All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Coats disease is a telangiectatic neovascular disease of the retina of unknown etiology that frequently affects unilateral eyes of young males.
George Coats[1] in 1908 described the histopathological features of enucleated eyes with massive exudation. He divided the morphology into 3 groups:
"Group I demonstrated massive subretinal exudate alone,
group II consisted of eyes with massive subretinal exudate, intra and subretinal hemorrhage, and retinal vascular dilatations, and
group III included eyes with subretinal exudate and retinal arteriovenous malformations."[2] Later, Von Hippel recognized group 3 as a separate entity called angiomatosis retinae.
A large study of 117 patients[3] took the definition of Coats disease as 'idiopathic retinal telangiectasia and intraretinal or subretinal exudation without appreciable signs of vitreoretinal traction.'
Disease Entity
Coats disease is usually characterized by unilateral (95%), progressive development of abnormal vessels in the retina of the affected individuals. It’s more frequent in males (at least 3:1) than females, and in patients younger than 8 years old, even though it has been observed in infants as well as older patients.
Other names
Leber's miliary aneurysm is considered to be a milder variant of the Coats disease, which usually does not have massive subretinal exudation, hemorrhage or exudative retinal detachment. Type 1 idiopathic macular telegiectasia is now considered the same disease as Coats disease.[2]
Disease
The disease is primarily due to aneurysms and telangiectatic vessels. The usual location of these vessels is within the temporal retina. These abnormal vessels are leaky and there is exudation in various degrees.
Genetics
No genetic basis has been found but there has been described chromosomal instability in chromosomes 3 and 13.
Other genes which have been implicated include:
- NDP (Norrie disease protein)
- CRB1
- PANK2
Associations
Coats like response has been noted in cases in patients with Turner Syndrome (XO), Senior Loken Syndrome, retinitis pigmentosa (both syndromic and isolated), facioscapulohumeral dystrophy (FSHD), and Linear Scleroderma/ Parry Romberg Syndrome. Especially in females, bilateral involvement and FSHD should be ruled out.
Diagnosis
Signs and Symptoms
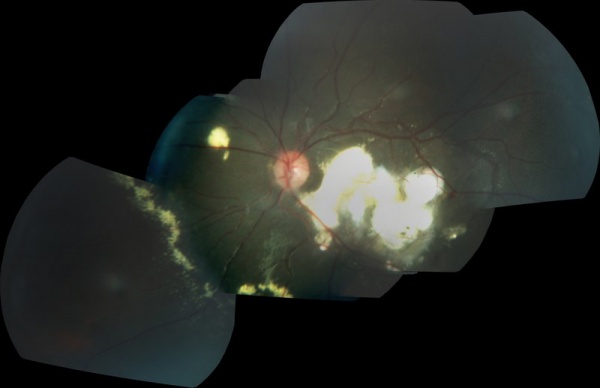
In a large study[4] on 150 patients, 'the most common referral diagnoses were Coats disease in 64 cases (41%) and retinoblastoma in 43 (27%). The first symptom or sign was decreased visual acuity in 68 cases (34%), strabismus in 37 (23%), leukocoria in 31 (20%), and 13 patients (8%) were asymptomatic. Visual acuity at presentation was 20/200 to no light perception in 121 eyes (76%). The anterior segment was normal in 142 eyes (90%). The retinal telangiectasia involved the midperipheral or peripheral fundus in 156 of the 158 eyes (99%) and was restricted to the macular area in two eyes (1%); involved mainly the temporal fundus in 66 eyes (42%), inferior fundus in 41 eyes (26%), and more than one sector in 34 eyes (22%). Retinal exudation was present in all 12 clock hours in 86 eyes (55%) and six or more clock hours in 115 eyes (73%). There was a total retinal detachment in 74 eyes (47%) and neovascular glaucoma in 12 (8%). Retinal macrocysts were present in 18 eyes (11%), a vasoproliferative tumor in nine eyes (6%) and retinal neovascularization in four eyes (3%). Fluorescein angiography in 49 of the 158 eyes (37%) disclosed early hyperfluorescence of the telangiectasias and macular edema in 18 of eyes (37%). Ultrasonography typically showed a retinal detachment but no solid mass'
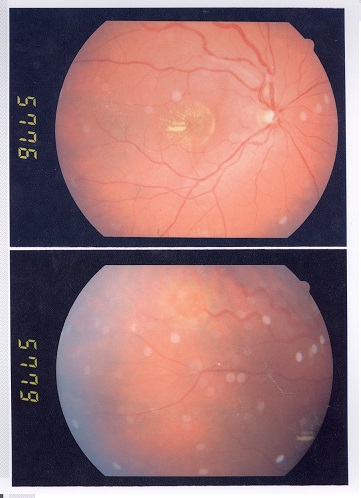
In mild cases one or two foci of retinal telangiectasia can be found usually on the temporal hemispheres. Microaneurysms, and thickening of retinal vessels are seen. Affected vessels show irregular enlargement with aneurysms which light up like bulb during fluorescein angiogram. The vascular abnormalities are usually prominent near the peripheral capillary dropout. The vascular leakage causes hard exudates which may be peripheral (near the vascular abnormalities) or mid peripheral and central (at macula). In type 1 macular telangiectasia, the telangiectasia and aneurysm with hard exudates (primarily cholesterol) are seen temporal to the fovea. Intraretinal or subretinal fluid/exudate may be noted at the macula.
