Zonulopathy: Evaluation and Surgical Management
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
2016/2017 ICD-10 Codes
No specific ICD 10 code exists for “Zonulopathy” or synonymous terminology, however associated findings may be used for coding purposes. Examples include:
- H27.10 Dislocation of lens, unspecified
- H25.89 Other age-related cataract (has taken place of pseudoexfoliation of lens capsule from ICD 9)
- Note that for clinical application, a laterality modifier should be included.
Disease
Zonulopathy is a state in which there is a deficiency of zonular support for the lenticular capsule. Zonulopathy may include malposition of the lens (subluxation or dislocation), though in many cases no malposition may be present.
Synonymous Terminology:
- Zonular Dehiscence
- Zonular Dialysis
Etiology
Etiology for zonulopathy include pseudoexfoliation syndrome, traumatic zonulysis, iatrogenic zonulysis (cataract extraction, pars plana vitrectomy, repeat intravitreal injections), ultra-brunescent cataracts, retinitis pigmentosa, aniridia, advanced age, intraocular neoplasm and systemic syndromes including Marfan syndrome, homocystinuria, Weill-Marchesani syndrome and Ehlers-Danlos syndrome. See EyeWiki article on Ectopia Lentis for complete discussion on systemic causes of zonulopathy.
Pathophysiology
The zonular fibers, also known as the zonular apparatus or zonule of Zinn, originate from the basal laminae of the nonpigmented epithelium of the ciliary body, and insert into the lens capsule at the equatorial region. The fibers insert 1.5mm anterior to the equator and 1.25 mm posterior, and are 5-30 um in diameter.[1] Approximately 140 fiber bundles make up the zonular apparatus, with a key component of the fibers being fibrillin, a connective tissue glycoprotein that provides strength and elasticity to the fibers. Fibrillin is coded by the FBN1 gene, which is anomalous in Marfan syndrome resulting in poor zonular stability and lens subluxation.
Diagnosis
- Zonulopathy is a clinical diagnosis that may be suspected due to the patient’s history, but should be carefully evaluated for prior to any lens surgery.
History
History may be useful in directing the ophthalmologist’s examination towards subtle findings that may otherwise be missed. A history of trauma, systemic disorder or family history should be elicited prior to cataract surgery.
Most patients are often asymptomatic, though in cases of significant subluxation or dislocation patients may experience fluctuation of their vision as the pupil dilates and constricts or as the lens shifts position within the eye. Primary symptoms include blurry vision, visual distortion, or monocular diplopia.
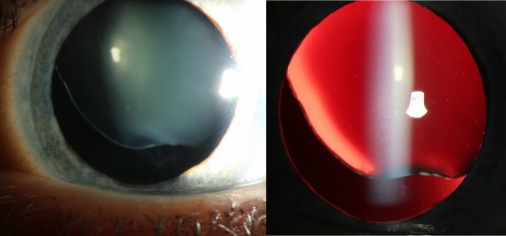
Physical examination
Physical examination of patients with a history concerning for zonulopathy as well as in all patients undergoing evaluation for cataract surgery should include visual acuity, objective and manifest refraction, and a focused slit lamp examination. The slit lamp biomicroscopy should be carefully performed with attention to lenticular centration or malposition, iris transillumination defects, pseudoexfoliation material on the anterior lens capsule or pupil margin, or phacodonesis. In cases of identified zonular dehiscence, it is important to identify both the number of clock hours involved and severity of the dehiscence as this will determine the approach to surgical repair.[2]
Despite an experienced clinician’s best efforts to identify subtle findings of zonulopathy, it is often not until the patient is in the operating room that intraoperative tissue and fluid dynamics reveal underlying zonular instability. For this reason it is imperative that all anterior segment surgeons be comfortable identifying and managing zonulopathy in the operative setting.
