Hypertensive Retinopathy
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Hypertension is a risk factor for systemic conditions that can lead to target-organ damage. Specifically, hypertension may lead to multiple adverse effects to the eye that can cause retinopathy, optic neuropathy, and choroidopathy. Moreover, hypertension can also cause occlusion of major retinal vessels such as the branch retinal artery, central retinal artery, branch retinal vein, and central retinal vein.[1] [2]This article focuses primarily upon hypertensive retinopathy, which is the most common ocular presentation.
Disease Entity
Disease
The arteriosclerotic changes of hypertensive retinopathy are caused by chronically elevated blood pressure. In 2017, the American College of Cardiology/American Heart Association (ACC/AHA) suggested the following definitions for high blood pressure.[3]
| Category | Systolic (SBP) | Diastolic (DBP) | |||
|---|---|---|---|---|---|
|
|
| |||
|
|
| |||
|
|
|
Hypertensive retinopathy includes 2 disease processes. The acute effects of systemic arterial hypertension are a result of vasospasm to autoregulate perfusion.[4] The chronic effects of hypertension are caused by arteriosclerosis and predispose patients to visual loss from complications of vascular occlusions or macroaneurysms.[5]
Epidemiology
In the United States, 33% of adults have hypertension and only 52% have controlled blood pressures.[6] Hypertensive retinopathy ranges from 2% to 17% in nondiabetic patients, but the prevalence varies by demographic group.[7] Hypertensive retinopathy is more common in African Americans and persons of Chinese descent. In addition, the incidence of hypertension increases with age. Among persons younger than 45 years, men are more likely to be affected by hypertension than women, but among persons older than 65 years, women are more likely to be affected than men.[6]
Etiology
The arteriosclerotic changes of hypertensive retinopathy are caused by chronically elevated blood pressure, defined as systolic blood pressure (SBP) greater than 140 mm Hg and diastolic blood pressure (DBP) greater than 90 mm Hg.[5] Primary hypertension is usually essential and not secondary to another disease process. Essential hypertension is a polygenic disease with multiple modifiable environmental factors contributing to the disease. However, secondary hypertension can develop in the setting of pheochromocytoma, primary hyperaldosteronism, Cushing syndrome, renal parenchymal disease, renal vascular disease, coarctation of the aorta, obstructive sleep apnea, hyperparathyroidism, and hyperthyroidism.[8] Many young patients with secondary hypertension may actually present to an ophthalmologist with bilateral vision loss due to serous macular detachment, bilateral optic disc edema, and exudative retinal detachment. In addition, genetic factors have been associated with a higher risk of hypertensive retinopathy.[9]
Risk Factors
Risk factors for essential hypertension include a high salt diet, obesity, tobacco use, alcohol, family history, stress, and ethnic background. The major risk for arteriosclerotic hypertensive retinopathy is the duration of elevated blood pressure. The major risk factor for malignant hypertension is the degree of blood pressure elevation over normal.
Some studies suggest a genetic influence on retinal vascular caliber. A 2010 population-based study indicated 4 novel loci (19q13, 6q24, 12q24, and 5q14) as significantly associated with retinal venular caliber.[10] Furthermore, locus 12q24 was connected with hypertension and coronary heart disease.
Pathophysiology
Hypertensive retinopathy goes through vasoconstrictive, sclerotic, and exudative phases based upon the extent of hypertension control.
Vasoconstrictive Phase:
In the vasoconstrictive phase, owing to elevated luminal pressures, local autoregulatory mechanisms cause retinal arteriole narrowing and vasospasm to reduce flow.
Sclerotic Phase:
In the sclerotic phase, the layers of the endothelial wall undergo changes such as intimal thickening, medial hyperplasia, and hyaline degeneration,[11] arteriolar narrowing, arteriovenous (AV) crossing changes, and silver and copper wiring.