The exudates vary in size and they have a tendency to occupy the inferior pole, as a result, visual acuity is reduced primarily due to infiltration of the fovea, formation of cystoid macular edema or even exudative retinal detachment. Those exudates ultimately cause discoid glial scarring and subretinal neo-vascularization. Long standing subretinal exudate may cause superficial crystalline deposits. The retinal vessels overlying the subretinal exudates may undego gliotic sheating. Retinal pigment epithelial metaplasia with subretinal fibrosis may be noted. Retinal neovascularization is uncommon, but can occur in late stages.
The anterior segment is usually not involved in early cases, but late cases may cause neovascularization of the iris or angle of anterior chamber, ectropion uvae, or neovascular glaucoma.
In children, the exudative detachment may be bullous, immobile and touching the posterior capsule of the lens. The irregular caliber of telangiectatic vessels, aneurysms, subretinal exudates and lack of calcification on ultrasound differentiates it from retinoblastoma.
Representative cases are presented at https://webeye.ophth.uiowa.edu/eyeforum/cases/100-Coats-Disease.htm
and https://webeye.ophth.uiowa.edu/eyeforum/cases/237-Coats-Disease.htm
Clinical diagnosis
Besides thorough fundoscopy, which ultimately establishes the diagnosis, several clinical tests may be utilized. The diagnostic tests include OCT, ultrasound, and fluorescence angiography.
Fluorescein angiogram
The features include
- telangiectatic vessels
- aneurysms appearing like light bulbs
- early and progressive perivascular leakage
- peripheral capillary nonperfusion
Staging
Two useful staging systems include those developed by Comez-Morales and by Siegelman.
Gomez- Morales Staging
Stage I: Focal exudates
Stage II: Massive exudation
Stage III: Partial exudative retinal detachment
Stage IV: Total Retinal Detachment
Stage V: Complications
Sigelman Staging
Stage I: Only telangiactasia
Stage II: Focal exudates
Stage III: Partial exudative retinal detachment
Stage IV: Total Retinal Detachment
Stage V: Complications
Shields' classification (usually followed)[3]
Stage 1: Retinal telangiectasia only
Stage 2: Telangiectasia and exudation
A. Extrafoveal exudation
B. Foveal exudation
Stage 3: Exudative retinal detachment
A. Subtotal detachment 1. Extrafoveal 2. Foveal
B. Total retinal detachment
Stage 4: Total retinal detachment and glaucoma
Stage 5: Advanced end-stage disease
Differential diagnosis
The major clinical significance of Coats Disease is to differentiate it from retinoblastoma since both appear with leukocoria, but calcium seen on CT or ultrasound excludes Coats in favor of retinoblastoma. Other conditions such as Toxocara infection, retinopathy of prematurity, pars planitis, familial exudative vitreoretinopathy, retinal metastatic lesions, Norrie disease, Eales disease, cavernous retinal hemangioma and leukemia, should be considered. A retinal vasoproliferative tumor is differentiated by presence of feeder and draining vessels, an obvious vascular mass, preretinal fibrosis and extreme peripheral location.
