Transposition Surgeries in Strabismus
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Introduction
Transposition surgeries involve the redirection of the paths of the extraocular muscles.
The history of transposition surgeries in strabismus dates back to 1908, when Hummelsheim first described the transposition procedure for the correction of esodeviation in sixth nerve palsy. A large number of modifications further took place resulting in a large number of variations in the procedure. These procedures however must be avoided in patients with vascular insufficiency, or when there is stiffness of the antagonist extraocular muscle resulting in restriction.
Indications
- Indications for transposition surgeries include
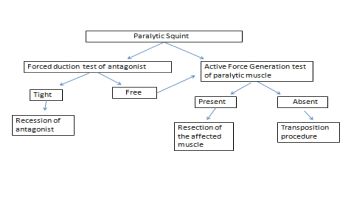
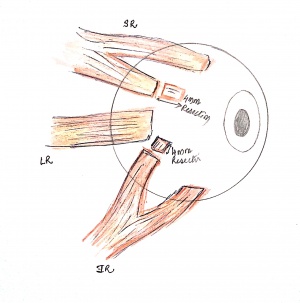
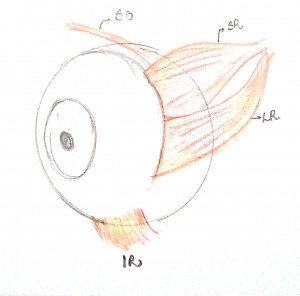
- Paralytic strabismus: The most common indication for transposition surgeries in strabismus is paralytic strabismus. Transposition surgeries must be planned only when the forced duction test is free and active force generation test reveals absence of any active force generation.(Figure1)
- Duane's Retraction Syndrome
- Monocular elevation deficiency
- Lost or slipped muscle
Mechanism of Action
The main aim of transposition surgery is to realign the eyes in primary position.[1] Although the results of a transposition procedure are usually good, patients must understand that the ductions in the direction of action of a paralyzed muscle might not improve much. The mechanism of action of transposition procedures is still controversial. Some authors believe that improvement of alignment in the primary position can be due to a transfer of function of the transposed muscle in the direction of action of the paralyzed muscle, through a change in the direction of vector forces of the transposed muscle. Other hypothesis attributes it to the passive restraint created by the transposed muscle which assists in holding the eye in primary position. In augmented procedures with posterior fixation sutures, it has been suggested that rectus muscle pulleys are diverted posteriorly in the direction of transposition while translating the centre of the globe. Probably more than one mechanism acts together to achieve alignment in the primary position.
Transposition procedures for Sixth nerve palsy
Full tendon transposition
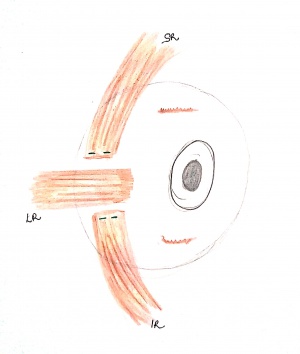
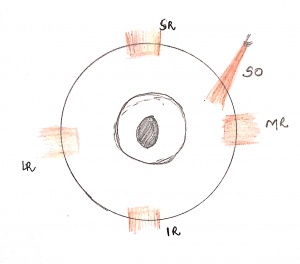
A full tendon transposition involves the dis-insertion of the full-width tendons of the vertical rectus muscles and transposition of these towards the lateral rectus. [2] To prevent the risk of anterior segment ischemia, simultaneous surgery on the horizontal rectus muscles should be avoided. Additionally, it is recommended that the vertical recti are carefully dissected to conserve the anterior ciliary artery branches. Extensive dissection should be avoided. (Figure 2a)
The effect of the transposition can be enhanced through the resection of the vertical rectus muscle before the transposition. Adjustable suture techniques can be used to reduce induced vertical deviations and overcorrections. [3]
Another augmentation technique involves the use of posterior fixation sutures. These sutures are placed at the superior and inferior borders of the horizontal rectus muscle 6-8 mm posterior to its insertion and incorporating 1/4 of the transposed vertical rectus muscle. [4] This modification is believed to increase the vectorial force of the transposition.