Exudative Phase:
In the exudative phase, there is a disruption of the blood-brain barrier and leakage of plasma and blood, causing retinal hemorrhages, hard exudates, retinal ischemia, and necrosis of smooth muscle.[11]
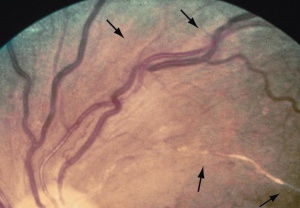
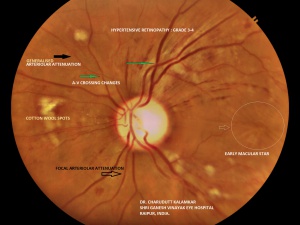
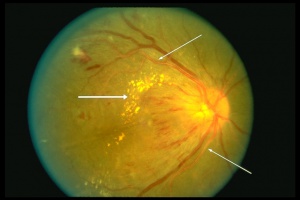
Retinal hemorrhages (Figures 1, 2, and 3) develop when necrotic vessels bleed into either the superficial retinal nerve fiber layer (flame-shaped hemorrhage) or the inner retina (dot-blot hemorrhage). Cotton-wool spots (Figures 1 and 3) are caused by ischemia to the nerve fiber layer secondary to fibrinous necrosis and luminal narrowing. Ischemia to the nerve fibers leads to decreased axoplasmic flow, nerve swelling, and ultimately fluffy opacification. Exudates (Figure 2) occur later in the course of the disease, surrounding areas of hemorrhage, as a result of lipid accumulation. Malignant hypertension can cause papilledema (Figure 3), which is a result of both leakage and of ischemia of the arterioles supplying the optic disc that undergo fibrinous necrosis. Ischemia causes optic nerve edema, whereas leakage causes hemorrhage and disc edema.[12]
Of note, the severity and degree of malignant hypertension corresponds to changes of renal function, highlighting the multi-organ damage caused by systemic microvascular dysfunction.[13]
Primary Prevention
Routine blood pressure monitoring and treatment will prevent hypertensive retinopathy from developing.
Diagnosis
Hypertensive retinopathy is diagnosed based upon its clinical appearance on dilated fundoscopic examination and coexistent hypertension.
History
This should focus upon the patient's hypertension history, symptoms, and complications. To gauge hypertension disease severity, patients should be asked about their severity and duration of hypertension and about the medications taken, as well as their adherence to the medication regimen. Symptoms of hypertension to ask about include headaches, eye pain, reduced visual acuity, focal neurological deficits, chest pain, shortness of breath, dyspnea on exertion, paroxysmal nocturnal dyspnea, orthopnea, and palpitations. Patients should be asked about the complications of hypertension, including history of stroke or transient ischemic attack, history of coronary or peripheral vascular disease, and history of heart failure.[8] Many patients may be asymptomatic.
Physical Examination
The physical examination of a patient with hypertension includes vital signs; cardiovascular, pulmonary, and neurological examinations; and dilated fundoscopy. Vital signs should obviously focus on blood pressure. Key elements of the cardiovascular examination include heart sounds (gallops or murmurs), carotid or renal bruits, and peripheral pulses. Pulmonary examination can identify signs of heart failure if rales are present. Signs of cerebral ischemia can be detected by a good neurological examination.[8] And finally, dilated fundus examination is necessary for staging of hypertensive retinopathy.
Signs
The signs of hypertensive retinopathy include constricted and tortuous arterioles, retinal hemorrhage (Figure 1, 2, and 3), hard exudates (Figure 2), cotton-wool spots (Figure 1 and 3), retinal edema, and papilledema (Figure 3). The signs of chronic arterial hypertension in the retina include widening of the arteriole reflex, arteriovenous crossing signs, and copper (Figures 1 and 3) or silver wire arterioles (copper- or silver-colored arteriole light reflex).[4]
Malignant hypertension can also cause choroidopathy. Fibrinoid necrosis of choroidal arterioles leads to segmental infarction of choriocapillaris.[11] Poor perfusion of the choriocapillaris causes Elschnig spots, defined as hyperpigmented patches in the choroid surrounded by a ring of hypopigmentation, or Siegrist streaks, defined as linear hyperpigmented lesions over choroidal arteries. Hypertensive choroidopathy can cause a focal pigment epithelium detachment, leading to exudative retinal detachment.[5] Generally, hypertensive choroidopathy affects younger patients with malignant hypertension.[14]
Hypertension may lead to optic neuropathy (Figure 3). Hypertensive optic neuropathy, specifically, presents as optic disc swelling.[11] The signs include flame-shaped hemorrhages at the disc margin, blurred disc margins, congested retinal veins, papilledema, and secondary macular exudates.[5] Hard exudates can deposit in the macula, causing a macular star. Optic nerve pallor is also present in patients with chronic hypertension.
