Optic Disc Hemorrhage
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disc hemorrhages are characteristic linear hemorrhages perpendicular to the optic disc, most commonly on the superotemporal or inferotemporal margin. The cause of disc hemorrhages has not been fully characterized, and mechanical and vascular hypotheses with evidence supporting both have been proposed. Although disc hemorrhages can occur in eyes with no signs of glaucoma, in glaucomatous eyes, disc hemorrhages are a possible indicator of progression. Disc hemorrhages themselves cannot be treated but their presence may warrant clinical monitoring or intensification of intraocular pressure (IOP) lowering therapy in glaucomatous eyes. The purpose of this article is to provide a review of disc hemorrhage for the trainee and practicing ophthalmologist.
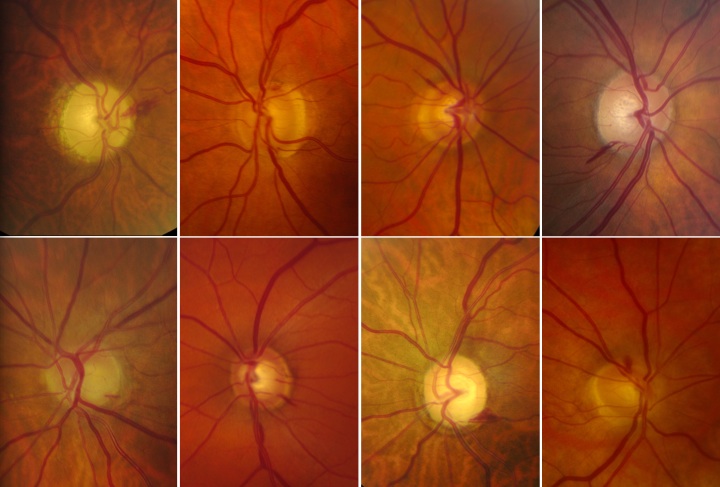
Figure 1. A selection of typical appearing disc hemorrhages.
Disease Entity
Disc hemorrhage.
Alternate names: optic disc hemorrhage, Drance hemorrhage, splinter hemorrhage, nerve fiber layer hemorrhage, optic nerve head hemorrhage.
Disease: Disc Hemorrhages
Disc hemorrhages are splinter or flame-shaped hemorrhages oriented perpendicular to the optic disc margin (Figure 1).[1][2][3][4] Classically, these hemorrhages are located in the prelaminar optic disc, cross the peripapillary zone, and extend into the adjacent superficial retinal nerve fiber layer,[1][3][4] although they may not occupy the entire length from disc to retina.[4] Alternately, deeper disc hemorrhages may appear round and blotchy.[3] Less commonly, a disc hemorrhage may be noted in the peripapillary retinal nerve fiber layer reaching within one disc diameter of the optic disc margin.[2]
Etiology and Pathophysiology
Mechanical and Vascular Hypotheses
Although disc hemorrhages have been the subject of tremendous research, the exact mechanism by which they appear remains elusive. Two primary hypotheses exist: mechanical and ischemic vascular.
Proponents of the mechanical theory hypothesize that disc hemorrhages result from mechanical shearing at the lamina cribrosa[5] or damage to the capillary network at the border of retinal nerve fiber layer defect enlargement.[6] Essentially, this theory suggests that the primary insult is neurodegenerative, causing changes or stretching of connective tissue, remodeling of lamina cribosa, and/or traction from glial scar formation, which in turn damages the microvascular network leading to hemorrhage. The hemorrhage is a secondary event resulting from tissue damage.[7][8]
Other authors suggest various vascular etiologies,[9][10][11][12][13] for example, ischemic microinfarction in the optic nerve head[9] or perturbation of the blood-retinal barrier.[12][13] In this theory, a yet unknown primary vascular problem increases vessel susceptibility to damage and rupture. Recent use of OCT angiography has shown that 46.3% of eyes with disc hemorrhages show peripapillary choroidal microvascular dropout at the site of hemorrhage, as compared to 29.4% of eyes without hemorrhage.[14] Further, densitometric studies have suggested that the blood from ODHs may have an arterial origin.[15][16][17]
The etiology of optic disc hemorrhages remains an area of active research. Given the presence of disc hemorrhages in glaucomatous and non-glaucomatous eyes,[4][18] it is probable that multiple factors may contribute to their development. The relationship between pathogenesis and ODH location, shape, and retinal depth is an ongoing area of research. [19][8][20]
The Relationship to Rim Notches
A neural rim notch is a localized divot in the neuroretinal rim. Several studies have noted a positive association between rim notching and ODH.[21][22][23] In a study of 33 eyes for which optic disc images prior to development of a disc hemorrhage were available for review, Law and colleagues noted that all eyes with preexisting neural rim notches had a subsequent disc hemorrhage at or adjacent to the notches.[24] Their observations that a rim notch may precede disc hemorrhage (on average, by 21.5 months) and that disc hemorrhages occurred at or adjacent to rim notches[24] differed from older work[3][25] that suggested disc hemorrhages precede notches. The fact that disc hemorrhages occur at or near preexisting rim notches lends evidence to the theory that glaucomatous damage begins prior to the appearance of a hemorrhage.
Epidemiology
Prevalence
Several population-based studies[18][26][27][28][29][30][31] have reported disc hemorrhage prevalence estimates ranging from 0.6%[26][27] to 1.4%.[18][32] The Beaver Dam Eye Study and Blue Mountains Eye Study, which have similar methodologies, reported an overall disc hemorrhage prevalence of 0.9%[28] and 1.4%,[18] respectively. Disc hemorrhage prevalence in the first survey of residents of Dalby, Sweden was 0.8%,[30] and in repeated surveys of Dalby residents, the prevalence was 0.7%.[29] Two large-scale eye disease screening projects on healthy Japanese adults each revealed a prevalence of 0.6%.[26][27] The Beijing Eye Study, a population-based survey in Northern China, reported a prevalence of 1.2%.[31] The 13-year follow-up data from the African Descent and Glaucoma Evaluation Study reported an ODH prevalence of 4.4% in patients of European descent and 1.1% in patients of African descent.[33] Accordingly, the prevalence of ODH may vary between populations and ethnicities, although the specific mechanism behind these differences is unclear.
