Solitary Fibrous Tumor
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Solitary fibrous tumors of the orbit are rare spindle-shaped neoplasias that typically present as benign orbital masses in middle-aged adults and are typically cured with complete surgical excision.
Etiology
Solitary fibrous tumors are composed of spindle-shaped cells and were originally considered a neoplasia of the mesothelium due to their propensity to arise from the pleura and mediastinum. In fact, in the original description by Klemper and Rabin in 1931 it was called a “localized mesothelioma.”[1] Since its classic description, solitary fibrous tumors have been described in multiple extraserosal tissues including the lung, liver, thyroid, paranasal sinuses, and orbit, making it less likely to actually be derived from mesothelium, and more likely to be from a fibroblastic differentiated cell type in the submesothelial mesenchyme.[2] [3] [4] Possible cells of origin could include endoneural dendritic cells, dermal dendrocytes, or pericytes. Their electron microscopic appearance and dense staining with CD34 and vimentin are also consistent with a fibroblastic differentiated cell line.[5] [6] [7]
Risk Factors
Higher rates of recurrence and malignant transformation can occur in tumors that are not completely excised. Malignant transformation has also been reported to occur following radiation therapy.[8]
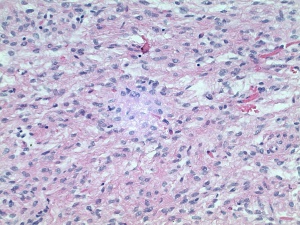
General Pathology
Solitary fibrous tumors of the orbit are mostly benign, but malignant forms of the tumor can occur de novo or transform from a low grade lesion.[9] Solitary fibrous tumors share a common histopathologic morphology with hemangiopericytomas, giant cell angiofibromas, and fibrous histiocytomas, and in fact, some have recommended classifying all these tumors together under the general term solitary fibrous tumor.[10] All of these tumors are characterized by haphazardly arranged fibroblast-like cells, indistinct nucleoli, prominent vasculature with perivascular fibrosis, and variable stromal collagen. Solitary fibrous tumors, in particular, demonstrate a “patternless pattern” on microscopic examination with abundant “rope-like” collagen in between tumor cells.[6] [11] Histopathologic features that suggest a more aggressive variant include: high mitotic rates of greater than 4/10 high power fields, necrosis, hypercellularity, nuclear pleomorphism, and high MIB-1 labeling (a cell proliferation marker).[12] In addition to their typical light microscopic appearance, solitary fibrous tumors display a typical pattern of immunohistochemical staining. These tumors stain strongly and diffusely with vimentin, BCL2, and CD34. They stain negatively for keratin, cytokeratin, epithelial membrane antigen, S100, smooth muscle actin, and desmin.[2] [6] This immunohistochemical staining pattern helps to differentiate solitary fibrous tumors from neural tumors, smooth muscle tumors, nodular fasciitis, and fibrous histiocytomas. Distinguishing solitary fibrous tumor from hemangiopericytomas can be difficult since they can have the same light microscopic appearance and both stain immunohistochemically for vimentin, BCL2, and CD34. It is the diffuse and strong staining with CD34 that differentiates it from a hemangiopericytoma, which has weak and patchy CD34 staining.[6] Solitary fibrous tumors have a tendency to present in the superior aspect of the orbit, but can be found anywhere in the orbit including the lacrimal gland and lacrimal gland fossa.[9] [11] [13] Rarely, intracranial extension can occur,[14] even in the absence of malignant histopathology.[15] Recurrent tumors have been reported to invade surrounding orbital tissues, into the paranasal sinuses, and into the intracranial space, and may or may not show malignant histopathologic transformation.[2] [15] There has been one reported case of distant metastases from a primary orbital solitary fibrous tumor.[14]
Primary Prevention
Solitary fibrous tumors that are not completely excised have a high risk for recurrence. Therefore, complete surgical excision is recommended. One case in the literature to date has documented radiation therapy as a possible risk factor for malignant degeneration.[8] Therefore, caution should be taken in irradiating these lesions.
