Risk Factors above). However, may also be idiopathic and may develop in younger and otherwise healthy individuals with a normal systemic history. Patients report the sudden onset of paracentral scotomas without other ocular or visual symptoms.
Physical Examination
Extra-ocular physical examination has no distinct features. For ocular features, see Signs below.
Signs
On OCT, the acute lesions of PAMM characteristically appear as placoid, hyperreflective bands at the level of the INL, sparing the outer retina, showing corresponding hypoautofluorescence on fundus autofluorescence and are hyporeflective and well-demarcated on near infra-red reflectance. A legacy of thinning and atrophy of the affected INL ensues, and is responsible for the permanent visual deficits patients with PAMM typically experience.
OCTA allows for detailed, high-resolution images of the retinal vasculature segmented by layer. Recent cases of PAMM have been imaged using simultaneous en face OCT and OCTA. Enface OCT may emerge as the preferred method to image and follow the clinical course of these patients. Focal vascular remodeling with pruning of the intermediate and posterior capillary plexus over time seems to coincide with evolution of the SD-OCT lesions from hyperreflective plaques into INL atrophy.
Differential diagnosis
The main differential diagnosis is Acute Macular Neuroretinopathy.
Acute Macular Neuroretinopathy is a much more rare entity (less than 100 reported cases in English literature in the last 40 years) and typically affects a young healthy woman in their teens-30’s. The hyperreflective band-like AMN lesions develop slightly lower at the junction of the outer plexiform and outer nuclear layers, and there may be associated persistent disruption of the ellipsoid and interdigitation zones that may help to explain the long standing symptomatic scotomas in some patients with AMN compared with patients with PAMM.
Management
PAMM may be idiopathic and may even develop in young and healthy individuals with an otherwise normal ocular exam. However, in the setting of PAMM with an apparently healthy fundus and appropriate systemic work-up to exclude contributing systemic or cardiovascular risk factors, such as arterial hypertension, dyslipidemia or diabetes, is advisable. Diffuse lesions can harbour an occult central retinal artery occlusion and, in such instances, is mandatory to rule out underlying carotid disease (carotid ultrasound imaging) or giant cell arteritis (ESR, RCP). Wide field fluorescein angiography may also help to rule out associated retinal artery occlusion.
General treatment
None.
Medical therapy
No specific medical intervention can be performed and underlying vascular or systemic disease if present must be addressed accordingly.
Medical follow up
Follow-up is at the discretion and comfort level of the physician and may be every few weeks or months simply to document the course of the disease.
Surgery
Carotid endarterectomy may be necessary if significant carotid obstruction is present.
Complications
None.
Prognosis
Full resolution of scotomas have been reported but partially resolution is the most common outcome. Significant visual impairment is uncommon.
References
- Rahimy E, et al. Paracentral Acute Middle Maculopathy What We Knew Then and What We Know Now. Retina, The Journal of Retinal and Vitreous Diseases 2015, Vol 35, 10
- Chen X, et al. Spectrum of retinal vascular diseases associated with paracentral acute middle maculopathy. Am J Ophthalmol 2015;160(1):26–34;
- Yu S, et al. The spectrum of superficial and deep capillary ischemia in retinal artery occlusion. Am J Ophthalmol 2015;159(1):53–63.e1-2.;
- Rahimy E, et al. Paracentral Acute Middle Maculopathy in Nonischemic Central Retinal Vein Occlusion. Am J Ophthalmol 2014;158:372–380;
- Munk M, et al. New associations of classic acute macular neuroretinopathy. Br J Ophthalmol 2015; 306845.