Although the observation of a disc hemorrhage should prompt a thorough investigation for glaucoma, the overall low prevalence of disc hemorrhages in population-based studies limits their usefulness as an effective glaucoma screening tool.[2][34] The reported prevalence of disc hemorrhage in different types of glaucoma also varies.[35] In the Blue Mountain Eye Study, disc hemorrhages were present in 13.8% of participants with open-angle glaucoma (OAG; 8% of patients with high-pressure glaucoma and 25% of patients with low-pressure glaucoma), 1.5% of patients with ocular hypertension, and 1% of normals.[18] Thirteen-year follow up data of the OHTS study demonstrates a low incidence of ODH in participants with OHT alone (0.5%/year), but a doubling of the incidence of ODH after POAG has developed (1.2%/year).[36]
Notably, most reports of disc hemorrhage prevalence are subject to selection bias because they have reported on subjects with ocular hypertension, suspected glaucoma, or diagnosed glaucoma often selected from clinical or hospital populations. In studies of subjects with open angle glaucoma,[25][30][37][38][39] for example, disc hemorrhage prevalence ranges from 4.7%[37] to 58.3%.[30] Similarly, in patients with normal tension glaucoma, the prevalence of ODH ranged between 20.5 and 33.3%. [40]
Overall, disc hemorrhages have been observed more frequently in early compared with advanced glaucoma[41][42] and in patients with normal-tension rather than high-pressure glaucoma.[18][38][43]
Associations
Multiple studies have identified both local and systemic associations with disc hemorrhages.
Ocular
Related to the eye, increased vertical cup-to-disc ratio,[18][37][44] relatively low IOP,[3][38][45] nerve fiber layer atrophy,[46] worsening visual fields,[47][48][49][50] and multiple other ocular variables are associated with disc hemorrhages. In the 13 year OHTN analysis, thinner central corneal thickness, larger vertical cup-to-disc ratio, and higher intraocular pressure were identified as risk factors for ODH. [36]
An association between peripapillary atrophy, specifically beta zone, and disc hemorrhage was demonstrated in a cohort of mostly normal-tension glaucoma patients with unilateral disc hemorrhage,[51] and a large-scale study of apparently healthy subjects revealed that the prevalence of peripapillary atrophy (both alpha and beta zone) was significantly greater in eyes with ODH compared to those without ODH.[26] However, in a study of bilateral OAG eyes, the eye with a disc hemorrhage and the contralateral eye did not vary with respect to the size of the alpha or beta zone peripapillary atrophy.[52]
Ocular vascular abnormalities have also been associated with ODH. Decreased intra-disc vessel density has been associated with ODH in eyes with POAG.[53]
Several studies reported that OAG eyes with ODH demonstrate significantly decreased parapapillary choroidal vascular density compared to OAG eyes with no ODH.[54][55][14] Similar associations have been reported in non-glaucomatous eyes.[56] Areas of choroidal loss appear to be localized and often spatially correspond to the ODH location.[54] ODH has also been associated with decreased radial peripapillary capillary density in NTG patients.[57]
Further, ODH has been found to predict faster vessel density loss in both POAG and glaucoma suspects.[58] Using OCTA to observe choroidal microvascular dropout has been suggested as a biomarker for OAG progression in eyes with ODH.[14]
Low mean arterial ocular perfusion pressure has also been described as a risk factor for ODH development in NTG patients.[59][60] A recent study found an association between seasonal temperature changes and ODH incidence; the authors hypothesized that low temperatures may cause increased IOP and decreased ocular blood flow, potentially leading to the relatively higher ODH incidence reported in winter months.[61]
Systemic
A selection of systemic associations and authors who noted these associations are shown in Table 1.
| Systemic associations | Significant Association Observed | No Significance Observed |
|---|---|---|
| Age | Healey[18], Sugiyama[26], Bengtsson[62], Yamamoto[27], Budenz[36], Jonas[63], Tomidokoro[64], Kim YK[65] | |
| Female gender | Healey[18], Yamamoto[27], Sugiyama[26], Klein[28], Bengtsson[62], Tomidokoro[64] | |
| African American race | Budenz[36] (self-reproted), Skaat[33] | |
| Systemic hypertension or elevated systolic blood pressure | Healey[18], Kottler[66], Drance[67], Jonas[63], Tomidokoro[64], Kim YD [35] | Soares[45], Diehl[37], Grodum[68], Tuulonen[69], Budenz[36] |
| Low systolic blood pressure | Furlanetto[59] | Budenz[36] |
| Vascular disease: angina, MI, stroke | Healey[18], Bundez[36] | |
| Migraine | Healey[18] (glaucomatous eyes only), Furlanetto[59] | Budenz[36] |
| Cold extremities | Kim[70] | |
| Diabetes | Soares[45], Healey[18], Shihab[71], Poinoosawmy[72], Tuulonen[69] | Diehl[37], Grodum[68], Kottler[66], Budenz[36] |
| Use of systemic anti-hypertensives | Furlanetto (beta-blockers specifically)[59] | Grodum[68] |
| Aspirin use | Soares[45], Grodum[68] | |
| Exfoliation syndrome | Healey[18] | |
| Smoking status | Healey[18], Bundez[36] | |
| Renal function impairment | Lee JY[73] |
Diagnosis
Physical Examination and Clinical Diagnosis
Clinical examination of the optic disc and peripapillary retina is performed with a high magnification convex lens and slit lamp biomicroscope. The findings should be described and the location of a disc hemorrhage should be drawn and photographed.[2]
ODH can be a subtle finding on both clinical exam and fundus photography.[74] Interestingly, in the Ocular Hypertensive Treatment Study (OHTS), significantly more disc hemorrhages (84%) were detected on annual photographic review at a dedicated reading center than were detected on clinical exam and photographic review at the clinical encounter (16%),[4] a finding that emphasizes the challenge of identifying disc hemorrhages on exam alone. Notably, ODH lesions in patients with high tension glaucoma have been noted to be smaller than those in normal tension glaucoma, possibly due to IOP-related blood confinement.[75]
At present, optic disc imaging techniques are unable to reliably identify disc hemorrhages. Currently, imaging functions as an adjunct to, rather than a replacement for, clinical examination.