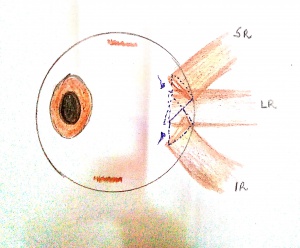
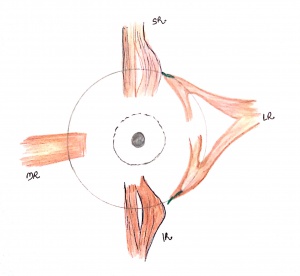
Crossed-adjustable technique
The transposed vertical rectus muscles are passed beneath the lateral rectus muscle and attached at the respective opposite corners of the lateral rectus muscle insertion. This technique increases the transposed muscle path length while avoiding resection of the transposed muscles. In the original description for abducens nerve palsy, it reduced the need for simultaneous ipsilateral medial rectus weakening more than twofold.[5](Figure 2b)
Hummelsheim procedure (partial tendon transposition)
A partial tendon transposition involves the transposition of 1/2 tendon-width of the vertical rectus muscles, reducing the risk of anterior segment ischemia by allowing half of the vertical rectus insertion and its ciliary vasculature to remain intact.
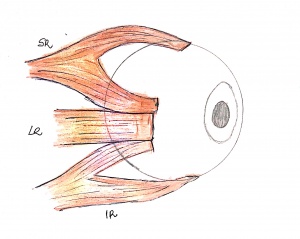
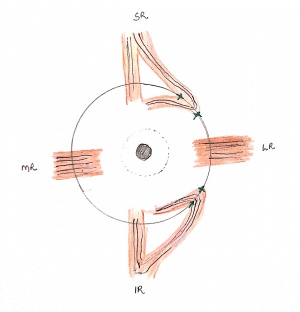
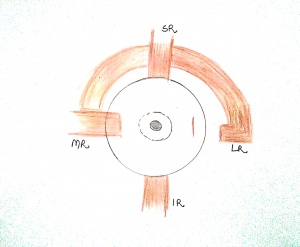
Technique
After making a limbal based incision superiorly and inferiorly, the superior and inferior muscles are split half-tendon width up to approximately 14 mm from the insertion with the help of a muscle hook. The temporal halves of the superior and inferior rectus muscles are then secured, disinserted and further transposed towards the lateral rectus. The transposed halves of both vertical recti are then sutured to the sclera adjacent to the insertion of the lateral rectus. While splitting and dis-inserting the vertical recti, care must be taken to protect the anterior ciliary circulation.[6] (Figure 3)
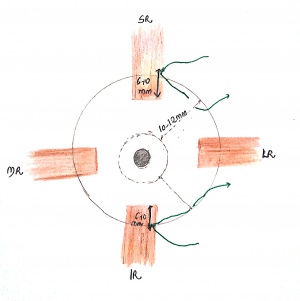
Modified Hummelsheim
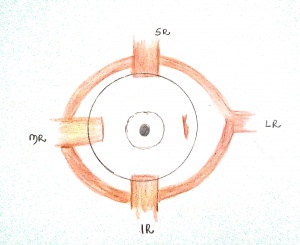
To increase the effectiveness of the Hummelscheim procedure, a simultaneous recession of the medial rectus muscle and/or resection of the transposed tendons or posterior fixation sutures can be added. (Figure 4). The modified Hummelsheim procedure has been reported to correct a preoperative deviation of 43 Δ ± 5 Δ to postoperative 6 Δ ± 7 Δ .[7]
Jensen’s procedure
Jensen’s procedure was first described by Jensen et al in 1964.[8] In this procedure the muscle bellies of adjacent muscles are tied together without being dis-inserted, therefore decreasing the risk of anterior segment ischemia. Even with this procedure, however, some vascular compromise occurs, and cases of anterior ischemia have been reported.
