Intraocular Lens Opacification
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
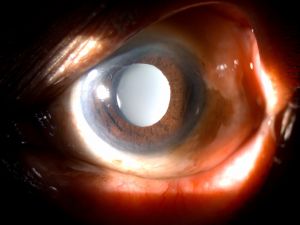
Intraocular lens (IOL ) Opacification is an uncommon but serious complication of cataract surgery. It can cause significant deterioration of visual performance and may necessitate IOL explantation and exchange.[1] Clinical identification and evaluation of this condition is important as a misdiagnosis may prompt surgeons to perform unnecessary interventional procedures such as Nd YAG capsulotomy or vitrectomy resulting in complications.[2] A better understanding of the risk factors can also help in avoidance of opacification.
Disease Entity
Disease
IOL opacification is usually unilateral and may be seen on the surfaces or in the substance of the optic, haptics, or whole lens.[3] Different patterns of opacification are observed in different IOL biomaterials such as Snowflake opacification in Polymethylmethacrylate (PMMA) IOLs, Discoloration in Silicone IOLs, Calcification in Hydrophilic acrylic IOLs and IOL Glistenings in Hydrophobic acrylic IOLs.[1][4]
Time of presentation
Intraoperative
Early postoperative (hours or days after surgery)
Late postoperative (several months or years after surgery).
Risk Factors[5] [6] [7] [8] [9] [10]
| Local ocular factors: | Systemic associations | IOL Related Factors: |
|---|---|---|
| Breakdown of Blood Aqueous Barrier (BAB):
Prolonged or complex surgery, Severe post-operative inflammation Chronic uveitis Preservatives in topical glaucoma medications
Residual lens matter-dystrophic calcification due to increase in calcium concentration of aqueous humor
Ocular Pathologies: Glaucoma Pseudoexfoliation- spoke like opacification on anterior IOL surface
Secondary Surgical Interventions: Posterior Lamellar Keratoplasty procedures (DSEK, DSAEK, DMEK) with intra cameral injection of gas or air There is a recent increase in the incidence PPV (pars plana vitrectomy) with endotamponade Intracameral rtPA (recombinant tissue plasminogen activator) Vitreoretinal surgeries- adherence of silicone oil to the IOL optic more commonly seen in silicone IOLs Nd:YAG Capsulotomy -direct contact between lens and vitreous following Nd:YAG capsulotomy |
Diabetes Mellitus due to breakdown of BAB
Systemic medications -Long term use of Amiodarone and Rifabutin are associated with Silicone IOL Opacification/Discoloration. Hypertension |
IOL biomaterial impurities
Errors in IOL manufacturing and storage
Interactions with the packaging material-silicone sleeves which are used to hold IOL in the vial impart negative charge to IOL resulting in its opacification. Higher refractive power of the IOL and the use of bigger diameter cartridge during phacoemulsification were significantly related to the higher severity of glistening. |
Etiology and Patho physiology
Based on many reports, it has been noted that opacification can occur in different ways depending on the time period and the IOL materials.
Intra Operative opacification
Usually caused by precipitation of crystalline deposits on the IOL's surface, which can be related to the viscoelastic substance or the balanced saline solution[11] [12] used in the procedure. There are recent reports of acute intra operative clouding of hydrophilic and hydrophobic IOLs which could be caused by sudden changes in temperature.[13] The acute clouding was transient and resolved in a few hours after the procedure.
Opacification in Immediate postoperative period
There are reports of silicone IOL opacification due to hydration (brown haze) and also due to the interaction of hydrogel material with dyes or the viscoelastic used during surgery[14]
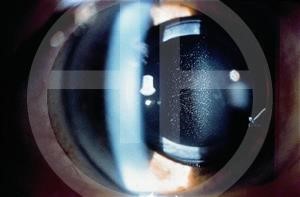
Glistenings
Glistenings are fluid-filled microvacuoles (1- 20 µm) that form within the intraocular lens (IOL) optic when the IOL is in an aqueous environment. It is more commonly seen in hydrophobic IOLs and forms as a result of thermal changes rather than structural changes.[4][15] Glistenings are thought to cause retinal stray light and light scatter and to consequently negatively affect the quality of vision. The only option for a patient with symptomatic glistening is IOL exchange. However, most patients with IOL glistening do not have visual complaints.
Calcification
Calcification is due to precipitation of calcium and phosphate on and/or within the IOL and is more frequently seen with hydrophilic IOLs.
Neuhann et al. suggested three main groups of calcifications[16]:
- primary—related to IOL itself (properties of the polymer, it’s surface or IOL packaging),
- the secondary calcification can occur as a result of diseases or pathologies that causes the disruption of BAB and
- pseudocalcification when false positive staining of calcium occurs. However, usually, calcification is a multifactorial problem.
