Morning Glory Anomaly
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Morning Glory Disc Anomaly
Disease
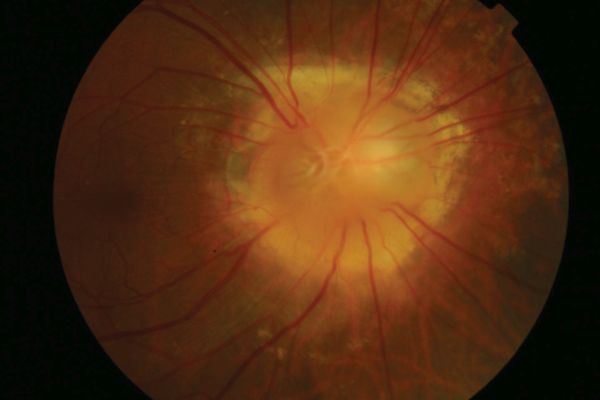
Morning glory anomaly is a rare congenital malformation of the optic nerve.[2] It is named for its resemblance to the morning glory flower.[3] When it is associated with systemic signs and symptoms, it is known as morning glory syndrome.
Etiology
The embryonic origins of morning glory anomaly is not clear but is hypothesized to be either due to a defect in fetal fissure closure or a primary mesenchymal abnormality.[2]
Risk Factors
Morning glory anomaly is more common in females and more rare in African-Americans.[4]
Systemic Associations
- Transsphenoidal basal encephalocele
- Basal encephalocele, a congenitally malformed outpouching of the meninges, often contains the optic chiasm and hypothalamus and protrudes through a defect in the sphenoid bone.[4]
- Children with this structural defect often have dysmorphic features, including a wide head, flat nose, hypertelorism, and a midline notch in the upper lip.[4]
- Many patients with transsphenoidal encephalocele also have callosal agenesis, leading to dilation of the lateral ventricles.[5]
- Although common presentation of basal encephalocele includes midline defects, some adults can present uncommonly with headaches, visual field defects, or vision loss. [6][7]
- Of note, basal encephalocele is also associated with ocular abnormalities other than MGDA, including other optic disc dysplasia, optic disc pits with maculopathy, chorioretinal atrophy, and colobomas.
- Cerebrovascular anomalies
- Pituitary stalk duplication (PSD)
- There are various theories regarding the mechanism of PSD, some including incomplete splitting of the developing pituitary stalk, prochordal plate cell duplication, or notochord tissue splitting.[8] Although PSD is uncommon, it is often reported in patients who present with MGDA and/or moyamoya.[8] [9]
Diagnosis
Symptoms
Visual acuity can vary from normal 20/20 to very poor(20/200 to count fingers) depending on the extent of optic nerve anomaly. Patients often have visual field defects, commonly enlarged blind spots.[3][4] However, amblyopia may be a contributing factor to the poor vision in unilateral cases. Patients are also often initially referred for leukocoria or strabismus.[3]
Clinical Diagnosis
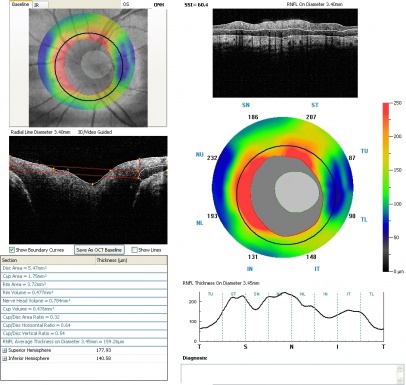
The optic nerve appears large and funneled.[4] There is a conical excavation of the dysplastic optic disc and the surrounding posterior pole, filled with glial tissue.[3] An increased number of straight retinal vessels arise from the disc margin and peripapillary pigmentation can also been seen.[3] The term “macular capture” is used when the macula is involved in the excavation.[4] Contractions of the optic nerve have also been described and is attributed to the presence of myofibroblasts in the papillae.[3] Due to unilateral involvement in most cases, an afferent pupillary defect can be noted.[3]
Differential diagnosis
Optic nerve coloboma: Optic nerve colobomas will typically appear as a white excavation involving the inferior portion and extending to the choroid and retina.[3] Optic nerve colobomas also lack the central glial tuft and peripapillary pigmentation seen in morning glory disc anomalies.[4] It is important to differentiate from a morning glory disc anomaly because optic nerve colobomas can be associated with systemic syndromes such as CHARGE (coloboma of the eye, heart defects, choanal atresia, growth retardation, genitourinary abnormalities and ear abnormalities).[3]
Peripapillary staphyloma: Peripapillary staphyloma is another excavation of the optic disc where the optic disc is seen at the bottom of the excavation.[4] It can be differentiated from morning glory disc anomaly by the lack of central glial tuft and normal retinal vasculature.[4]
Management
There is no treatment for morning glory disc anomaly. However it is important to optimize visual acuity to prevent amblyopia.[3] Dilated fundus exams should be done to detect serous retinal detachments that tend to originate in the peripapillary area and extends to the posterior pole.[4] Brain imaging (MRI, MRA and/or CTA) should be done to rule out CNS involvement, including basal encephalocele, Moyamoya and other structural or vascular abnormalities.[3] Surgical correction of the transsphenoidal basal encephalocele can be extremely difficult or even contraindicated due to the vital structures that may be found in the herniation, including the optic chiasm, the hypothalamus, and the anterior cerebral artery.[4]
References
- ↑ American Academy of Ophthalmology. Morning glory disc anomaly. https://www.aao.org/image/morning-glory-disc-anomaly-2 Accessed June11, 2019.
- ↑ Jump up to: 2.0 2.1 Cennamo, G et al. 2009. Evaluation of Morning Glory Syndrome with Spectral Optical Coherence Tomography and Echography. Ophthalmology. 117:6, p1269–1273
- ↑ Jump up to: 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 Lee, BJ and Traboulsi, EI. 2008. Update on the Morning Glory Disc Anomaly. Ophthalmic Genetics 29:2, p47-52
- ↑ Jump up to: 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 Brodsky, M.C. 2010. Congenital Optic Disc Anomalies in Pediatric Neuro-ophthalmology. 2nd ed. New York: Springer
- ↑ Jump up to: 5.0 5.1 Brodsky, MC. 1994. Congenital Disc Anomalies. Survey of Ophthalmology 39:2, p89-112
- ↑ Monica ML, Connolly ES, Kalil RF. Basal encephalocele presenting with monocular visual loss. J Clin Neuroophthalmol. 1984;4(1):9-13.
- ↑ Moore T, Freedman K. Basal Encephalocele Presenting with Bitemporal Hemianopsia in an Adult Male. Neuroophthalmology. 2017;42(3):156-158. Published 2017 Aug 18. doi:10.1080/01658107.2017.1356857
- ↑ Jump up to: 8.0 8.1 Khodeiry MM, Chau VQ, Yasin A, Starke RM, Miri S, Pasol J. Morning glory disc anomaly associated with moyamoya disease and pituitary stalk duplication. Am J Ophthalmol Case Rep. 2022;27:101632. Published 2022 Jun 24. doi:10.1016/j.ajoc.2022.101632
- ↑ Loddenkemper T, Friedman NR, Ruggieri PM, Marcotty A, Sears J, Traboulsi EI. Pituitary stalk duplication in association with moya moya disease and bilateral morning glory disc anomaly - broadening the clinical spectrum of midline defects. J Neurol. 2008;255(6):885-890. doi:10.1007/s00415-008-0799-5