Artificial Intelligence and deep-learning-based methodologies are being researched to improve the quality of optic disk photographs and aid in ODH detection.[76][77][78] Some models have reported sensitivities and specificities similar to a clinician, but are not in clinical use at this time.[77]
Location
Classically, disc hemorrhages associated with glaucoma are found mostly in the inferotemporal and superotemporal regions of the optic disc (Figure 2).[27][45][71][79] The 7 o’clock hour has been reported as a common location of ODH.[19][20] In a study of 128 primary open angle glaucomatous eyes with disc hemorrhage, Kim and colleagues mapped 58.0% to the inferior sector of the inferotemporal quadrant, 40.6% to the disc rim.[40] They also noted larger and longer hemorrhages in cases of normal baseline IOP compared to patients with baseline high IOP.
In one prospective study of 195 eyes with POAG, sites showing ultimate structural progression in RNFL defects were more common in the inferior and temporal disk quadrants.[20]
Figure 2. Inferotemporal disc hemorrhage of the left optic nerve head.
Duration and Recurrence
Weekly photography has demonstrated that optic disc hemorrhages persist for 2 to 35 weeks and on average are present for about 6-12 weeks.[38][17] A recurrent disc hemorrhage was observed in 64% of eyes, 92% of which occurred within 28 weeks of the prior hemorrhage.[38]
Diagnostic Procedures
As noted above, documentation of a disc hemorrhage is accomplished both by drawing the location of the hemorrhage with respect to the optic nerve and taking disc photographs. Clinical examination remains an essential component of diagnosis.
Differential diagnosis
Although disc hemorrhages are strongly associated with glaucoma, there are other causes. Textbooks,[2][80] reviews,[1] articles,[4] and letters[34] cite diabetes mellitus, optic disc drusen, ischemic optic neuropathies, vascular diseases of the retina, systemic hypertension, leukemia, and systemic lupus erythematosus among the possible causes of linear hemorrhages at the optic disc, although little primary literature addresses these associations.
Posterior vitreous detachment can also cause optic disc hemorrhage.[81][82] In a recent study, PVD-related and glaucomatous ODH were found to have differing shapes on presentation. PVD cases were more commonly flame-shaped than splinter-shaped (60.9% vs. 34.8%, respectively), while glaucomatous cases were more likely to have splinter shapes (92.3%) than flame shapes (7.7%, p <0.001).[19] Further, PVD cases were relatively more likely to have a nasal location and larger area in comparison to glaucomatous cases.[19]
A thorough history and close evaluation for evidence of nonglaucomatous optic neuropathies, disc edema, retinal abnormalities, or retinal vasculature changes may help to distinguish these entities as a potential cause of disc hemorrhage.
Whether disc hemorrhages can occur in normal eyes is discussed below.
Management
The observation of a disc hemorrhage should prompt a thorough investigation for glaucoma, and individuals with disc hemorrhages should be considered glaucoma suspects.[3] Early identification of glaucoma and subsequent significant IOP reduction is the only treatment at present to prevent vision loss, perimetric progression, and changes to the disc and retinal nerve fiber layer.
In individuals with known glaucoma, a disc hemorrhage may be a sign of active disease and progression. Accordingly, some authors suggest that the presence of ODH should prompt regular VF monitoring.[83][84] Thus, while a disc hemorrhage does not need to be treated, per se, its presence may signal the need to initiate or intensify IOP-lowering therapy. The effect of IOP lowering treatment is discussed below.
Prognosis
Numerous studies show disc hemorrhages to be an important risk factor in the development and progression of glaucoma and visual field loss.
Development of Glaucoma
In a review of several population studies, Jasty et al. found that patients with ODH were at a greater risk for POAG development.[17] In the 13-year follow-up analysis of the OHTS, the cumulative incidence of POAG in eyes with hemorrhage was 25.6% compared with 12.9% in eyes without disc hemorrhage.[36] In eyes in which the end point of POAG developed, the median time between disc hemorrhage and POAG was 13 months.[4] Multivariateanalysis revealed that the presence of ODH increased the risk of developing POAG 3.7-fold. Similarly, in the Collaborative Normal-Tension Glaucoma Study (CNTGS), a patient with a disc hemorrhage at enrollment had 2.72 times the chance of developing a perimetric endpoint.[49]
A recent review argued that ODH may be an indicator ongoing glaucomatous damage, rather than a causative risk factor of its development.[8] These authors suggest that early, undetectable axonal loss may occur prior to ODH development, with ODH development occurring as a result of glaucoma progression and independently of the causal pathogenic mechanism.[8] Others have suggested that ODH may occur due to capillary disruption during RNFL defect enlargement.[85][8] It is unclear if ODH is a sign of, or risk factor for, progression.[8][86][87] Further research on ODH pathogenesis may allow more definitive conclusions; yet, ODH still has value as a clinical indictor of potential glaucoma progression.