Technique
When performing Jensen’s procedure for lateral rectus palsy, limbal base incisions are made to expose the bellies of the lateral, superior and inferior rectus. The intermuscular septa of all the three muscles is then dissected to expose 12-15 mm of the muscle belly behind its insertion. The muscle bellies of each of the exposed recti are then split half tendon width to at least 12-14 mm from the insertion with the help of a muscle hook. During this step, utmost care must be taken to preserve at least one anterior ciliary artery undisturbed. A 5-0 ethibond or Mersilene suture is then used to form a loop around each of the adjacent muscle belly halves (superior-lateral rectus and inferior-lateral rectus). The sutures are then tied to approximate the muscle bellies approximately 12 mm behind the insertion. (Figure 5)
Effectiveness of Jensen Procedure
Cline et al in their study on 26 patients who underwent Jansen’s procedure with medial rectus recession found that at 6 months follow up 18 eyes had less than 20% of normal abduction saccadic velocity; 9 eyes had 20% to 40%, and 2 patients could not be assessed with saccadic velocities.[9]
Modifications of Jensen's Procedure
Vessel sparing modification: In this modification instead of looping the suture around the entire rectus muscle segments, the suture can be passed beneath the anterior ciliary vessels present on the orbital surface of each muscle.
Nishida’s Procedure
Technique
The technique was described by Nishida et al in 2003.[10] In this technique after making a limbal based conjunctival peritomy the vertical recti are hooked. Intermuscular septum and fascia along the lateral margin of each of the vertical recti are carefully dissected and the vertical muscle belly is then longitudinally split half tendon width to approximately 15 mm from the insertion with a short muscle hook. Following this, 6-0 nylon sutures are used to secure the temporal half of each muscle 8 to 10mm posterior to the insertion. The same sutures are then passed through the sclera 8mm posterior to the insertion of lateral rectus beside the superior or inferior margin. The temporal margin of each vertical rectus is then transposed and anchored onto the sclera. One scleral suture can be added on the inside edge of each transposed muscle to the sclera.(Figure 6) With this procedure, the risk of anterior segment ischemia is reduced by avoiding muscle tenotomy.
Effectiveness of Nishida's procedure
According to Nishida et al, the surgery resulted in an average correction of 42.4 PD.[10]
Modification Of Nishida's Procedure
Nishida et al further modified the procedure and omitted the step of muscle splitting to prevent further damage during the surgical manipulation (transposition procedure without tenotomy or splitting). [11]
Indications
Besides abducens nerve palsy, the modified Nishida’s technique has been used in patients of monocular elevation deficit[12] and in cases of transected and lost medial rectus[13] [14]
Technique
A limbal based incision is made which helps for better exposure of the vertical recti. Non-absorbable sutures (6-0 polypropylene or ethibond sutures) are passed incorporating the temporal 1/3 of the vertical recti at a distance of 8 to 10 mm behind the insertion points of the vertical recti. The sutures can be tied there to avoid muscle breakage due to tension during transposition. The same suture is then passed through each scleral wall at a distance of 10 to 12 mm behind the supero-temporal and infero-temporal limbus. The temporal margin of each vertical rectus is then transposed and anchored onto the sclera. (Figure7)
Effectiveness of Modified Nishida's procedure
The muscle transposition alone corrects ocular deviations ranging from 24-36 PD. When used in combination with a recession of the medial rectus muscle the correction ranges from 50 to 62 PD. [15]
Superior Rectus transposition (SRT)
SRT was described by Jhonston et al.[16] The procedure involves transposing only the superior rectus muscle to the insertion of lateral rectus. This helps to preserve ciliary circulation and simplifies the procedure. The procedure has been found to improve the mean angle of esotropia, abduction limitation, and head turn, with recovery of stereopsis in 80% of patients with no clinically significant induced vertical or torsional diplopia.[17] Although theoretical concerns with the procedure include vertical misalignment and induced torsion, in practice these complications are infrequent.[18](Figure 8)
To increase the effectiveness of the procedure, the SRT can be combined with augmentation sutures and/or medial rectus recession. An adjustable graded augmentation has also been described.[19]
Inferior Rectus Transposition (IRT)
IRT is a logical alternative to SRT. When combined with an augmentation suture, either with or without simultaneous adjustable medial rectus recession, IRT was shown to significantly improve the esotropia, abduction, and head turn in a small group of patients who were deemed at risk of hypothetical exacerbation by SRT due to preoperative hypertropia or intorsion of the operative eye. IRT can also achieve a small downward shift in the operative eye that can help correct a preexisting hypertropia.[20]
Transposition Procedures for Third Nerve Palsy
Superior oblique tendon transfer
Technique
The procedure was initially described by Peter in 1934.[21] A limbal based peritomy is performed in the supero-nasal quadrant which is sufficient to provide exposure to both medial and superior recti. The superior oblique is isolated and dissected free of surrounding fascial attachments along the tendon, following underneath and along the nasal side of the superior rectus. The superior oblique tendon is engaged on a small muscle hook on the nasal side of the superior rectus muscle and is secured with a double-armed 6-0 absorbable suture The tendon is disinserted and brought down toward the superior edge of the medial rectus insertion. The tendon is then sutured to the sclera at the superior border of the medial rectus insertion. (Figure 9) An adjustable suture technique can be used allowing for immediate management of postoperative vertical deviations. This procedure is generally combined with a profound weakening of the ipsilateral lateral rectus muscle.