Management
Prior to Surgery
In surgical planning for patients with clinically evident zonulopathy or high suspicion for zonular deficiency, it is important to plan for all possible situations that may arise intraoperatively. This includes having all tools and hardware potentially required, available in the OR at the time of surgery. Additionally, eyes that have zonular deficiency often times have ocular comorbidities such has glaucoma or poor mydriasis as in the case of pseudoexfoliation syndrome. Pupillary dilation and maintenance of dilation can be optimized during surgery by providing pre-operative topical NSAIDs.[3]
Surgical Intervention
Considerations for Surgical Technique
Capsulorhexis
Performing a continuous curvilinear capsulorhexis (CCC) may be challenging in cases of zonular deficiency due to the abnormal vector forces created by areas of decreased or absent counter-traction. If difficulty is encountered initiating a capsular tear, an attempt should be made to direct shearing forces toward the area of zonulopathy so counter-forces are available in regions of intact zonules.[4] If the location of zonular loss does not lend itself to this technique, the surgeon may find benefit providing a point of fixation on the central lens capsule with a second instrument through the side port incision.[5]
Due to the challenging nature of creating a CCC with poor zonular support, the surgeon must be prepared to handle a rhexis that trends towards tearing out. The Little capsulorhexis tear-out rescue maneuver introduced by Brian Little in 2006 has become a powerful tool for preventing extension of capsular tears.[6] Ample viscoelastic should be used to gently counterbalance outward forces on the anterior capsule, though care must be taken to not over-inflate the anterior chamber.
Hydrodissection & Rotation
Excellent cortical cleaving hydrodissection as described by Howard Fine in 1992 is a key step in mobilizing the lens within the capsular bag so as to minimize stress on the intact zonular fibers during lens rotation and nuclear disassembly.[7] A variety of cannula are available for this maneuver, though a surgeon should default to the equipment with which he or she is most comfortable. Lens rotation can be difficult when there is compromised zonular support despite adequate hydrodissection. A bimanual technique for lens rotation may be employed to reduce the forces placed on the capsule. If significant zonular laxity is identified at this point in the case, it is often safest to place capsular support hooks prior to attempting nuclear disassembly and removal.
Nuclear Disassembly
Many techniques exist for nuclear fragmentation and phacoemulsification, each with strengths and weaknesses. Surgeons often have a preferred method for routine cataract extractions, though some of these techniques may be excessively vigorous or traumatic for an eye with zonulopathy. An alternative technique for nuclear disassembly in cases of zonular weakness or at-risk patients may be appropriate for some surgeons.
Employing a surgical technique that minimizes lens manipulation and rotation may decrease the risk of extending zonular dialysis. The “cross chop” technique described by Dooho Brian Kim is one rotationless horizontal chop technique can be used to divide the lens. Following an initial horizontal chop, a second subdivision is created without spinning the lens by reaching across the phaco instrument to form an “X” with the instruments, subsequently performing a second horizontal chop. After removing the two quadrants, the remaining hemilens can be safely removed as well (https://eyewiki.org/Zero-Min-Spin_Technique).[8] Other techniques for minimizing stress on zonules during nuclear division and removal such as the “double chop” method[9], though standard nuclear disassembly techniques may be performed without significant zonular stress when properly performed by a skilled surgeon.
Cortical Removal
Irrigation and aspiration (I/A) with either a coaxial or bimanual technique can apply significant centripetal force on the capsular bag which transmits to the zonular apparatus and may result in iatrogenic zonulysis. Using a tangential stripping technique, inducing a force perpendicular to the radial fibers can minimize the strain on zonules and decrease the risk of creating or extending a dialysis. The method for tangential I/A described as the “hurricane cortical aspiration technique” was introduced by Nakano et al in 2014, in which they demonstrated the reduced forces created by tangential cortical stripping in cadaver eye video analysis.[10] The technique can be an excellent tool for not only eyes with zonulopathy but is an efficient method for cortical removal in routine cataract cases as well.