Symptoms
Malignant Hypertension
Acute malignant hypertension will cause patients to complain of eye pain, headaches, or reduced visual acuity.[4] However, the complications of arteriosclerotic hypertensive changes will cause patients to present with the typical symptoms of vascular occlusions or macroaneurysms.
Chronic Hypertension
Chronic arteriosclerotic changes from chronic hypertension will not cause any symptoms alone, but patients often experience decreased vision.
The Scheie Classification below delves into the retinopathic changes seen in both acute, malignant hypertension and chronic, systemic hypertension.
Clinical Diagnosis
The signs of malignant hypertension are well summarized by the Modified Scheie Classification of Hypertensive Retinopathy[5]:
- Grade 0: No changes
- Grade 1: Barely detectable arterial narrowing
- Grade 2: Obvious arterial narrowing with focal irregularities (Figure 1)
- Grade 3: Grade 2 plus retinal hemorrhages, exudates, cotton-wool spots, or retinal edema (Figure 3)
- Grade 4: Grade 3 plus papilledema (Figure 4)
The signs of chronic arteriosclerotic hypertension are also summarized by the Scheie Classification[4]:
- Stage 1: Widening of the arteriole light reflex
- Stage 2: Stage 1 + Arteriovenous crossing sign (Figure 3)
- Stage 3: Copper wiring of arterioles (copper-colored arteriole light reflex)
- Stage 4: Silver wiring of arterioles (silver-colored arteriole light reflex).
Another classification schema is the Keith-Wagner-Barker classification proposed in 1939.[15]
- Grade 1: Mild, generalized constriction of retinal arterioles
- Grade 2: Definite focal narrowing of retinal arterioles + AV nicking
- Grade 3: Grade 2 + flame-shaped hemorrhages + cotton-wool spots + hard exudates
- Grade 4: Severe Grade 3 retinopathy + papilledema or retinal edema
Of specific interest is the classification of hypertensive retinopathy by Wong and Mitchell (2004), in which the worsening grades of retinopathy were more strongly associated with systemic issues.[16] The classification is as follows:
- None: no detectable signs
- Mild: one or more of the following: generalized arteriolar narrowing, focal arteriolar narrowing, arteriovenous nicking, opacity (“copper wiring”) of the arteriolar wall
- Moderate: one or more of the following: retinal hemorrhage (blot, dot, or flame-shaped), microaneurysm, cotton-wool spots, hard exudate, or a combination of these signs
- Severe: moderate retinopathy plus swelling of the optic disc
A new classification was proposed in 2014, based on optical coherence tomography (OCT) features such as subretinal fluid (SRF). The study compared the grading system based on OCT findings to the Keith-Wagener-Barker grading system and found that the following classification was significantly correlated to final best-corrected visual acuity.[17]
- Mild-moderate retinopathy
- Malignant retinopathy w/o SRF
- Malignant retinopathy w/SRF
Diagnostic procedures
Fluorescein angiography (FA) during acute malignant hypertension will demonstrate retinal capillary nonperfusion, microaneurysm formation, and a dendritic pattern of choroidal filling in the early phase. In the late phase, diffuse leakage will be seen.[5] Indocyanine green angiography during malignant hypertension will show a moth-eaten appearance of the choriocapillaris.[5] Fluorescein angiography can demonstrate hypertensive choroidopathy. FA will show focal choroidal hypoperfusion in the early phases and subretinal leakage in the later phases.[5]
Differential diagnosis
The differential for hypertensive retinopathy with diffuse retinal hemorrhage, cotton-wool spots, and hard exudates includes, most notably, diabetic retinopathy. Diabetic retinopathy can be distinguished from hypertensive retinopathy by evaluation for the individual systemic diseases.[4] Other conditions with diffuse retinal hemorrhage that can resemble hypertensive retinopathy include radiation retinopathy, anemia, and other blood dyscrasias, ocular ischemic syndrome, and retinal vein occlusion. Conditions with optic disc edema also include diabetic papillopathy, anterior ischemic optic neuropathy, and neuroretinitis.