Werner et al. proposed possible causes of calcification after surgeries that require exogenous gas or other substances injection into the eye.[17] In these cases, calcification is confined to the central area of optic. Injected gas, air, tissue plasminogen activator, silicone oil can have direct contact to IOL surface. Secondly, it can be related to a metabolic change in the anterior chamber due to the presence of the exogenous substance and lastly—exacerbated inflammatory reaction with the breakdown of BAB caused by the surgical procedure itself.
Calcification in silicone IOLs is associated with the coexistence of asteroid hyalosis, as more than 85% of patients with calcification had clinically detectable ipsilateral asteroid hyalosis.
Snowflake Degeneration
Snowflake degeneration is a slowly progressive opacification of PMMA IOLs due to prolonged exposure to ultraviolet radiation. It affects the central region of IOL and leaves the periphery relatively free of the deposits due to its protection by the iris.[18] [19]
Diagnosis
History
History of cataract extraction with IOL implantation.
Symptoms
Opacifications of the IOL optic may cause reduced visual acuity, decreased contrast sensitivity and glare. Glistenings specifically do not appear to cause a significant decrease in visual acuity but could degrade vision by inducing glare symptoms.
Clinical Diagnosis
The key to diagnosis is careful slit lamp examination in high magnification paying special attention to the IOL optic surfaces for signs of granularity or opacification. Slit lamp photography helps to monitor progression. Visual acuity and contrast sensitivity are reduced in IOL opacification cases.
Diagnostic procedures
AS-OCT (Anterior Segment Optical Tomography) helps in detection of presence, location and density of calcification.[20] [21] Very superficial changes are more difficult to detect in this way.
Differential diagnosis
- Posterior capsular opacification
- Vitreous haze or hemorrhage[22]
- Anterior lens epithelial cell proliferation
- Inter lenticular Opacification in piggy back IOL
- IOL Schisis[23]
Management
Surgery
IOL exchange is the only therapeutic option in symptomatic patients with opacified IOL.
Video credit- Uday Devgan MD - CataractCoach.com[24]
Complications
IOL Exchange can be associated with zonular dehiscence (ZD), posterior capsular rupture (PCR) or corneal decompensation.[25] The adherence of most deposits is extremely strong and Nd:YAG laser treatment is often proven to be ineffective in the cleaning of the lenses' surfaces and unnecessary laser capsulotomy in eyes with opacified IOLs may also increase the complication rate during the IOL exchange procedure.[26] It was reported that 33% of IOL exchanges require an anterior vitrectomy, this can increase to 48% with a previously performed Nd:YAG capsulotomy[27] and even jeopardize ‘in the bag’ implantation of IOL.[2] Cases of postoperative recurrent cystoid macular edema, retinal detachment and choroidal hemorrage following IOL exchange have been reported in patients with IOL opacification, misdiagnosed as PCO and treated initially with Nd:YAG Capsulotomy. Erroneous diagnosis as vitreous hemorrage or haze can lead to unnecessary vitrectomy. In such a case, IOL exchange complicated by post operative endophthalmitis has been reported.
References
- ↑ Jump up to: 1.0 1.1 Szigiato A-A, Schlenker MB, Ahmed IIK. Populationb ased analysis of intraocular lens exchange and repositioning. J CataractRefract Surg. 2017;43(6):754-760.
- ↑ Jump up to: 2.0 2.1 Werner L. Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg. 2007 Apr;33(4):713-26. doi: 10.1016/j.jcrs.2007.01.015. PMID: 17397749.
- ↑ Neuhann IM, Werner L, Izak AM, Pandey SK, Kleinmann G, Mamalis N, et al. Late postoperative opacification of a hydrophilic acrylic (hydrogel) intraocular lens: A clinicopathological analysis of 106 explants. Ophthalmology 2004;111:2094-101.
- ↑ Jump up to: 4.0 4.1 Werner L. Glistenings and surface light scattering in intraocular lenses.J Cataract Refract Surg2010;36:1398-420.
- ↑ Rahimi M, Azimi A, Hosseinzadeh M. Intraocular Lens Calcification: Clinico-pathological Report of Two Cases and Literature Review. J Ophthalmic Vis Res. 2018 Apr-Jun;13(2):195-199. doi: 10.4103/jovr.jovr_36_16. PMID: 29719650; PMCID: PMC5905315.
- ↑ Grzybowski A, Markeviciute A, Zemaitiene R. A narrative review of intraocular lens opacifications: update 2020. Ann Transl Med 2020;8:1547.
- ↑ Kubaloglu A, Sari ES, Koytak A, Cinar Y, Erol K, Ozerturk Y. Intraocular lens exchange through a 3.2-mm corneal incision for opacified intraocular lenses. Indian J Ophthalmol. 2011 Jan-Feb;59(1):17-21. doi: 10.4103/0301-4738.73713. PMID: 21157067; PMCID: PMC3032237.
