Strabismus Surgery, Horizontal
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Strabismus is defined as a misalignment of the eyes. It affects approximately 4% of the population the United States. [1] It is further defined by the direction of misalignment. The types of horizontal misalignment are esotropia (inturn) or exotropia (outturn).
Risk Factors
Risk factors for strabismus include:
- Prematurity
- Amblyopia
- Refractive error, particularly anisometropia
- Family history of strabismus
- Craniofacial disorders
- Cranial nerve palsies
- Poor vision in one or both eyes
- Thyroid disease
- Genetic syndromes
- Demyelinating disease
- Central nervous system disorders
- Neuromuscular disorders [2]
Diagnosis
Strabismus can be diagnosed with a comprehensive ocular evaluation. A thorough history is obtained followed by an assessment of the visual acuity, stereoacuity, pupils, sensorimotor testing, ductions and versions, slit lamp examination, cycloplegic refraction and dilated fundus examination. The amount of misalignment can be measured by a variety of methods based on the age of the patient. Measurements are taken in the nine cardinal positions of gaze in addition to right head tilt, left head tilt and at near. The magnitude of deviation will help determine the type and amount of surgery to be performed, as does the presence of any pattern deviation.
Management
General
The treatment of strabismus may consist of glasses, patching, prisms, eye exercises and/or eye muscle surgery. These may be utilized alone or in combination. This topic will focus on the goals, pre-operative evaluation, and surgical procedure for horizontal strabismus surgery. Information on related surgical topics may be found at:
- [Strabismus Surgery Under Topical Anesthesia ]
- Adjustable Sutures for Strabismus Surgery
- Strabismus Surgery, Vertical
- Transposition Surgeries in Strabismus
Horizontal Strabismus Surgery
The primary goal of strabismus surgery is to improve the alignment of the eyes. Additional goals are to re-establish or expand the field of single binocular vision, increase stereoacuity, improve ocular strain related to intermittent deviations, decrease visual confusion, improve abnormal head posture and restore peripheral visual field. [3] Strabismus surgery can also help improve disfigurement, which can have psychosocial and socioeconomic impacts. In a study by Olitsky et al., patients without strabismus had their photos digitally altered to create the appearance of strabismus. Study subjects were then asked to judge the photos and rate personality characteristics and employment capability of the strabismic and non-strabismic patients. The study found, “Overall, the strabismic faces were judged significantly more negatively than the non-strabismic face.” [4]
Pre-operative Evaluation
Once it is decided to proceed with strabismus surgery, a determination is made by the ophthalmologist as to which muscles will be operated on. A muscle can be surgically weakened (recession) or tightened (resection or plication). Additionally, a muscle’s insertion can be transposed to change the direction of its force. Which muscles will be operated on, the type of surgery, and the amount of surgery are dependent on the type and amount of deviation. The surgeon should take into account the patient’s vision, comitance of the deviation and history of any prior surgery.
Surgical Decision
The planned amount of recession (weakening) or resection or plication (strengthening) of muscles is derived from retrospective analyses of dose response curves. There are multiple surgical tables published which list the millimeters of recession or resection of a muscle based on prism diopters of deviation. These tables provide a general guideline and are not a precise predictor of results. The variability in surgical results is dependent not only on the surgeon’s technique but also on the anatomy and pathology of the patient’s disease. In horizontal strabismus surgery, a decision must be made whether to perform recession, resection or a recess-resect procedure. There is no definitive answer as to which procedure is better in most situations, thus is it dependent on the patient’s underlying deviation as well as the surgeon’s experience. The disadvantage of recession is that large recessions of muscles can create limitation in the field of action of that muscle. The disadvantage of resections is that discomfort is greater and there is a limit to the amount of resection of a muscle that can be done. For example, it recommended not to exceed 7 mm for a medial rectus resection and not to exceed 10 mm for a lateral rectus resection to help keep the portion of resected tissue confined to tendon and also to help prevent globe retraction.[5]
There are modifications to horizontal strabismus surgery which can address secondary deviations. Muscles can be vertically transposed to change the vector force. [6] A and V patterns of esotropia and vertical deviations can be corrected by vertical transposition of the horizontal muscles (Medials to the Apex, Laterals to the Empty space = MALE). In patients with limitation of motility in a certain direction, the duction deficit can be matched by placing a posterior fixation suture (Faden procedure) on the contralateral yolk muscle. [7] [8] [9] For very small deviations, a marginal myotomy or central tenotomy can be performed.[10][11]
Procedure Techniques and Instrumentation
This section outlines common strabismus surgical techniques and instrumentation. Note that techniques vary widely and there are many variations of the techniques described below.