Lateral rectus to Medial Rectus transposition
Technique
A limbal based peritomy is performed over the lateral, superior, and medial rectus muscles. The attachments and intermuscular septa of lateral rectus muscle are dissected. The lateral rectus muscle is then secured with 6.0 vicryl sutures and disinserted. This suture is then passed beneath the superior rectus muscle in the direction of the medial rectus muscle, thus pulling the lateral rectus muscle in that direction. The lateral rectus is then sutured near the superior margin of the medial rectus insertion. (Figure 10)
Effectiveness
The procedure was initially described by Taylor[22] and was found to be effective, later Morad et al described the procedure in a case of combined third and fourth nerve palsy.[23]
Full tendon medial transposition of lateral rectus with augmentation sutures
Saxena R et al introduced a modification of the full lateral rectus transposition, for cases with hypertropia along with exotropia. In this modification, the disinserted lateral rectus is passed under the inferior rectus and inferior oblique. It is then reattached just below the insertion of the medial rectus muscle. Augmentation sutures with 5–0 Ethibond are then placed 8 mm behind the new insertion of the transposed lateral rectus muscle, including at least a third of the muscle fibers in each bite. In their series of patients with hypotropia, the lateral rectus muscle was passed under the superior rectus and superior oblique and reattached at the upper border of the medial rectus along with augmentation sutures.[24]
Medial transposition with Y splitting of lateral rectus
Technique
A limbal based peritomy is performed and the lateral rectus is hooked and the intermuscular septa is dissected up to 15mm posterior to the insertion. the lateral rectus muscle is then split half tendon width to approximately 15 mm posterior to the insertion. The split portions of the lateral rectus are then secured with a 6-0 polyester suture, and disinserted. The upper half of the muscle is then passed beneath the superior rectus muscle and superior oblique, and inferior half is moved beneath the inferior rectus muscle and inferior oblique. The two halves of lateral rectus are then inserted near the insertion of medial rectus. (Figure11)
Effectiveness of the procedure
Gokyigit et al, inserted the lateral rectus 1 mm posterior to medial rectus found a success rate of 90 percent with the procedure with the mean pre-op deviation being 73.7Δ ± 8.9Δ and post-op deviation being 11.8Δ ± 1.0Δ.[25]
Augmentation of the split lateral rectus
Indications
The procedure has been used in third nerve palsy and synergistic divergence.[26]
Technique
The surgery is undertaken through four fornix conjunctival incisions in each quadrant after performing a forced duction test to confirm a free lateral rectus muscle. The lateral rectus is hooked, split in half up to at least 15 mm posteriorly after placing 6-0 Vicryl sutures. Superior oblique is hooked and posterior tenectomy is done as in conventional surgeries. Posterior tenectomy of superior oblique helps in free movements of the transposed muscle under it, reduces the abduction effect and hence brings out greater correction. The upper half of the muscle is then passed beneath the superior rectus muscle, and inferior half is moved beneath the inferior rectus muscle and inferior oblique. The two halves of lateral rectus are then inserted near the insertion of medial rectus. In this modification, in addition to the above surgical steps, equatorial fixation sutures are placed 8 mm behind the new insertion of the split muscles with 5-0 Ethibond sutures, incorporating 25℅ of the muscle.[27]
Transposition Procedures for Duane's Retraction Syndrome
Indications of surgery for Duane's Retraction Syndrome