Management
The treatment for hypertensive retinopathy is primarily focused upon reducing blood pressure. It is important to work together with the patient’s primary care doctor to ensure timely evaluation and management to reduce ocular and systemic damage. A thorough history is vital for the proper and timely treatment of hypertensive retinopathy to prevent vision-threatening complications.
General treatment
The treatment for moderate to severe hypertensive retinopathy is to reduce the mean arterial pressure by 10%-15% in the first hour. Of note, blood pressure should be lowered in a controlled manner and by no more than 25% compared to baseline by the end of the first day of treatment to prevent further ischemic damage to target end organs. Initial treatment often requires administering parenteral antihypertensive agents and then transitioning to oral agents. Goal-oriented hypertension treatment aims to lower systolic blood pressure to < 130 mm Hg and diastolic pressure to < 80 mm Hg over the next 2-3 months.[18]
Medical therapy
Drugs that are commonly used in the outpatient setting to reduce blood pressure include angiotensin-converting enzyme inhibitors, calcium channel blockers, and diuretics. Other less commonly used medications include α-adrenergic blockers, direct vasodilators, and central α2-adrenergic agonists. Patients should be followed closely by their primary physician for management of hypertension. Patients in hypertensive crisis should be referred to an emergency department for acute management of blood pressure.
Studies have explored intravitreal antibody treatment against vascular endothelial growth factor (bevacizumab) for acute hypertensive retinopathy and showed a reduction in macular edema and retinal hemorrhage.[6] One study showed prompt recovery of malignant hypertensive retinopathy in patients after administration of bevacizumab.[19] However, the use of these agents has not yet become widespread or widely accepted.
Medical follow-up
Follow-up is dependent upon the degree of hypertensive retinopathy and status of hypertension. Close contact is essential between the ophthalmologist and the primary care physician for consistent follow-up individually tailored to each patient.
Surgery
There is no surgical treatment for essential hypertension or its ocular complications. In cases of secondary hypertension, surgical treatment may be effective, depending upon the etiology.
Complications
Hypertension predisposes patients to many other retinal vascular diseases including central or branch retinal artery occlusion, central or branch retinal vein occlusion, and retinal arterial macroaneurysms. Ischemia secondary to vascular occlusions can cause neovascularization, vitreous hemorrhage, epiretinal membrane formation, and tractional retinal detachment. Hypertension also leads to more advanced diabetic retinopathy progression.[5] Hypertensive optic neuropathy can cause chronic papilledema, leading to optic nerve atrophy and severe loss of visual acuity.[4] It may also be a risk factor for glaucoma. Recently the term "proliferative hypertensive retinopathy" has been coined.[20]
Prognosis
Patients with severe hypertensive retinopathy and arteriosclerotic changes are at increased risk for coronary disease, peripheral vascular disease, and stroke. Mortality of patients with untreated malignant hypertension was 50% in 2 months and 90% in 1 year.[15] Since arteriosclerotic changes in the retina do not regress, these patients remain at increased risk for retinal artery occlusions, retinal vein occlusions, and retinal macroaneurysms. Most retinal changes secondary to malignant hypertension will improve once blood pressure is controlled, but arterio-venous changes and arteriolar narrowing will remain. Damage to the optic nerve and macula, however, could cause long-term reductions in visual acuity.