Anesthesia and Prep
Prior to surgery a decision is made as to the type of anesthesia to be performed. Options for anesthesia include general, retrobulbar or peribulbar block, sub-Tenon’s injections, or topical. Considerations for anesthesia selection include the laterality of surgery, age of the patient, and comorbid medical conditions. Once in the operating room, the periorbital skin is sterilized with povidone-iodine or hexachlorophene, after which the ocular surface is rinsed with half-strength povidone-iodine solution. Draping of the face and head is performed to maintain sterility.
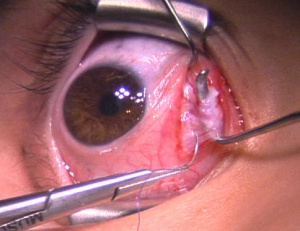
Isolating the muscle
A lid speculum is used to retract the lids as well as keep the eyelashes out of the surgical field. Forced ductions are performed to identify any restrictions or limitations. Depending on the type of surgery to be performed and the surgeon preference, the first incision through conjunctiva is made either in the fornix or at the limbus. A limbal incision may provide better exposure and is thought to cause less scarring because Tenon’s capsule is not as traumatized.[12] However, a limbal incision is thought to affect the anterior segment blood supply more and can be more uncomfortable post-operatively. Fornix incisions have the advantage of better cosmetic appeal post-operatively with less risk to the anterior segment circulation. Dissection is performed to bare sclera, through the conjunctiva, Tenon’s capsule and the intermuscular septum. A Stevens or similar hook is then passed between Tenon’s and sclera, with the plane of the hook parallel to the insertion of the muscle. Traction is placed on the hook towards the limbus to isolate the fibers of the muscle insertion. A larger muscle hook, such as a Jameson, Helveston or Greene hook, is then passed behind the Stevens hook to ensure all muscle fibers are isolated. The insertion of the muscle is then exposed by removing any Tenon’s attachments if performing a limbal incision or by freeing up and retracting the conjunctiva and draping it over the toe of the hook if using a fornix incision. The intermuscular septum at the toe of the hook is incised and special attention is made to ensure all muscle fibers are obtained with a pole test. The muscle is carefully cleaned of all its fascial attachments and check ligaments.
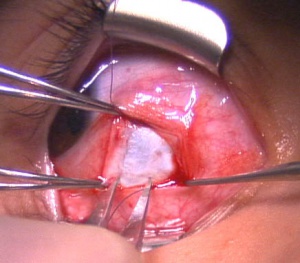
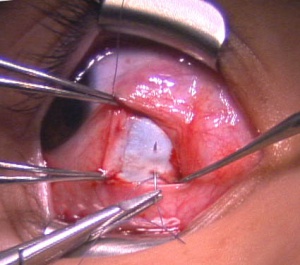
Recession
For a recession, the anterior insertion of the muscle is cleaned and adequately exposed. A double armed 6-0 suture on a spatulated needle is used to secure the muscle insertion (Figure 1). Absorbable sutures such as Vicryl (Ethicon) are commonly used. The muscle is secured in a manner to facilitate a recession via scleral suturing or a hang-back technique. For scleral suturing, a partial thickness muscle pass exiting at the muscle margin is made followed by a full thickness single or double locking bite at both the superior and inferior poles. For the hang-back technique, a central locking bite is made first, followed by the procedure described above. The muscle is disinserted from the globe by placing traction on the muscle hook and the sutures to keep them away from the insertion. Westcott scissors are then used to disinsert the muscle from the sclera. The cut stump of the insertion remaining on the sclera is grasped with forceps at both the superior and poles to maintain orientation of the globe. For scleral suturing, calipers set at the predetermined amount of recession are used to mark the distance posterior from the poles of the original insertion for placement of the muscle (Figure 2). The posterior sclera is marked to correspond with both the superior and inferior aspects of the insertion. The needles attached to the previously disinserted muscle are passed partial thickness through the sclera with visualization of the needle through the superficial sclera lamellae (Figure 3). The direction of the pass is angled slightly anterior to parallel with the insertion. Special caution is taken to ensure that a perforation or penetration of the globe does not occur. This is repeated with the second arm of the suture which is passed at the second marked site posterior to the insertion. The scleral exit sites of the needles usually are closely approximated. The “crossed sword” technique is thought to allow for a more secure knot. The sutures are then pulled anteriorly to bring the muscle up to the new recessed position on the sclera. The sutures are then tied and trimmed. For the hang-back technique, after the muscle has been disinserted, both arms of the suture are passed through half-thickness sclera at the original insertion and pulled up to the insertion. The sutures are clamped with a locking needle driver and calipers are used to measure the number of millimeters for the intended recession from the exit of the scleral tunnels. The sutures are securely tied with 3 square knots and cut. The muscle is then allowed to retract in a hang-back fashion and the amount of recession is verified with calipers.