Diagnosis
History
Solitary fibrous tumors of the orbit are typically benign slow growing lesions. As such, patients typically present with months to years of progressive proptosis. There is about equal incidence between males and females. Patients can present as young as 5 years old to as old as 77 years old, with the average age of presentation in the forties.[8] [11] [16] Occasionally diplopia, decreased vision, and rarely pain may also be elicited from the patient’s history
Physical examination
The most common physical exam finding in patients with solitary fibrious tumors is proptosis, so exophthalmometry measurements should be documented. These lesions can often times be located anteriorly in the orbit, permitting direct palpation of the lesion. Patients may have lid swelling and ptosis as their only physical exam finding, so marginal reflex distances should be recorded.[7] Patients should be examined for extraocular muscle motility and optic nerve appearance and function. If there is concern for compression of the optic nerve, the presence of a relative afferent pupillary defect should be checked, and color vision testing and automated visual field testing should be considered.
Signs
About 75% of patients present with proptosis, and 15% present with eyelid swelling, visual disturbance, or a palpable mass. Less commonly (3% of the time) ptosis is the presenting symptom.[11] Imaging studies typically reveal a well circumscribed mass lesion that most commonly is found supero-medially, but can be present anywhere in the orbit, including the lacrimal gland fossa.[11] [13] [16]
Symptoms
Patients present with proptosis and possibly ptosis, eyelid swelling, tearing, diplopia or decreased vision.[11] Malignant infiltrating lesions can sometimes cause pain.
Clinical diagnosis
An orbital mass lesion is either visible on examination or suspected based on clinical exam measurements of exophthalmos, globe displacement, decreased extraocular muscle motility, and possible deterioration of optic nerve function.
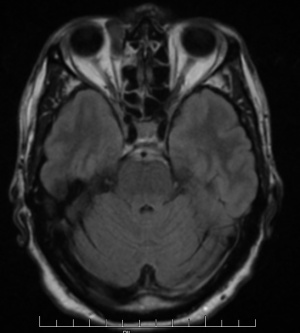
Diagnostic procedures
Ultrasonography of solitary fibrous tumors demonstrates low internal reflectivity with sound wave attenuation.[17] CT scan and MRI can be helpful to narrow the differential diagnosis. However, there is variability in the radiographic and MRI appearance of solitary fibrous tumors, so definitive diagnosis can only be made with histopathologic and immunohistopathologic examination. Generally speaking, solitary fibrous tumors will appear as a well-defined soft tissue mass on CT imaging that strongly enhances and may show bony remodeling if the tumor is longstanding. Significant bony changes in patients who have a history of prior tumor excision are suggestive of possible malignant degeneration.[18] Solitary fibrous tumors tend to be hypointense on T1 weighted images and iso/hypo-intense on T2 weighted images. Intralesional pseudocystic cavities are rare, but have been described,[19] and when present, may suggest malignant transformation in recurrent tumors.[20] After administration of contrast, they also tend to show a washout time intensity curve pattern. They have an apparent diffusion coefficient (ADC) value of more than 1.0 x 10-3mm2/s.[18]
Differential diagnosis
The differential diagnosis includes: cavernous hemangiomas; neural tumors such as gliomas, meningiomas, schwanomas, and neurofibromas; smooth muscle tumors such as leiomyomas and leiomyosarcomas; mesenchymal lesions such as giant cell angiofibromas, hemangiopericytomas, or fibrous histiocytomas.
Management
The primary management of solitary fibrous tumors is complete surgical excision. In patients with previous excision of tumor, with a histopathologic diagnosis of a benign solitary fibrous tumor, clinical monitoring with serial exam and imaging can be cautiously considered.[7]
General treatment
En bloc complete surgical excision is the treatment of choice given the tendency for recurrence and possible malignant degeneration in tumors that are not primarily excised. Infiltrating malignant lesions may require exenteration.
Medical therapy
There is no known medical treatment for localized solitary fibrous tumors of the orbit. Radiotherapy may cause malignant degeneration of these tumors, so it should be used with extreme caution. Current chemotherapy regimens have only been applied to non-orbital cases of metastatic solitary fibrous tumors and so far have not been very effective.[21]
Surgery
Complete surgical excision of the lesion or exenteration of infiltrating lesions are the recommended surgical treatments.
Surgical follow up
Routine follow up can be recommended for patients in whom tumors are completely excised. Patients who have incomplete tumor removal should be followed more frequently and should have serial imaging to check for recurrence.