In cases of severe diffuse zonular laxity and high risk for zonular dialysis in older patients, a new technique of “central cortical cleanup” has been suggested to leave a central clear visual axis while avoiding stress to the peripheral normally encountered during complete cortical removal. Mansour et al in 2016 uses a bimanual technique, elevating central cortical fibers and aspirating them toward the periphery.[11] Patients selected for this technique were over the age of 90 as a more complete cortical cleanup and definitive treatment of zonulopathy would likely be more appropriate for younger patients with greater longevity.
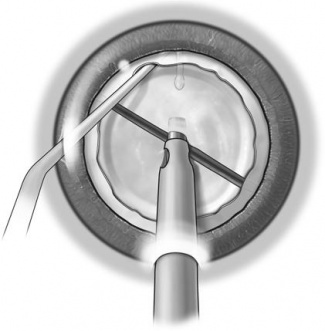
Capsular Hooks
Capsular hooks (aka capsule retractors) are modified nylon iris hooks which are used to provide support to the unsteady capsule during phacoemulsification in cases of severe zonular instability. They differ from iris hooks in the “looped” shape of the supporting end which distributes the force placed on the capsule over a larger area, thereby decreasing the risk of tearing the anterior capsule. These modified iris retractors may be inserted through limbal incisions or posterior to the limbus in an orientation that is parallel to the iris in order to minimize anterior tenting of the iris.[12] Capsular hooks are easily inserted and removed, making them excellent tools for decreasing risk of complications due to an unstable capsular bag.[13],[14]
One potential complication that has been reported in cases CTR placement in capsular bags being supported by hooks is inadvertent threading of the CTR through the capsular retractor loop. Should this situation occur, the surgeon can free the incarcerated CTR by cutting the retractor loop with lens cutting scissors.[15]
Video 1: Removal of PXF Cataract. Zonular laxity was identified as phacodonesis preoperatively in this patient with pseudoexfoliation syndrome. Capsular hooks are inserted and used to stabilize the loose capsular bag during nuclear removal. A CTR and in-the-bag IOL are placed prior to case completion. Credit: Brandon Ayres, MD
Capsular Tension Rings
Capsular Tension Rings (CTR) are inserted into the capsular bag during cataract surgery for supporting areas of zonular laxity and maintaining shape of the bag. The tool is now widely used as an integral step in cases where there is a loss of zonular integrity.[16] The device is an open polymethyl methacrylate (PMMA) ring with eyelets on either end and comes in sizes from approximately 12 to 14.5 mm diameter, and compresses approximately 2 mm when placed into the capsular bag. CTRs have been shown to be effective in treating zonular dialysis of up to 150 degrees.[17],[18],[19]
Contraindications to CTR placement are anterior capsular tear, discontinuous capsulorhexis, posterior capsule tear, and capsular bags with severe zonulopathy and no plan for scleral fixation. Potential complications of CTR implantation may include anterior or posterior capsular tear, extension of existing tear or zonular dialysis, entrapment of intraocular lens haptic or inadvertent sulcus placement.[16]
Timing of CTR implantation during the course of cataract extraction provides the least trauma to zonules and the capsular bag after removal of the crystalline lens. Early implantation of a CTR is occasionally necessary prior to lens removal, however this has been shown to have significant stress on the zonules with large displacement of the lens during implantation.[20] As an alternative, implantation of a capsular tension segment may be done in a far more atraumatic way, and may be the superior option when early support is indicated.[20]
Several strategies have been proposed to minimize stress to intact zonules and minimize the risk of extending zonular dialysis during CTR implantation. Angunawela and Little described a “fishtail” method for insertion of the CTR in a bent fashion through a 2.8 mm incision, though this resulted in overbending in some cases, particularly in smaller incisions.[21] A modified “fishtail on a line” technique was introduced by Jordan Rixen and Thomas Oetting which minimized the risk of overbending.[22] A new technique of “suture-guided CTR placement” was introduced by Timothy Page involving a 10-0 nylon through the leading eyelet, guiding implantation of the CTR while being introduced into the eye through a traditional CTR inserter method.[23]
Some have suggested placing capsular tension rings prophylactically in pseudoexfoliation patients, should they have progressive zonulopathy and late presentation of IOL subluxation. In this situation, a CTR will be available for suturing the IOL in-the-bag to the scleral wall.[24]