- Presence of a compensatory head posture towards the affected side causing neck discomfort
- Cosmesis in primary gaze due to the horizontal deviation
- Severe co-contraction
Transposition procedures help improve abduction in cases of Duane's retraction syndrome, although there has always been a concern about the increase in severity of co-contraction after transposition surgery.[28]
Various transposition procedures advocated for Duane's Retraction Syndrome include:[29]
- Full Vertical Rectus transposition
- Full Vertical Rectus transposition with cross suture approach
- Jensen's procedure
- Nishida's procedure
- Superior Rectus Transposition
- Inferior Rectus Transposition
Vertical Muscle Palsy
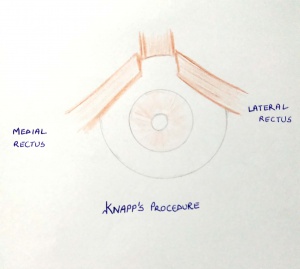
Knapp’s procedure
Knapp’s procedure is indicated in patients of monocular elevation deficiency. In this procedure the horizontal recti (both medial and lateral recti) are disinserted full width and transposed superiorly.[30](Figure 12)
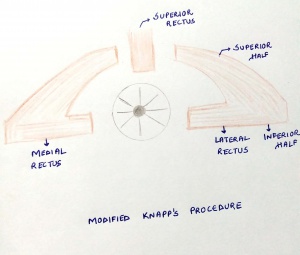
Modified Knapp’s
In modified Knapp’s procedure, both the horizontal recti are split into two halves. The lower half is used for correction of horizontal deviation and the superior half is transposed superiorly.[31](Figure 13)
Augmented Knapp’s
The augmented Knapp’s procedure is similar to Knapp’s with the addition of a posterior fixation or foster suture[32]
Inverse Knapp’s
The procedure is relatively less commonly performed, the common indications include double depressor palsy and congenital absence of inferior rectus. In this procedure, the horizontal recti are transposed to the level of inferior rectus. [33] (Figure10) Maurino et al in their study found Inverse Knapp's to correct the vertical deviation in primary position and down gaze from 16.06 PD to 7.35 PD and 26.45 PD to 6.66 PD respectively.[34]
Single horizontal muscle transposition
Gandhi described a single horizontal muscle (medial or lateral) transposition to 2 mm from the insertion of the superior rectus muscle along the spiral of Tillaux with an augmentation suture placed 8 mm behind its insertion. This procedure allows for the simultaneous inferior rectus recession.[35]
Complications
- Anterior segment ischemia: Circulation to the anterior segment is provided by seven anterior ciliary arteries and two posterior ciliary arteries. One anterior ciliary artery supplies the lateral rectus muscle and two supply each of the other extraocular muscles. The vertical rectus muscle in particular has a major impact on anterior segment circulation. Disinsertion of the recti leads to disruption of blood supply to the anterior segment increasing the risk of anterior segment ischemia (ASI). Old age, atherosclerotic changes in the blood vessels, hyperviscosity, buckle surgery for retinal detachment and simultaneous disinsertion of two or more recti increase the risk of anterior segment ischemia. ASI is associated with lid edema, conjunctival congestion and chemosis, cataractous changes in the lens, corneal edema, anterior chamber cells and flare. Vertical transposition surgeries along with recession of a horizontal muscle carry the highest risk for ASI. Jensen's procedure, although theoretically safer, can also cause ASI. [36]The risk of ASI is maximum in the first six months, hence a repeat surgery should be planned after 6 months of the initial surgery, providing sufficient time for the development of collateral vessels.
- Undercorrection: Undercorrection in strabismus surgeries is far more common than overcorrection. The second surgery to be done depends upon the cause of residual deviation. If the forced duction test (FDT) is still tight then further recession of the antagonist can be planned, but if FDT is free then further addition of foster sutures can be helpful. In third nerve palsy medial periosteal fixation of globe can be planned.