Do all individuals with disc hemorrhage develop glaucoma?
Although many authors and glaucoma specialists have developed opinions as to whether nonglaucomatous eyes can have disc hemorrhages, there is no clear consensus in the literature. In the Blue Mountain Eye Study, 70% of disc hemorrhages were observed in eyes without glaucoma (diagnosed by perimetric criteria in the presence of optic disc criteria).[18] Similar diagnostic criteria were used in the Beaver Dam Eye Study, and 96% of disc hemorrhages were observed in eyes without glaucoma.[28] In the OHTS, 78 % of subjects with a disc hemorrhage did not develop a POAG endpoint in a median follow up 49 months after disc hemorrhage.[36]
In contrast, two studies found no disc hemorrhages in healthy eyes; they were observed only in suspect[37] and glaucomatous eyes.[37][41] Kitazawa and colleagues found that only 0.4% of normal patients observed consecutively at the University of Tokyo had a disc hemorrhage; a much higher prevalence of hemorrhage was observed in patients with low tension glaucoma and POAG (20.5% and 4.2%, respectively).[38]
Some of the variability between these studies is likely due to their definitions of glaucoma and length of follow up. Although diagnostic criteria for glaucoma may not be met at the time of disc hemorrhage observation, many eyes may eventually progress to glaucoma. There is likely a complex relationship between POAG and ODH, with many contributory variables such as age, ethnicity, and gender, among others.[17] As emphasized elsewhere, the presence of a disc hemorrhage should prompt a thorough investigation for glaucoma.
Progression of Glaucoma
In patients with glaucoma, studies support associations between disc hemorrhages and perimetric progression,[47][48][49][50][20] optic disc changes,[50] retinal ganglion cell loss,[88] and retinal nerve fiber layer thinning.[46]
Disc hemorrhage at the time of study enrollment was a risk factor for perimetric progression in the CNTGS.[49] In fact, a recent review of 85 articles investigating prognostic factors for visual field progression in patients with OAG found a clear association between visual field progression and disc hemorrhage in patients with NTG.[47] The association between disc hemorrhage and perimetric progression is likely similar in the various glaucomas. For example, Rasker and colleagues observed an association between visual field deterioration and disc hemorrhage in eyes with normal pressure glaucoma, POAG, and ocular hypertension.[48] In the Early Manifest Glaucoma Trial, as the percentage of patient visits with disc hemorrhages increased, as noted by clinical assessment rather than photographic review, the risk of perimetric and photographic optic disc criteria progression increased.[50]
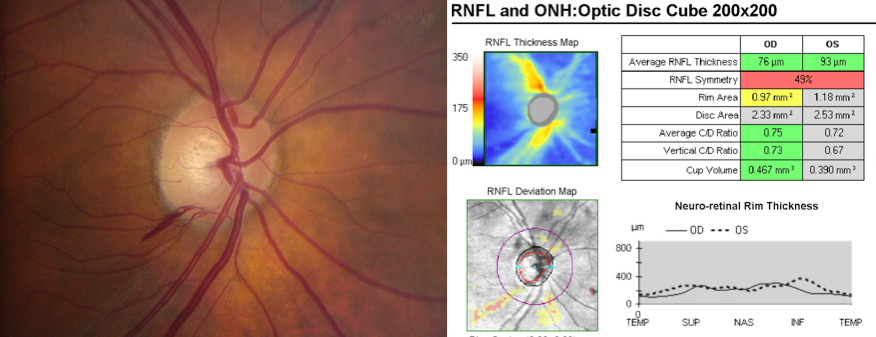
Eyes with ODH have been found to be significantly more likely to have visual field loss progression.[84][20] ODH eyes were also found to have faster rates of progression than eyes without ODH.[84][83][88] In glaucomatous eyes, the rate of visual field loss was approximately 5.5 times faster in ODH eyes than non-ODH eyes. [84] Similarly, recent spectral-domain optical coherence tomography research revealed an association between disc hemorrhage and progressive retinal nerve fiber layer thinning in glaucomatous eyes.[46] Figure 3 demonstrates inferotemporal focal retinal nerve fiber layer thinning at 18 months following a disc hemorrhage in the same location.
Figure 3. Inferotemporal disc hemorrhage of the right eye is seen in the left panel. Eighteen months later, Cirrus optical coherence tomography (right panel) demonstrates retinal nerve fiber layer thinning corresponding with the location of the prior disc hemorrhage.
Exfoliation Glaucoma
Exfoliation glaucoma (XFG), the most common type of secondary open angle glaucoma,[89] tends to progress more quickly and become more severe compared to POAG.[89][90][91][92] Disc hemorrhage has been shown to be an independent risk factor for progression of XFG.[93]
Recurrent Disc Hemorrhages: The two-population hypothesis
Eyes with ODH are at an elevated risk of recurrent ODH. As noted above, a weekly photography study demonstrated recurrent disc hemorrhage in 64% of eyes, and 72% of recurrent hemorrhages occurred in the same optic disc quadrant.[38] Similarly, Ishida and colleagues observed recurrent disc hemorrhages in 71.9% of subjects in their cohort of untreated NTG patients, and 78.2% of recurrences were in the same quadrant.[79] Interestingly, they observed that eyes with recurrent disc hemorrhages were significantly more likely to demonstrate visual field progression compared to eyes with only a single observed disc hemorrhage (mean follow up 5.6 years).[79] The CNTGS also found a higher frequency of disc hemorrhages in patients whose glaucoma progressed even when adjusted for follow up time.[49] However, recurrent ODH has not been linked to an increased rate of VF loss compared to single-occurrence ODH.[75]
Observations like these have led some authors to propose two populations of glaucoma patients: bleeders and nonbleeders.[38][79][94][95][96] Some eyes may suggested to be particularly predisposed to disc hemorrhage even with adequate IOP-lowering therapy, and this may be especially true of eyes with NTG.[94] The significance of the two population hypothesis with respect to progression and treatment has not been fully established.
