Tilted Disc Syndrome
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Tilted Disc Syndrome
Disease
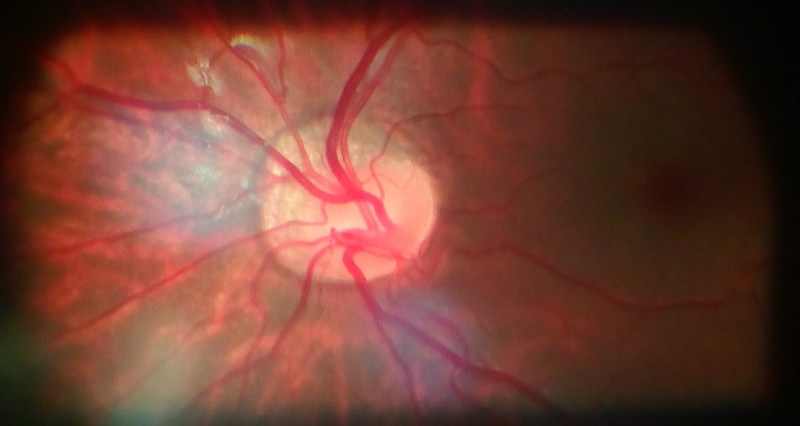
Tilted disc syndrome (TDS), also known as Fuchs Coloboma, is a congenital anomaly that occurs in 1 to 2% of the population. While mostly understood as a nonhereditary process, reports of autosomal dominant inheritance exist. It is characterized by inferonasal tilting of the optic disc and most commonly occurs bilaterally. TDS also has an association with high myopia as one fifth of patients with greater than 5 diopters of myopia have tilted discs. Bitemporal superior visual field defects are present in about one-fifth of patients with tilted discs and other features of TDS include inferior or inferonasal crescent, irregular orientation of retinal vessels (situs inversus), and an ectasia of the lower fundus or inferior staphyloma.
Etiology
TDS is thought to be caused by oblique insertion of the optic nerve and retinal vessels due to incomplete closure of the embryonic fissure of the eye. Additionally, there is hypoplasia and thinning of the retinal, choroidal, and scleral layers with focal hypopigmentation and ectasia of the inferonasal posterior wall of the globe. It is unclear whether both the disc anomalies and inferior staphylomas co-exist at birth or whether the inferior staphyloma deepens with time.
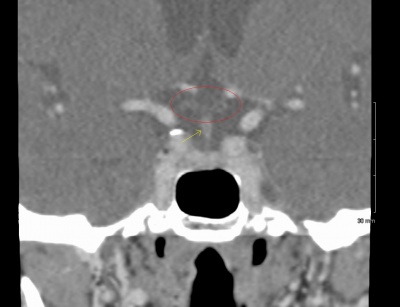
While Fuchs made early descriptions of tilted optic discs, the first clear description of TDS was by Rucker in 1944. To date, TDS has mainly been analyzed by ophthalmoscopic examination; however, OCT, CT, and MRI have also been used to characterize the abnormalities in TDS.
Pathophysiology
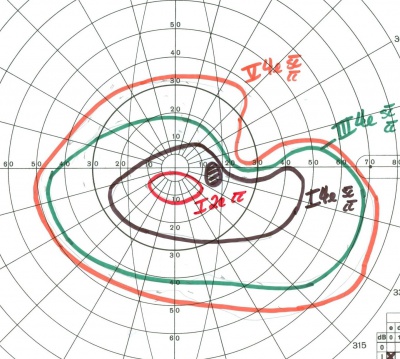
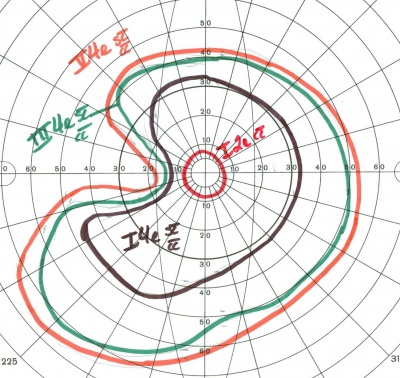
The superior bitemporal visual field defects associated with TDS may be confused with chiasmal lesions; however, the visual field defects in TDS can cross the vertical meridian. Other types of defects in TDS include altitudinal or arcuate defects that may be confused with glaucomatous changes.
The visual field defects may be a result of a refractive scotoma due to regional myopia confined to the ectatic inferior fundus. These defects can often be reduced or eliminated with myopic correction corresponding to the floor of the ectasia; however, if extensive ectasia or coloboma is present, the visual field defect may not improve with optical correction.