| Feature | Coats Disease | Retinoblastoma |
|---|---|---|
| Presentation | Older patient, Unilateral, Male | Younger presentation, Maybe bilateral, Unisex |
| Leukocoria | Grey to pink | White |
| Telangiectasia | Classic, Vessels can be traced | With tumor infiltration, Vessels dip into the mass |
| Vitreous seeding | Absent | Maybe present |
| Calcification | Not a feature | Seen on USG, CT Scan |
| Intraocular mass | Not a feature | Seen in endophytic cases |
| FFA | Leaks with telangiectatic vessels | Double circulation |
Management
Treatment
Observation- In minimal telangiectatic vessels with little or no exudation and no imminent threat to vision, or in painless and comfortable blind eyes
Laser treatment (low power, long duration, large spot burns to the telangiectatic vessels and aneurysms, also laser the peripheral capillary nonperfusion as per scatter laser settings) - in telangiectasia with exudation but no or minimal subretinal fluid
Cryotherapy- for exudation with subretinal fluid of such thickness that cryo reaction can reach the retina
Vitreoretinal surgery- for extensive retinal detachment not allowing cryo or laser.
Enucleation - Painful blind eye or when retinoblastoma can not be ruled out by imaging and clinical examination
Anti-VEGF therapy- has been promising but the safety profile for children is as of yet unclear.
Intravitreal triamcinolone acetonide- may reduce the exudation, but risks of glaucoma and cataract exist.
Prognosis
The prognosis depends on the extent of the disease with milder, older presenting cases, having a better prognosis, of even spontaneous regression, whereas children under the age of three have a poorer prognosis.
In the study the Shields and colleagues[3] on 150 patients 'anatomical improvement or stability was achieved in 76% of eyes,
and final visual acuity was 20/50 or better in 17 eyes
(14%), 20/60 to 20/100 in eight (6%), 20/200 to finger
counting in 30 (24%), and hand motion to no light
perception in 49 (40%) Enucleation was ultimately
necessary in 20 eyes (16%).
Risk factors predictive of poor visual outcome (20/200
or worse) included postequatorial (P 5 .01), diffuse
(P 5 .01), or superior (P 5 .04) location of the
telangiectasias and exudation, failed resolution of subretinal
fluid after treatment (P 5 .02), and presence of
retinal macrocysts (P 5 .02). The main risk factors for
enucleation were elevated intraocular pressure (greater
than 22 mm Hg; P less than or equal to .001) and iris
neovascularization (P less than or equal to .001).'
Additional Resources
- AAPOS Resource http://www.aapos.org/terms/conditions/34
- Information for parents http://www.coatsdisease.org/index.html
- Office of rare diseases on Coats disease http://rarediseases.info.nih.gov/gard/6121/coats-disease/resources/1
- Nikolaos Tr Stagkos, Kliniki Ophthalmologia, Thessaloniki- Greece, Aristotelian University Press,2002.
- American Academy of Ophthalmology. Pediatric Ophthalmology and Strabismus BCSC, Leo, 2011-2012.
- Jack J. Kanski- Brad Bowling, Clinical Ophthalmology- A systematic approach, Seventh Edition, Elsevier, 2011.
- Hoyt and Taylor, Pediatric Ophthalmology and Strabismus, fourth edition, Eslevier, 2012.
References
- ↑ Coats G. Forms of retinal diseases with massive exudation. R Lond Ophthalmol Hosp Rep. 1908;17:440-525
- ↑ Jump up to: 2.0 2.1 Sigler EJ, Randolph JC, Calzada JI, Wilson MW, Haik BG. Current management of Coats disease. Surv Ophthalmol. 2014 Jan-Feb;59(1):30-46. doi: 10.1016/j.survophthal.2013.03.007. Epub 2013 Oct 15. Review. PubMed PMID:24138893.
- ↑ Jump up to: 3.0 3.1 3.2 Shields JA, Shields CL, Honavar SG, Demirci H, Cater J. Classification and management of Coats disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001 May;131(5):572-83. PubMed PMID: 11336931.
- ↑ Shields JA, Shields CL, Honavar SG, Demirci H. Clinical variations and complications of Coats disease in 150 cases: the 2000 Sanford Gifford Memorial Lecture. Am J Ophthalmol. 2001 May;131(5):561-71. PubMed PMID: 11336930.