Effect of Treatment
Whether IOP reduction lowers the frequency of disc hemorrhages has not been fully established.[4][62][94][95] Some studies suggest a decrease in disc hemorrhage frequency with significant IOP reduction,[94][95] which may be more readily achieved in primary open angle glaucoma (POAG) and glaucoma suspects compared with normal tension glaucoma (NTG) eyes.[95] IOP lowering medications were found to have no effect on hemorrhage development in patients with normal tension glaucoma.[36] Conversely, long-term analysis of the OHTS data shows a strong relationship between randomization to treatment group and disc hemorrhage. Participants in the treatment group had a 30% lower hazard ratio for a disc hemorrhage, a trend that was seen in earlier OHTS studies but was not significant until 13-year follow up. [4][36]
Future Work
Additional research is needed to determine exactly why disc hemorrhages occur and to clarify why only some glaucoma patients develop disc hemorrhages so we may better understand the associated implications for prognosis and management. Advances in imaging techniques and artificial intelligence may help elucidate future answers to these questions.
References
- ↑ 1.0 1.1 1.2 Uhler TA, Piltz-Seymour J. Optic disc hemorrhages in glaucoma and ocular hypertension: implications and recommendations. Curr Opin Ophthalmol. 2008;19(2):89–94.
- ↑ 2.0 2.1 2.2 2.3 2.4 Schacknow PN, Samples JR eds. The glaucoma book: a practical, evidence-based approach to patient care. New York: Springer; 2010.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Drance SM. Disc hemorrhages in the glaucomas. Surv Ophthalmol. 1989;33(5):331–337.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Budenz DL, Anderson DR, Feuer WJ, et al. Detection and prognostic significance of optic disc hemorrhages during the Ocular Hypertension Treatment Study. Ophthalmology. 2006;113(12):2137–2143.
- ↑ Quigley HA, Addicks EM, Green WR, Maumenee AE. Optic nerve damage in human glaucoma. II. The site of injury and susceptibility to damage. Arch. Ophthalmol. 1981;99(4):635–649.
- ↑ Nitta K, Sugiyama K, Higashide T, et al. Does the enlargement of retinal nerve fiber layer defects relate to disc hemorrhage or progressive visual field loss in normal-tension glaucoma? J. Glaucoma. 2011;20(3):189–195.
- ↑ Kim KO, Park KH. Optic disc hemorrhage in glaucoma: pathophysiology and prognostic significance. Curr opin ophthalmol. 2017;28:105-112
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Lee EJ, Han JC, Kee C. A novel hypothesis for the pathogenesis of glaucomatous disc hemorrhage. Prog in Retinal and Eye Res. 2017;60 20e43
- ↑ 9.0 9.1 Begg IS, Drance SM, Sweeney VP. Ischaemic optic neuropathy in chronic simple glaucoma. Br J Ophthalmol. 1971;55(2):73–90.
- ↑ Sonnsjö B, Krakau CE. Arguments for a vascular glaucoma etiology. Acta Ophthalmol (Copenh). 1993;71(4):433–444.
- ↑ Kurvinen L, Harju M, Saari J, Vesti E. Altered temporal peripapillary retinal flow in patients with disc hemorrhages. Graefes Arch. Clin. Exp. Ophthalmol. 2010;248(12):1771–1775.
- ↑ 12.0 12.1 Grieshaber MC, Terhorst T, Flammer J. The pathogenesis of optic disc splinter haemorrhages: a new hypothesis. Acta Ophthalmol Scand. 2006;84(1):62–68.
- ↑ 13.0 13.1 Golubnitschaja O, Yeghiazaryan K, Liu R, et al. Increased expression of matrix metalloproteinases in mononuclear blood cells of normal-tension glaucoma patients. J. Glaucoma. 2004;13(1):66–72.
- ↑ 14.0 14.1 14.2 Park HL, Kim JW, Park CK. Choroidal microvasculature drop‐out is associated with progressive retinal nerve fiber layer thinning in glaucoma with disc hemorrhage. Ophthalmology. 2018;125:1003–13.
- ↑ Cousins CC, Pan BX, Chou JC, et al. Densitometric profiles of optic disc hemorrhages in the ocular hypertension treatment study. American journal of ophthalmology. 2020;217:10-19
- ↑ Chou JC, Cousins CC, Miller JB, et al. Fundus densitometry findings suggest optic disc hemorrhages in primary open-angle glaucoma have an arterial origin. American journal of ophthalmology. 2018;187:108-116.
- ↑ 17.0 17.1 17.2 17.3 Jasty U, Harris A, Siesky B, et al. Optic disc haemorrhage and primary open-angle glaucoma: a clinical review. British Journal of Ophthalmology. 2020;104(11):1488-1491.
- ↑ 18.00 18.01 18.02 18.03 18.04 18.05 18.06 18.07 18.08 18.09 18.10 18.11 18.12 18.13 18.14 18.15 Healey PR, Mitchell P, Smith W, Wang JJ. Optic disc hemorrhages in a population with and without signs of glaucoma. Ophthalmology. 1998;105(2):216–223.
- ↑ 19.0 19.1 19.2 19.3 Jin C, Park GS, Kim KN, Song MY, Hwang YH. Comparison of posterior vitreous detachment-related and glaucomatous optic disc hemorrhage. Scientific Reports. 2023;13(1):5011.