Henderson CTR
In some cases of severe zonulopathy it may be necessary for early implantation of the CTR. This can present a few unique challenges as nuclear and cortical material may become incarcerated under the CTR making removal of residual lens difficult. The Henderson CTR was designed with a series of 8 scalloped depressions that allow for improved removal of remaining lens fragments. This CTR is also composed of PMMA and is inserted in the same fashion as traditional capsular rings.[25]
Cionni Ring – Modified CTR
In situations of profound zonular loss, scleral fixation may be necessary to stabilize the location and orientation of the capsular bag. The Cionni CTR was developed by Robert J Cionni and Robert Osher as a way to secure the CTR directly to the scleral wall without violating the capsular bag. The standard CTR is modified to include one or two fixation eyelets on angled hooks through which suture can be passed and tied into the sclera, anterior to the capsulotomy. The same task may also be completed in two steps with implantation of a traditional CTR along with a sutured capsular segment as described below. It should be noted that the Cionni ring carries the advantage of accomplishing both goals of capsular support and scleral fixation in a single step. The Cionni ring is inserted manually with a hand-over-hand technique or with a standard CTR inserter.
Capsular Tension Segments
The capsular tension segment (CTS) was introduced by Iqbal Ike Ahmed in 2002 as a method for re-centering subluxed lenses and providing optimal intraoperative and long-term support to in-the-bag IOL implantation. This PMMA device covers 120 degrees of the capsular fornix with an anteriorly placed fixation eyelet for suturing to the scleral wall.[2] One of the principle advantages of the device is the ability to insert into the capsular bag and provide support prior to removal of the crystalline lens. During early implantation, an iris hook can be inserted through the eyelet to provide capsular support until the lens can be removed and the CTS is safely sutured into proper position.
Hoffman Pockets
Scleral fixation through suturing previously required a conjunctival dissection and manipulation of suture to bury the knot and prevent exposure. One method for bypassing these steps was introduced by Hoffman in 2006. The “Hoffman Pocket” is a technique which two scleral pockets are dissected posteriorly from the limbus 180 degrees apart.[26] Prolene or gortex sutures are passed through the eyelet of the capsular support device before being passed through the sclera within the boundaries of the scleral pocket dissection. Needles are removed and the suture is externalized through the pocket using a Sinsky hook or similar tool. The suture can then be tied within the pocket, taking care not to over-tighten the knot, and loose suture ends are trimmed. Note that the 3 and 9 o’clock positions are spared in order to avoid the long ciliary vessels. The procedure caries the advantages of improved post-operative comfort, rapid healing time, and reduced risk of suture exposure.
Video 2: Cataract extraction in a patient with severe zonular laxity and lens subluxation. A manual approach to re-centration of the crystalline lens prior to nuclear removal, CTR implantation, and Ahmed capsular segment implantion with gortex sutures secured through Hoffman pockets. Credit: Brandon Ayres, MD
Femtosecond Laser Assisted Cataract Surgery (FLACS)
The femtosecond laser was developed as a way to improve the overall predictability, safety and standardization of routine cataract surgeries. Though it has not been proven to significantly improve outcomes in most cataract surgeries, it may have a roll in improving the safety of several steps in cases of zonulopathy or lens subluxation.[27] Chee et al demonstrated a greater than 90% success rate at retaining the capsular bag with intracapsular IOL implantation using FLACs for capsulotomy and nuclear softening in subluxed lenses with at least 6 clock hours of zonular weakness.[28] In a separate case series, four eyes in two patients with Marfan syndrome were successfully treated with FLACS, showing the ability to treat mild, moderate and severe cases of lens subluxation with the femtosecond laser.[29] When available, femtosecond laser systems may be a helpful tool improving safety and success in lenses with loss of zonular support.