- Induced Vertical deviation: Induced vertical deviations have been observed in 6-30% patients undergoing vertical rectus transposition for lateral rectus palsy.[37] Vertical deviations can be minimized by meticulous surgical dissection of the attachments between inferior rectus muscle, capsulopalpebral fascia, and Lockwood’s ligament. Induced vertical or cyclotropias from altered tension or direction of action of the superior oblique muscle can also occur; thus dissection of the attachments between the superior rectus muscle and the superior oblique tendon are also important. Intraoperative forced ductions can help identify patients at risk for a new-onset hypotropia
- Other complications of squint surgery include tenon's prolapse, conjunctival prolapse, conjunctival cyst, corneal dellen formation, scleral perforation, slipped muscle, bradycardia and secondary infections.
References
- ↑ Rosenbaum AL. The efficacy of rectus muscle transposition surgery in esotropic Duane syndrome and VI nerve palsy;Costenbader Lecture.J AAPOS. 2004 Oct; 8(5):409-19.
- ↑ Schillinger RJ. A new type of tendon transplant operation for abducens paralysis. J Int Coll Surg. 1959;31:593–600.
- ↑ Hendler K, Pineles SL, Demer JL, Yang D, Velez FG. Adjustable augmented rectus muscle transposition surgery with or without ciliary vessel sparing for abduction deficiencies. Strabismus. 2014;22(2):74-80. doi:10.3109/09273972.2014.904901
- ↑ Foster RS. Vertical muscle transposition augmented with lateral fixtation. JAAPOS 1997; 1:20-30
- ↑ Phamonvaechavan P, Anwar D, Guyton DL. Adjustable suture technique for enhanced transposition surgery for extraocular muscles. J AAPOS 2010;14:399-405.)
- ↑ Hummelsheim E. Weitere Ertahunger mit partiellar Sehnenuberpflanzung an der Augenmuskln (abstract) Arch Augenheilkd. 1908–1909;62:71.
- ↑ Couser NL, Lenhart PD, Hutchinson AK. Augmented Hummelsheim procedure to treat complete abducens nerve palsy. J AAPOS. 2012;16(4):331‐335.
- ↑ Jensen CD. Rectus muscle union: A new operation for paralysis of the rectus muscles. Trans Pac Coast Otoophthalmol Soc Annu Meet. 1964;45:359–87.
- ↑ Cline RA, Scott WE. Long-term follow-up of Jensen procedures.J Pediatr Ophthalmol Strabismus. 1988 Nov-Dec;25(6):264-9.doi: 10.3928/0191-3913-19881101-04.
- ↑ 10.0 10.1 Nishida Y, Inatomi A, Aoki Y, et al. A muscle transposition procedure for abducens palsy, in which the halves of the vertical rectus muscle bellies are sutured onto the sclera. Jpn J Ophthalmol 2003;47:281–286.
- ↑ Nishida Y, Hayashi O, Oda S, Kakinoki M, Miyake T, Inoki Y, et al. A simple muscle transposition procedure for abducens palsy without tenotomy or splitting muscles. Jpn J Ophthalmol 2005;49:179-80.
- ↑ Murthy SR, Pappuru M. Modified Nishida's procedure for monocular elevation deficiency. J AAPOS. 2018;22(4):327‐329.e1.
- ↑ Kong M, Zhang LJ, Dai S, Li JH. A new application of modified Nishida muscle transposition procedure for medial rectus muscle transection following endoscopic sinus surgery without tenotomy or splitting muscles. J AAPOS. 2019;23(5):287‐289.
- ↑ Sharma P, Gaur N, Phuljhele S, Saxena R. What's new for us in strabismus?. Indian J Ophthalmol. 2017;65(3):184‐190. doi:10.4103/ijo.IJO_867_16
- ↑ Muraki S, Nishida Y, Ohiji M. Surgical results of a muscle transposition procedure for abducens palsy without tenotomy and muscle splitting. Am J Ophthalmol. 2013 Oct;156(4):819-24
- ↑ Johnston SC, et al. ARVO abstract; IOVS 2006;47:ARVO E-Abstract 2475.
- ↑ Mehendale RA, Dagi LR,Wu C, Ledoux D, Johnston S, Hunter DG.Superior rectus transposition and medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol 2012;130:195-201.