- ↑ 20.0 20.1 20.2 20.3 20.4 Higashide T, Ohkubo S, Udagawa S, et al. Spatial and Temporal Relationship between Structural Progression and Disc Hemorrhage in Glaucoma in a 3-Year Prospective Study. Ophthalmology Glaucoma. 2020
- ↑ AIRAKSINEN PJ. Fellow eyes of glaucomatous patients with uniocular optic disc haemorrhage. Acta Ophthalmologica. 1981;59(2):231-236.
- ↑ Airaksinen PJ, Mustonen E, Alanko HI. Optic disc hemorrhages: analysis of stereophotographs and clinical data of 112 patients. Archives of ophthalmology. 1981;99(10):1795-1801.
- ↑ Ozturker ZK, Munro K, Gupta N. Optic disc hemorrhages in glaucoma and common clinical features. Canadian Journal of Ophthalmology. 2017;52(6):583-591.
- ↑ 24.0 24.1 Law SK, Choe R, Caprioli J. Optic disk characteristics before the occurrence of disk hemorrhage in glaucoma patients. Am. J. Ophthalmol. 2001;132(3):411–413.
- ↑ 25.0 25.1 Airaksinen PJ, Mustonen E, Alanko HI. Optic disc haemorrhages precede retinal nerve fibre layer defects in ocular hypertension. Acta Ophthalmol (Copenh). 1981;59(5):627–641.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 Sugiyama K, Tomita G, Kawase K, et al. Disc hemorrhage and peripapillary atrophy in apparently healthy subjects. Acta Ophthalmol Scand. 1999;77(2):139–142.
- ↑ 27.0 27.1 27.2 27.3 27.4 27.5 Yamamoto T, Iwase A, Kawase K, Sawada A, Ishida K. Optic disc hemorrhages detected in a large-scale eye disease screening project. J. Glaucoma. 2004;13(5):356–360.
- ↑ 28.0 28.1 28.2 28.3 Klein BE, Klein R, Sponsel WE, et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology. 1992;99(10):1499–1504.
- ↑ 29.0 29.1 Bengtsson B. Optic disc haemorrhages preceding manifest glaucoma. Acta Ophthalmol (Copenh). 1990;68(4):450–454.
- ↑ 30.0 30.1 30.2 30.3 Bengtsson B, Holmin C, Krakau CE. Disc haemorrhage and glaucoma. Acta Ophthalmol (Copenh). 1981;59(1):1–14.
- ↑ 31.0 31.1 Wang Y, Xu L, Hu L, et al. Frequency of optic disk hemorrhages in adult chinese in rural and urban china: the Beijing eye study. Am. J. Ophthalmol. 2006;142(2):241–246.
- ↑ Razeghinejad MR, Nowroozzadeh MH. Optic disk hemorrhage in health and disease. Survey of Ophthalmology. 2017;62(6):784-802.
- ↑ 33.0 33.1 Skaat A, De Moraes CG, Bowd C, et al. African Descent and Glaucoma Evaluation Study (ADAGES): racial differences in optic disc hemorrhage and beta-zone parapapillary atrophy. Ophthalmology. 2016;123(7):1476-1483.
- ↑ 34.0 34.1 Jonas JB, Iester M. Disc hemorrhage and glaucoma. Ophthalmology. 1995;102(3):365–366.
- ↑ 35.0 35.1 Kim Y, Han S, Park K, et al. Risk factors associated with optic disc haemorrhage in patients with normal tension glaucoma. Eye. 2010;24(4):567-572.
- ↑ 36.00 36.01 36.02 36.03 36.04 36.05 36.06 36.07 36.08 36.09 36.10 36.11 36.12 36.13 Budenz DL, Huecker JB, Gedde SJ, Gordon M, Kass M. Thirteen-year follow-up of optic disc hemorrhages in the ocular hypertension treatment study. Am. J. Ophthalmol. 2017;174:126-133.
- ↑ 37.0 37.1 37.2 37.3 37.4 37.5 37.6 Diehl DL, Quigley HA, Miller NR, Sommer A, Burney EN. Prevalence and significance of optic disc hemorrhage in a longitudinal study of glaucoma. Arch. Ophthalmol. 1990;108(4):545–550.
- ↑ 38.0 38.1 38.2 38.3 38.4 38.5 38.6 38.7 Kitazawa Y, Shirato S, Yamamoto T. Optic disc hemorrhage in low-tension glaucoma. Ophthalmology. 1986;93(6):853–857.
- ↑ Susanna R, Drance SM, Douglas GR. Disc hemorrhages in patients with elevated intraocular pressure. Occurrence with and without field changes. Arch. Ophthalmol. 1979;97(2):284–285.
- ↑ 40.0 40.1 Kim YK, Park KH, Yoo BW, Kim HC. Topographic Characteristics of Optic Disc Hemorrhage in Primary Open-Angle Glaucoma. Invest Ophthalmol Vis Sci. 2014;55:169–176.
- ↑ 41.0 41.1 Jonas JB, Xu L. Optic disk hemorrhages in glaucoma. Am. J. Ophthalmol. 1994;118(1):1–8.
- ↑ Airaksinen PJ, Heijl A. Visual field and retinal nerve fibre layer in early glaucoma after optic disc haemorrhage. Acta Ophthalmol (Copenh). 1983;61(2):186–194.
- ↑ Suh MH, Park KH. Period prevalence and incidence of optic disc haemorrhage in normal tension glaucoma and primary open-angle glaucoma. Clin. Experiment. Ophthalmol. 2011;39(6):513–519.
- ↑ Gloster J. Incidence of optic disc haemorrhages in chronic simple glaucoma and ocular hypertension. Br J Ophthalmol. 1981;65(7):452–456.