- ↑ Ma ST, Yang CM, Hou YC. Postoperative intraocular lens opacification. Taiwan J Ophthalmol. 2018 Jan-Mar;8(1):49-51. doi: 10.4103/tjo.tjo_78_17. PMID: 29675350; PMCID: PMC5890585.
- ↑ Goodall KL, Ghosh YK. Total opacification of intraocular lens implant after uncomplicated cataract surgery: A case series. Arch Ophthalmol 2004;122:782-4.
- ↑ Apple DJ, Werner L. Complications of cataract and refractive surgery: A clinicopathological documentation. Trans Am Ophthalmol Soc 2001;99:95-107.
- ↑ Jensen MK, Crandall AS, Mamalis N, Olson RJ. Crystallization on intraocular lens surfaces associated with the use of HealonGV. Arch Ophthalmol 1994; 112:1037–1042
- ↑ Hickman MS, Werner L, Mamalis N, et al. Intraoperative explantation of two single-piece hydrophobic acrylic intraocular lenses due to surface deposits. Eye 2006; 20:1054–1060
- ↑ Tyagi, P., Shah, N. & Jabir, M. Intraoperative clouding of a posterior chamber intraocular lens. Int Ophthalmol 31, 483–484 (2011). https://doi.org/10.1007/s10792-011-9481-5
- ↑ Werner L, Dornelles F, Hilgert CR, et al. Early opacification of silicone intraocular lenses: laboratory analyses of 6 explants.J Cataract Refract Surg 2006; 32:499–509
- ↑ Mamalis N. Intraocular lens glistenings. J Cataract Refract Surg. 2012 Jul;38(7):1119-20. doi: 10.1016/j.jcrs.2012.05.023. PMID: 22727278.
- ↑ Neuhann IM, Kleinmann G, Apple DJ. A new classification of calcification of intraocular lenses. Ophthalmology2008;115(1):73–79.
- ↑ Werner L, Wilbanks G, Nieuwendaal CP, et al. Localized opacification of hydrophilic acrylic intraocular lenses after procedures using intracameral injection of air or gas. J Cataract Refract Surg 2015;41:199-207.
- ↑ Apple DJ, Peng Q, Arthur SN, et al. Snowflake degeneration of polymethyl methacrylate posterior chamber intraocular lens optic material; a newly described clinical condition caused by unexpected late opacification of polymethyl methacrylate. Ophthalmology 2002; 109:1666–1675
- ↑ Dahle N, Werner L, Fry L, Mamalis N. Localized, central optic snowflake degeneration of a polymethyl methacrylate intraocular lens: clinical report with pathological correlation. Arch Ophthalmol 2006; 124:1350–1353
- ↑ Werner L, Michelson J, Ollerton A, Leishman L, Bodnar Z. Anterior segment optical coherence tomography in the assessment of postoperative intraocular lens optic changes. J Cataract Refract Surg. 2012 Jun;38(6):1077-85. doi: 10.1016/j.jcrs.2012.01.027. PMID: 22624909.
- ↑ Choudhry S, Goel N, Mehta A, Mahajan N. Anterior segment optical coherence tomography of intraocular lens opacification. Indian J Ophthalmol. 2018;66(6):858-860. doi:10.4103/ijo.IJO_1172_17
- ↑ Haymore J, Zaidman G, Werner L, Mamalis N, Hamilton S, Cook J, Gillette T. Misdiagnosis of hydrophilic acrylic intraocular lens optic opacification: report of 8 cases with the MemoryLens. Ophthalmology. 2007;114(9):1689-95.
- ↑ Neuhann IM, Neuhann TF, Kleinmann G, Apple DJ. Clinical presentation of intraocular lens schisis. J Cataract Refract Surg. 2006 Sep;32(9):1503-8. doi: 10.1016/j.jcrs.2006.04.016. PMID: 16931263.
- ↑ Devgan, U. YouTube. CataractCoach 1011: IOL exchange of an opaque IOL. https://youtu.be/MlPmywHWiPA Accessed February 14, 2023.
- ↑ Dagres E, Khan MA, Kyle GM, et al. Perioperative complications of intraocular lens exchange in patients with opacified Aqua-Sense lenses. J Cataract Refract Surg 2004;30:2569-73.
- ↑ Tandogan T, Khoramnia R, Choi CY, et al. Optical and material analysis of opacified hydrophilic intraocular lenses after explantation: a laboratory study. BMC Ophthalmol 2015;15:170.
- ↑ Platt SM, Iezzi R, Mahr MA, et al. Surgical removal of dystrophic calcification on a silicone intraocular lens in association with asteroid hyalosis. J Cataract Refract Surg 2017;43:1608-10.