- ↑ Velez FG, Oltra E, Isenberg SJ, Pineles SL. Assessment of torsion after superior rectus transposition with or without medial rectus recession for Duane syndrome and abducens nerve palsy. J AAPOS 2014; 18:457-60.
- ↑ Dagi LR, Elhusseiny AM. Adjustable graded augmentation of superior rectus transposition for treatment of abducens nerve palsy and Duane Syndrome. J AAPOS. 2020 Oct;24(5):268.e1-268.e7.
- ↑ Velez FG, Chang M, Pineles SL. Inferior rectus transposition: a novelprocedure for abducens palsy. Am J Ophthalmol 2017;177:126-30.
- ↑ Peter LC. The use of the superior oblique as an internal rotator in third nerve paralysis. Trans Am Ophthalmol Soc 1933; 31:232-7.
- ↑ Taylor JN. Surgical management of oculomotor nerve palsy with lateral rectus transplantation to the medial side of the globe. Aust N Z J Ophthalmol 1989;17:27-31.
- ↑ Morad Y, Nemet P. Medial transposition of the lateral rectus muscle in combined third and fourth nerve palsy. J AAPOS 2000;4:246-7.
- ↑ Saxena R, Sharma M, Singh D, Sharma P. Full tendon medial transposition of lateral rectus with augmentation sutures in cases of complete third nerve palsy. Br J Ophthalmol. 2018;102(6):715‐717.
- ↑ Gokyigit B, Akar S, Satana B, Demirok A, Yilmaz OF. Medial transposition of a split lateral rectus muscle for complete oculomotor nerve palsy. J AAPOS. 2013;17(4):402‐410.
- ↑ Sharma P, Saxena R, Bhaskaran K, Dhiman R, Sethi A, Obedulla H. Augmented medial transposition of split lateral rectus in the management of synergistic divergence. J AAPOS. 2020;24(1):37‐40.
- ↑ Saxena R, Sharma M, Singh D, Dhiman R, Sharma P. Medial transposition of split lateral rectus augmented with fixation sutures in cases of complete third nerve palsy. Br J Ophthalmol. 2016;100(5):585‐587.
- ↑ Jampolsky A. Duane syndrome. In: Rosenbaum AL, Santiago AP, eds.Clinical Strabismus Management. Philadelphia: W.B. Saunders &Co; 1999:331.
- ↑ Doyle JJ, Hunter DG. Transposition procedures in Duane retraction syndrome. J AAPOS. 2019;23(1):5‐14.
- ↑ Knapp P. The surgical treatment of double elevator paralysis. Trans Am Ophthalmol Soc. 1969; 67:304–2
- ↑ Kamlesh, Dadeya S. Surgical management of unilateral elevator deficiency associated with horizontal deviation using a modified Knapp’s procedure. Ophthalmic Surg Lasers Imaging. 2003; 34:230–5.
- ↑ Snir M, Friling R, Kalish-Stiebel H, Bourla D, Weinberger D, Axer-Siegel R. Combined rectus muscle transposition with posterior fixation sutures for the treatment of double-elevator palsy. Ophthalmology. 2005;112(5):933–938.
- ↑ Burke J. Inverse Knapp procedure. Eye (Lond). 2001;15(Pt 1):5.
- ↑ Maurino V, Kwan AS, Lee JP. Review of the inverse Knapp procedure: indications, effectiveness and results. Eye (Lond). 2001;15(Pt 1):7‐11.
- ↑ Gandhi U, Kekunnaya R. Single Horizontal Muscle (Medial or Lateral Rectus) Transposition and Inferior Rectus Recession in Monocular Elevation Deficit: A Novel Surgical Technique. J Pediatr Ophthalmol Strabismus. 2019;56(3):183-187. doi:10.3928/01913913-20190306-01
- ↑ von Noorden GK. Anterior segment ischemia following the Jensen procedure. Arch Ophthalmol. 1976;94(5):845‐847.
- ↑ Ruth AL, Velez FG, Rosenbaum AL. Management of vertical deviations after vertical rectus transposition surgery. J AAPOS. 2009;13(1):16-1919117778