Medial Rectus Recession Under Topical Anesthesia HD
Resection
For a resection, once the insertion is isolated and cleaned, calipers are used to measure the amount of muscle to be resected from the insertion. A double armed 6-0 suture is then used to secure the muscle at the marked position with a central locking bite, partial thickness muscle passes and full thickness locking bites at the superior and inferior edges. A straight clamp is placed anterior to the previously passed sutures. The muscle is disinserted from the globe and the stump of insertion is grasped with locking forceps to stabilize the globe. The portion of muscle to be resected is excised from the clamp. The cut muscle edge is then cauterized. After the clamp is removed, the sutures are secured to the sclera at the original insertion site with partial thickness scleral passes. The sutures are then tightened and tied.
An alternative to resection is plication. The initial portions of the procedure to isolate and secure the muscle are similar to the resection. The suture poles are then attached to sclera just anterior to the muscle insertion using partial thickness passes through sclera. The sutures are then tightened to pull the muscle forward, using a Stevens muscle hook to fold the muscle under the plication (if needed). The sutures are then tied and cut. [13]
There is an alternative method to plication surgery as described above which includes no scleral passes to be made. This technique is exactly the same as described above for the plication procedure. However the suture poles are then inserted through the muscle belly right at the insertion site. The sutures are then tightened to pull the muscle forward, using a Stevens muscle hook to fold the muscle under the plication (if needed).
Lateral Rectus Resection Unedited HD
Closing the Conjunctiva
Upon completion of a horizontal muscle surgery, the conjunctiva is approximated and closed. The type of suture varies from Vicryl to chromic to gut. Alternatively, some surgeons close with cautery or tissue glue or choose not close a fornix incision.
Follow Up
The postoperative care of patients usually involves examination within the first week to first month after surgery. If an adjustable suture is used, the patient is seen anywhere from the same day of surgery to as late as 5-7 days post-operatively, depending on the technique. Postoperative care regimens vary, but may include topical and/or oral antibiotics, topical steroids or topical NSAIDs. Subsequent follow-up is usually 1-3 months after surgery to allow for stabilization of the alignment.
Complications
A comprehensive discussion of the complications of strabismus surgery can be found at: https://eyewiki.org/Strabismus_Surgery_Complications
Additional Resources
- Free Strabismus Software Download (Squintmaster.com)
- AAPOS Frequently Asked Questions on Strabismus Surgery
- Puente MA Jr, Lipsky SN, Turbert D. Strabismus. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/diseases/strabismus-list. Accessed February 22, 2023.
References
- ↑ American Association for Pediatric Ophthalmology and Strabismus. “Strabismus.” https://aapos.org/glossary/strabismus. Last updated 2020 Oct 07. Accessed 2021 Mar 18.
- ↑ Chew E, Rernaley N, Tamboli A, Jialiang Z, Podgor M, Klebanoff M. Risk factors for esotropia and exotropia. Arch Ophtahlmol. 10:112, 1994.
- ↑ Mills MD, Coats DK, Donahue SP, Wheeler DT; American Academy of Ophthalmology. Strabismus surgery for adults: a report by the American Academy of Ophthalmology. Ophthalmol. 6:111, 2004.
- ↑ Olitsky SE, Sudesh S, Graziano A, Hamblen J, Brooks SE, Shaha SH. The negative psychosocial impact of strabismus in adults. J AAPOS. 4:3, 1999.
- ↑ Wright K: Color Atlas of Strabimus Surgery. Philadelphia, JB Lippincott, 1991.
- ↑ Jones ST. Treatment of hypertropia by vertical displacement of horizontal recti. Am Orthopt J 27:107, 1977.
- ↑ Paliaga GP, Braga M: Passive limitation of adduction after Cüppers’s "Fadenoperation" on medial recti. Br J Ophthalmol 73:633, 1989.
- ↑ Noorden GK von: Posterior fixation suture in strabismus surgery. In Symposium on Strabismus: Transactions of the New Orleans Academy of Ophthalmology. St Louis, Mosby–Year Book, 1978, p 307.
- ↑ Scott AB. The faden operation: mechanical effects. Am Orthopt J. 27, 1977.
- ↑ Helveston EM, Cofield DD.: Indications for marginal myotomy and technique. Am J Ophthalmol 70:574, 1970.
- ↑ L. Faber JTHN de, Noorden GK von: Medial rectus muscle marginal myotomies for persistent esotropia. Am J Ophthalmol 112:702, 1991.
- ↑ Noorden GK von: The limbal approach to surgery of the rectus muscles. Arch Ophthalmol 80:94, 1968.
- ↑ Alkharashi M, Hunter DG. Reduced surgical success rate of rectus muscle plication compared to resection. J AAPOS. 2017 Jun;21(3):201-204.