- ↑ 45.0 45.1 45.2 45.3 45.4 Soares AS, Artes PH, Andreou P, et al. Factors associated with optic disc hemorrhages in glaucoma. Ophthalmology. 2004;111(9):1653–1657.
- ↑ 46.0 46.1 46.2 Hwang YH, Kim YY, Kim HK, Sohn YH. Changes in retinal nerve fiber layer thickness after optic disc hemorrhage in glaucomatous eyes. J. Glaucoma. 2014;23(8):547–552.
- ↑ 47.0 47.1 47.2 Ernest PJ, Schouten JS, Beckers HJ, et al. An evidence-based review of prognostic factors for glaucomatous visual field progression. Ophthalmology. 2013;120(3):512–519.
- ↑ 48.0 48.1 48.2 Rasker MT, van den Enden A, Bakker D, Hoyng PF. Deterioration of visual fields in patients with glaucoma with and without optic disc hemorrhages. Arch. Ophthalmol. 1997;115(10):1257–1262.
- ↑ 49.0 49.1 49.2 49.3 49.4 Drance S, Anderson DR, Schulzer M, Collaborative Normal-Tension Glaucoma Study Group. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am. J. Ophthalmol. 2001;131(6):699–708.
- ↑ 50.0 50.1 50.2 50.3 Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch. Ophthalmol. 2003;121(1):48–56.
- ↑ Ahn JK, Kang JH, Park KH. Correlation between a disc hemorrhage and peripapillary atrophy in glaucoma patients with a unilateral disc hemorrhage. J. Glaucoma. 2004;13(1):9–14.
- ↑ Jonas JB, Martus P, Budde WM. Inter-eye differences in chronic open-angle glaucoma patients with unilateral disc hemorrhages. Ophthalmology. 2002;109(11):2078–2083.
- ↑ Lee JY, Sung KR, Shin JW, Kim KE, Kim JM. Reduced intradisc vessel density is associated with optic disc hemorrhage in eyes with primary open-angle glaucoma. Scientific Reports. 2023;13(1):1281.
- ↑ 54.0 54.1 Lee A, Shin JW, Lee JY, Baek MS, Kook MS. Optic disc hemorrhage is not associated with global choroidal vessel loss, but is associated with localized choroidal vessel loss in glaucoma. Journal of Clinical Medicine. 2022;11(4):1080.
- ↑ Rao HL, Sreenivasaiah S, Dixit S, et al. Choroidal microvascular dropout in primary open-angle glaucoma eyes with disc hemorrhage. Journal of glaucoma. 2019;28(3):181-187.
- ↑ Koh Y-Y, Lai C-C, Chen HS, Yeung L, Ku W-C, Chuang L-H. Optic disc hemorrhage in nonglaucomatous eyes: A cross-sectional study with average 8-year follow-up. PLoS One. 2020;15(8):e0237796.
- ↑ Nitta K, Sugiyama K, Wajima R, Tachibana G, Yamada Y. Associations between changes in radial peripapillary capillaries and occurrence of disc hemorrhage in normal-tension glaucoma. Graefe's Archive for Clinical and Experimental Ophthalmology. 2019;257:1963-1970.
- ↑ Nishida T, Moghimi S, David RCC, et al. Rates of circumpapillary retinal nerve fiber layer thinning and capillary density loss in glaucomatous eyes with disc hemorrhage. American journal of ophthalmology. 2022;235:24-31.
- ↑ 59.0 59.1 59.2 59.3 Furlanetto RL, De Moraes CG, Teng CC, et al. Risk factors for optic disc hemorrhage in the low-pressure glaucoma treatment study. Am. J. Ophthalmol. 2014;157(5):945–952.
- ↑ Wu X, Konieczka K, Liu X, et al. Role of ocular blood flow in normal tension glaucoma. Advances in Ophthalmology Practice and Research. 2022;2(1):100036.
- ↑ Jang M, Kim YK, Jeoung JW, Park KH. Analysis of variation in incidence of optic disc hemorrhage according to seasonal and temperature changes. American Journal of Ophthalmology. 2022;239:84-89.
- ↑ 62.0 62.1 62.2 Bengtsson B, Leske MC, Yang Z, Heijl A, EMGT Group. Disc hemorrhages and treatment in the early manifest glaucoma trial. Ophthalmology. 2008;115(11):2044–2048.
- ↑ 63.0 63.1 Jonas JB, Nangia V, Khare A, et al. Prevalence of optic disc hemorrhages in rural central India. the central India eye and medical study. PLoS One. 2013;8(9):e76154.
- ↑ 64.0 64.1 64.2 Tomidokoro A, Iwase A, Araie M, Yamamoto T, Kitazawa Y. Population-based prevalence of optic disc haemorrhages in elderly Japanese. Eye. 2009;23(5):1032-1037.
- ↑ Kim YK, Jeoung JW, Kim DM, Park KH. Prevalence of optic disc hemorrhage in Korea: the Korea National health and nutrition examination survey. Investigative Ophthalmology & Visual Science. 2015;56(6):3666-3672.
- ↑ 66.0 66.1 Kottler MS, Drance SM. Studies of hemorrhage on the optic disc. Can. J. Ophthalmol. 1976;11(2):102–105
- ↑ Drance SM, Fairclough M, Butler DM, Kottler MS. The importance of disc hemorrhage in the prognosis of chronic open angle glaucoma. Arch. Ophthalmol. 1977;95(2):226–228.
- ↑ 68.0 68.1 68.2 68.3 Grødum K, Heijl A, Bengtsson B. Optic disc hemorrhages and generalized vascular disease. J. Glaucoma. 2002;11(3):226–230.
- ↑ 69.0 69.1 Tuulonen A, Takamoto T, Wu DC, Schwartz B. Optic disk cupping and pallor measurements of patients with a disk hemorrhage. Am. J. Ophthalmol. 1987;103(4):505–511.