Video 3: Bringing it all together. In this surgical video by Brandon Ayres, MD, FLACS is performed on a subluxed lens in a patient with Marfan syndrome. Capsule hooks, CTR, and sutured Ahmed capsular segment are used for stability while a toric lens is placed in the capsular bag.
Intraocular Lens Selection
IOL selection depends on the degree of zonulopathy and planned surgical approach. Options include in-the-bag IOL with capsular support devices, sulcus IOL with or without optic capture, anterior chamber IOL, iris fixated IOL, scleral sutured IOL, or glued IOL.[30] A plan should be identified based on the pre-operative evaluation and degree of suspected zonular compromise, but the surgeon must have a “plan B” and be flexible as often times the full extent of zonulopathy isn’t identified until in the operating room.
Special Considerations Regarding Anaesthesia
Topical anaesthesia should be avoided in patients with zonular weakness because operation time in those patients is expected to be longer than straight forward routine cases.
Finally, "NOT ONLY THE ZONULES YOU HAVE TO WORRY ABOUT"!
Certain diseases that cause zonulopathy are associated with considerable risk during general anaesthesia, for example in homocysteinuria there is a risk of thromboembolic events if hydration was not strictly controlled. Nitrous oxide was avoided as it inhibits the enzyme methionine synthase and leads to elevation of of homocysteine levels. Marfan syndrome is associated with increased risk of aortic dissection as well as other considerations regarding difficult intubation and TM (temporomaxillary) joint dislocation.
References
- ↑ Sharon L. Jick, MD. in Section 11: Lens and Cataract 244 (American Academy of Ophthalmology).
- ↑ Jump up to: 2.0 2.1 Hasanee, K. & Ahmed, I. I. K. Capsular tension rings: update on endocapsular support devices. Ophthalmol. Clin. N. Am. 19, 507–519 (2006).
- ↑ Gimbel, H. V. The effect of treatment with topical nonsteroidal anti-inflammatory drugs with and without intraoperative epinephrine on the maintenance of mydriasis during cataract surgery. Ophthalmology 96, 585–588 (1989).
- ↑ Por, Y. M. & Lavin, M. J. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv. Ophthalmol. 50, 429–462 (2005).
- ↑ Cataract Surgery: Technique, Complications, and Management (ed. T.F. Neuhann) 134–142 (W.B. Saunders Co, 1995)
- ↑ Little, B. C., Smith, J. H. & Packer, M. Little capsulorhexis tear-out rescue. J. Cataract Refract. Surg. 32, 1420–1422 (2006).
- ↑ Fine, I. H. Cortical cleaving hydrodissection. J. Cataract Refract. Surg. 18, 508–512 (1992).
- ↑ Kim, D. B. Cross chop: Modified rotationless horizonal chop technique for weak zonules. J. Cataract Refract. Surg. 35, 1335–1337 (2009).
- ↑ Kim, D. B. Double-chop: Modified-chop technique eliminating ultrasonic energy and vacuum for lens fragmentation. J. Cataract Refract. Surg. 42, 1402–1407 (2016).
- ↑ Nakano, C. T. et al. Hurricane cortical aspiration technique: One-step continuous circular aspiration maneuver. J. Cataract Refract. Surg. 40, 514–516 (2014).
- ↑ Mansour, A. M., Antonios, R. S. & Ahmed, I. I. K. Central cortical cleanup and zonular deficiency. Clin. Ophthalmol. Auckl. NZ 10, 1919–1923 (2016).
- ↑ Lee, V. & Bloom, P. Microhook capsule stabilization for phacoemulsification in eyes with pseudoexfoliation-syndrome-induced lens instability. J. Cataract Refract. Surg. 25, 1567–1570 (1999).