Additional Resources
- http://en.wikipedia.org/wiki/Hypertensive_retinopathy
- http://www.nlm.nih.gov/medlineplus/ency/article/000999.htm
- http://emedicine.medscape.com/article/1201779-overview
- https://www.uptodate.com/contents/moderate-to-severe-hypertensive-retinopathy-and-hypertensive-encephalopathy-in-adults
- Porter D, Vemulakonda GA. Blood Pressure. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/blood-pressure-list. Accessed January 07, 2025.
Reference
- ↑ Tsukikawa, M., & Stacey, A. W. (2020). A Review of Hypertensive Retinopathy and Chorioretinopathy. Clinical optometry, 12, 67–73. https://doi.org/10.2147/OPTO.S183492
- ↑ ALEX MELAMUD, PETER K. KAISER,Chapter 28 - Hypertensive Retinopathy; Editor(s): David Huang, Peter K. Kaiser, Careen Y. Lowder, Elias I. Traboulsi,Retinal Imaging, Mosby,2006,Pages 283-288, ISBN 9780323023467
- ↑ 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 Lang, G.K. Ophthalmology: A Pocket Textbook Atlas (Thieme, Stuttgart, 2007).
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 AAO. in Basic and Clinical Sciences Course (Lifelong Education for the Ophthalmologist, San Fransisco, CA, 2006).
- ↑ Jump up to: 6.0 6.1 6.2 Harjasouliha A, Raiji V, Gonzalez J, Review of hypertensive retinopathy. Dis Mon. 2017 Mar;63(3):63-69.
- ↑ T. Nwankwo, S.S. Yoon, V. Burt, Q. Gu. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief, 133 (2013), pp. 1-8.
- ↑ Jump up to: 8.0 8.1 8.2 Katakam, R., Brukamp, K. &amp; Townsend, R.R. 2008. What is the proper workup of a patient with hypertension? Cleve Clin J Med 75: 663-72.
- ↑ Pontremoli R, Sofia A, Tirotta A, et al. The deletion polymorphism of the angiotensin I-converting enzyme gene is associated with target organ damage in essential hypertension. J. Am. Soc. Nephrol. 1996 Dec;7(12):2550-8.
- ↑ Konstantinidis, L., & Guex-Crosier, Y. (2016). Hypertension and the eye. Current opinion in ophthalmology, 27(6), 514–521. https://doi.org/10.1097/ICU.0000000000000307
- ↑ Jump up to: 11.0 11.1 11.2 11.3 Modi P, Arsiwalla T. Hypertensive Retinopathy. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020-.2020 Jan 8.
- ↑ Garner, A. & Ashton, N. 1979. Pathogenesis of hypertensive retinopathy: a review. J R Soc Med 72: 362-5.
- ↑ Shantsila, A., & Lip, G. (2017). Malignant Hypertension Revisited-Does This Still Exist?. American journal of hypertension, 30(6), 543–549. https://doi.org/10.1093/ajh/hpx008
- ↑ Bourke K, Patel MR, Prisant LM. Marcus DM. Hypertensive choroidopathy. J Clin Hypertens 2004 Aug;6(8):471-2.
- ↑ Jump up to: 15.0 15.1 Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am. J. Med. Sci. 1974 Dec;268(6):336-45.
- ↑ Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004 Nov 25;351(22):2310-7. doi: 10.1056/NEJMra032865. PMID: 15564546.
- ↑ Ahn SJ, Woo SJ, Park KH. Retinal and choroidal changes with severe hypertension and their association with visual outcome. Invest Ophthalmol Vis Sci 2014; 55:7775–7785.
- ↑ Elliott W, Varon J. Moderate to severe hypertensive retinopathy and hypertensive encephalopathy in adults. UpToDate. January 21. 2020
- ↑ Kim EY, Lew HM, Song JH. Effect of intravitreal bevacizumab (Avastin((R))) therapy in malignant hypertensive retinopathy: a report of two cases. J Ocul Pharmacol Ther 2012; 28:318–322.
- ↑ Stryjewski TP, Papakostas TD, Vavvas D. Proliferative Hypertensive Retinopathy. JAMA Ophthalmol 2016;:1. doi:10.1001/jamaophthalmol.2015.5583