- ↑ Kim M, Kim T-W, Weinreb RN, Lee EJ, Seo JH. Spontaneous retinal venous pulsation and disc hemorrhage in open-angle glaucoma. Invest. Ophthalmol. Vis. Sci. 2014;55(5):2822–2826.
- ↑ 71.0 71.1 Shihab ZM, Lee PF, Hay P. The significance of disc hemorrhage in open-angle glaucoma. Ophthalmology. 1982;89(3):211–213.
- ↑ Poinoosawmy D, Gloster J, Nagasubramanian S, Hitchings RA. Association between optic disc haemorrhages in glaucoma and abnormal glucose tolerance. Br J Ophthalmol. 1986;70(8):599–602
- ↑ Lee JY, Kim JM, Shim SH, et al. Association between optic disc hemorrhage and renal function in South Korea. Journal of glaucoma. 2018;27(3):251-256.
- ↑ Heijl A. Frequent disc photography and computerized perimetry in eyes with optic disc haemorrhage: a pilot study. Acta Ophthalmologica. 1986;64(3):274-281.
- ↑ 75.0 75.1 de Beaufort HC, De Moraes CGV, Teng CC, et al. Recurrent disc hemorrhage does not increase the rate of visual field progression. Graefe's Archive for Clinical and Experimental Ophthalmology. 2010;248:839-844.
- ↑ Zhang L, Tang L, Xia M, Cao G. The application of artificial intelligence in glaucoma diagnosis and prediction. Frontiers in Cell and Developmental Biology. 2023;11:1173094.
- ↑ 77.0 77.1 Brown A, Cousins H, Cousins C, et al. Deep learning for localized detection of optic disc hemorrhages. American Journal of Ophthalmology. 2023.
- ↑ Ha A, Sun S, Kim YK, et al. Deep-learning-based enhanced optic-disc photography. Plos one. 2020;15(10):e0239913
- ↑ 79.0 79.1 79.2 79.3 Ishida K, Yamamoto T, Sugiyama K, Kitazawa Y. Disk hemorrhage is a significantly negative prognostic factor in normal-tension glaucoma. Am. J. Ophthalmol. 2000;129(6):707–714.
- ↑ Roy FH. Ocular differential diagnosis. [S.I.]: F.E.P. International; 2009.
- ↑ Katz B, Hoyt WF. Intrapapillary and peripapillary hemorrhage in young patients with incomplete posterior vitreous detachment. Signs of vitreopapillary traction. Ophthalmology. 1995;102(2):349–354.
- ↑ Roberts TV, Gregory-Roberts JC. Optic disc haemorrhages in posterior vitreous detachment. Aust N Z J Ophthalmol. 1991;19(1):61–63.
- ↑ 83.0 83.1 Shukla AG, Sirinek PE, De Moraes CG, et al. Disc hemorrhages are associated with the presence and progression of glaucomatous central visual field defects. Journal of glaucoma. 2020;29(6):429.
- ↑ 84.0 84.1 84.2 84.3 David RCC, Moghimi S, Do JL, et al. Characteristics of central visual field progression in eyes with optic disc hemorrhage. American journal of ophthalmology. 2021;231:109-119.
- ↑ Nitta K, Sugiyama K, Higashide T, Ohkubo S, Tanahashi T, Kitazawa Y. Does the enlargement of retinal nerve fiber layer defects relate to disc hemorrhage or progressive visual field loss in normal-tension glaucoma? Journal of glaucoma. 2011;20(3):189-195.
- ↑ Sung KR. Disc hemorrhage: is that a risk factor or sign of progression? Journal of glaucoma. 2012;21(4):275-276.
- ↑ Lee EJ, Kee HJ, Han JC, Kee C. Evidence-based understanding of disc hemorrhage in glaucoma. Survey of Ophthalmology. 2021;66(3):412-422.
- ↑ 88.0 88.1 Gracitelli CPB, Tatham AJ, Zangwill LM, et al. Estimated rates of retinal ganglion cell loss in glaucomatous eyes with and without optic disc hemorrhages. PLoS ONE. 2014;9(8):e105611.
- ↑ 89.0 89.1 Heijl A, Bengtsson B, Hyman L, Leske MC, Early Manifest Glaucoma Trial Group. Natural history of open-angle glaucoma. Ophthalmology. 2009;116(12):2271–2276.
- ↑ Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol. 2001;45(4):265–315.
- ↑ Ritch R, Schlötzer-Schrehardt U, Konstas AGP. Why is glaucoma associated with exfoliation syndrome? Prog Retin Eye Res. 2003;22(3):253–275.
- ↑ Vesti E, Kivelä T. Exfoliation syndrome and exfoliation glaucoma. Prog Retin Eye Res. 2000;19(3):345–368.
- ↑ Holló G, Quaranta L, Cvenkel B, et al. Risk factors associated with progression in exfoliative glaucoma patients. Ophthalmic Res. 2012;47(4):208–213.
- ↑ 94.0 94.1 94.2 94.3 Miyake T, Sawada A, Yamamoto T, et al. Incidence of disc hemorrhages in open-angle glaucoma before and after trabeculectomy. J. Glaucoma. 2006;15(2):164–171.
- ↑ 95.0 95.1 95.2 95.3 Hendrickx KH, van den Enden A, Rasker MT, Hoyng PF. Cumulative incidence of patients with disc hemorrhages in glaucoma and the effect of therapy. Ophthalmology. 1994;101(7):1165–1172.
- ↑ Airaksinen PJ. Are optic disc haemorrhages a common finding in all glaucoma patients? Acta Ophthalmol (Copenh). 1984;62(2):193–196.