- ↑ Sati, A., Shankar, S., Gurunadh, V. S. & Sangwan, V. S. Iris retractors: the saviours in cataract surgery for cataract in lens coloboma. BMJ Case Rep. 2013, (2013).
- ↑ Sethi, H. S., Sinha, A., Pal, N. & Saxena, R. Modified flexible iris retractor to retract superior iris and support inferior capsule in eyes with iris coloboma and inferior zonular deficiency. J. Cataract Refract. Surg. 32, 715–716 (2006).
- ↑ Grove, K., Condon, G., Erny, B. C., Chang, D. F. & Kim, T. Complication from combined use of capsule retractors and capsular tension rings in zonular dehiscence. J. Cataract Refract. Surg. 41, 2576–2579 (2015).
- ↑ Jump up to: 16.0 16.1 Randleman, J. B. & Ahmed, I. I. K. Intraocular Lens Surgery: Selection, Complications, and Complex Cases. (Thieme, 2016).
- ↑ Jacob, S. et al. Efficacy of a capsular tension ring for phacoemulsification in eyes with zonular dialysis. J. Cataract Refract. Surg. 29, 315–321 (2003).
- ↑ Gimbel, H. V., Sun, R. & Heston, J. P. Management of zonular dialysis in phacoemulsification and IOL implantation using the capsular tension ring. Ophthalmic Surg. Lasers 28, 273–281 (1997).
- ↑ Price, F. W. et al. Interim results of the United States investigational device study of the Ophtec capsular tension ring. Ophthalmology 112, 460–465 (2005).
- ↑ Jump up to: 20.0 20.1 Ahmed, I. I. K., Cionni, R. J., Kranemann, C. & Crandall, A. S. Optimal timing of capsular tension ring implantation: Miyake-Apple video analysis. J. Cataract Refract. Surg. 31, 1809–1813 (2005).
- ↑ Angunawela, R. I. & Little, B. Fish-tail technique for capsular tension ring insertion. J. Cataract Refract. Surg. 33, 767–769 (2007).
- ↑ Jordan J. Rixen & Oetting, T. A. Fishtail on a line technique for capsular tension ring insertion. J. Cataract Refract. Surg. 40, 1068–1070 (2014).
- ↑ Page, T. P. Suture-guided capsular tension ring insertion to reduce risk for iatrogenic zonular damage. J. Cataract Refract. Surg. 41, 1564–1567 (2015).
- ↑ Stephenson, M. Keys to Managing Weak Zonules. Review of Ophthalmology Available at: https://www.reviewofophthalmology.com/article/keys-to-managing-weak-zonules. (Accessed: 30th November 2016)
- ↑ Henderson, B. A. & Kim, J. Y. Modified capsular tension ring for cortical removal after implantation. J. Cataract Refract. Surg. 33, 1688–1690 (2007).
- ↑ Hoffman, R. S., Fine, I. H. & Packer, M. Scleral fixation without conjunctival dissection. J. Cataract Refract. Surg. 32, 1907–1912 (2006).
- ↑ Feldman, B. H. Femtosecond laser will not be a standard method for cataract extraction ten years from now. Surv. Ophthalmol. 60, 360–365 (2015).
- ↑ Chee, S.-P., Wong, M. H. Y. & Jap, A. Management of Severely Subluxated Cataracts using Femtosecond Laser Assisted Cataract Surgery. Am. J. Ophthalmol. (2016). doi:10.1016/j.ajo.2016.09.021
- ↑ Crema, A. S., Walsh, A., Yamane, I. S., Ventura, B. V. & Santhiago, M. R. Femtosecond Laser-assisted Cataract Surgery in Patients With Marfan Syndrome and Subluxated Lens. J. Refract. Surg. Thorofare NJ 1995 31, 338–341 (2015).
- ↑ Blecher, M. H. & Kirk, M. R. Surgical strategies for the management of zonular compromise. Curr. Opin. Ophthalmol. 19, 31–35 (2008).