Diagnosis
Physical Examination
Myopia, tilted optic disc, situs inversus of retinal vessels (a nasal detour of the temporal retinal vessels as they emerge from the disc before turning back temporally), scleral crescent located inferiorly or inferonasally, inferior staphyloma
Diagnostics
Each patient suspected of TDS should undergo complete ophthalmic examination including refraction and dilated fundus exam. The diagnosis can usually be made based on the fundoscopic appearance of the optic disc; however, OCT, CT, and MRI have been used to show the various abnormalities in the optic nerve and shape of the eye in TDS. As mentioned prior, visual field testing may reveal superior bitemporal visual field defects that do not respect the vertical meridian. Diagnostic challenges may be present if TDS occurs concurrently with true chiasmal or glaucomatous disease.
Complications
There are various macular complications described in TDS in the literature. These include retinal pigment epithelium (RPE) atrophy, choroidal neovascular membrane (CNVM), subretinal fluid (SRF), polypoidal choroidal vasculopathy (PCV), fovea plana, foveoschisis, and lamellar macular hole (LMH). Choroidal mechanical and hemodynamic changes at the upper edge of the staphyloma have been proposed to explain the pathophysiology of these complications.[1][2]
Another significant complication is serous maculopathy associated with tilted disc syndrome.
Serous maculopathy associated with tilted disc syndrome
Clinical Features:
- Presence of tilted disc (superotemporal part of optic disc lying anterior to inferonasal part of disc)
- Presence of posterior staphyloma with RPE atrophy at the edge of staphyloma
Investigations:
- FFA: multiple pinpoint leakages at the site of RPE atrophy
- OCT: Serous macular detachment
Differential Diagnosis: Chronic CSR
Management: Photocoagulation to leakage site
Differential diagnosis
Optic nerve hypoplasia, megalopapilla, peripapillary staphyloma, colobomatous optic disc, optic pit, myelinated nerve fiber layer, glaucoma, chiasmal lesion while traditionally thought of as a benign congenital anomaly, cases of serous retinal detachment have been reported.
Gallery
Case Example
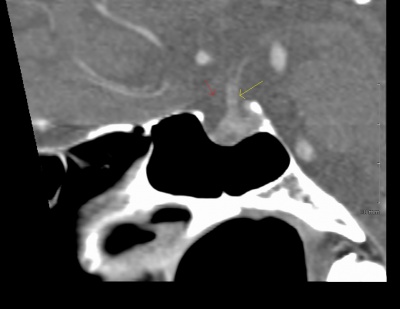
71 year old man with ~10 diopters of myopia OU and tilted optic nerves on clinical exam. Goldmann visual field testing shows bilateral superotemporal defects. CT sella shows no chiasmal lesion.
References
- ↑ Kumar V, Surve A, Kumawat D, Azad S, Vohra R, Venkatesh P. Macular associations of tilted disc syndrome. Indian J Ophthalmol. 2021 Jun;69(6):1451-1456
- ↑ Cohen SY, Vignal-Clermont C, Trinh L, Ohno-Matsui K. Tilted disc syndrome (TDS): New hypotheses for posterior segment complications and their implications in other retinal diseases. Prog Retin Eye Res. 2021 Nov 17:101020
- Williams, A, et al. The tilted disc syndrome. Practical Neurology, 2005, 5, 54-55
- Bottoni FG, et al. Dominant inherited tilted disc syndrome and lacquer cracks. Eye (1990), 4, 504-9
- Manfre L, Vero S, Focarelli-Barone C, Lagall R. Bitemporal Pseudohemianopia related to the “Tilted Disk” Syndrome: CT, MR, and Fundoscopic Findings. AJNR Am J Neuroradiol 20:1750-1751, October 1999
- Vuori ML Mantyjarvi M. Tilted disc syndrome may mimic false visual field deterioration. Acta Ophthalmol. 2008 Sep;86(6):622-5.
- Rucker CW (1944) Bitemporal defects in the visual fields resulting from developmental anomalies of the optic discs. Archives of Ophthalmology, 32, 56-9.
- Apple DJ, et al. Congenital anomalies of the optic disc. Surv Ophthalmol 27: 3-41
- Giuffre G. Hypothesis on the pathogenesis of papillary dysversion syndrome. J Fr Ophtalml 8: 565-572
- Shinohara K, et al. Analyses of shape of eyes and structure of optic nerves in eyes with tilted disc syndrome by swept-source optical coherence tomography and three-dimensional magnetic resonance imaging. Eye (2013) 27, 1233-1242
- Donati MC, et al. Treatment of macular serous neuroretinal detachment in tilted disk syndrome: report of 3 cases. Eur J Ophthalmol 2013 Mar-Apr; 23(2):267-70