Complications
Complications associated with surgical removal are typical for any orbital surgery including retrobulbar hemorrhage, diplopia, ptosis, strabismus, decreased vision, blindness, or incomplete tumor excision. Incomplete tumor excision may lead to recurrence and/or malignant degeneration.
Prognosis
Prognosis is excellent for tumors that are completely excised. Of the cases described in the literature, about 75% of solitary fibrous tumors display a benign course; and 25% showing invasion to adjacent tissues, recurrence, or distant metastasis.[11] Of the tumors that recur, about 95% demonstrate benign histopathology, and up to 75% of histopathologic confirmed malignant tumors display non-aggressive clinical behavior.[11] Tumor recurrence has been documented to occur as few as 3 months following primary excision to as long as 40 years following primary removal.[11]
References
- ↑ Klemperer P RC. Primary neoplasms of the pleura; a report of five cases. Arch Pathol. 1931;11:385-412.
- ↑ Jump up to: 2.0 2.1 2.2 Bernardini FP, de Conciliis C, Schneider S, Kersten RC, Kulwin DR. Solitary fibrous tumor of the orbit: is it rare? Report of a case series and review of the literature. Ophthalmology. 2003;110(7):1442-1448.
- ↑ Krishnakumar S, Subramanian N, Mohan ER, Mahesh L, Biswas J, Rao N a. Solitary fibrous tumor of the orbit: a clinicopathologic study of six cases with review of the literature. Surv Ophthalmol. 2003;48(5):544-554.
- ↑ McElvanney AM, Noble JL, O’Donovan DG, Bonshek RE, Banerjee SS. Solitary fibrous tumour: an atypical presentation within the orbit. Eye (Lond). 1996;10 ( Pt 3):396-399.
- ↑ Dorfman DM, To K, Dickersin GR, Rosenberg AE, Pilch BZ. Solitary fibrous tumor of the orbit. Am J Surg Pathol. 1994;18(3):281-287.
- ↑ Jump up to: 6.0 6.1 6.2 6.3 Westra WH, Gerald WL, Rosai J. Solitary fibrous tumor. Consistent CD34 immunoreactivity and occurrence in the orbit. Am J Surg Pathol. 1994;18(10):992-998.
- ↑ Jump up to: 7.0 7.1 7.2 Tam ES, Chen EC, Nijhawan N, Harvey JT, Howarth D, Oestreicher JH. Solitary fibrous tumor of the orbit: a case series. Orbit. 2008;27(6):426-431.
- ↑ Jump up to: 8.0 8.1 8.2 Blandamura S, Alaggio R, Bettini G, Guzzardo V, Valentini E, Bedogni A. Four cases of solitary fibrous tumour of the eye and orbit: one with sarcomatous transformation after radiotherapy and one in a 5-year-old child’s eyelid. J Clin Pathol. 2014;67(3):263-267.
- ↑ Jump up to: 9.0 9.1 Wang X, Qian J, Bi Y, Ping B, Zhang R. Malignant transformation of orbital solitary fibrous tumor. Int Ophthalmol. 2013;33(3):299-303.
- ↑ Furusato E, Valenzuela I a, Fanburg-Smith JC, et al. Orbital solitary fibrous tumor: encompassing terminology for hemangiopericytoma, giant cell angiofibroma, and fibrous histiocytoma of the orbit: reappraisal of 41 cases. Hum Pathol. 2011;42(1):120-128.
- ↑ Jump up to: 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 11.8 Le CP, Jones S, Valenzuela AA. Orbital Solitary Fibrous Tumor : A Case Series with Review of the Literature. Orbit. 2014;33(2):145-151.
- ↑ Vallat-Decouvelaere A V, Dry SM, Fletcher CD. Atypical and malignant solitary fibrous tumors in extrathoracic locations: evidence of their comparability to intra-thoracic tumors. Am J Surg Pathol. 1998;22(12):1501-1511.
- ↑ Jump up to: 13.0 13.1 Son DH, Yoo SH, Sa H-S, Cho K-J. A solitary fibrous tumor with giant cells in the lacrimal gland: a case study. Korean J Pathol. 2013;47(2):158-162.
- ↑ Jump up to: 14.0 14.1 Parrozzani R, Fusetti S, Montesco C, Favero V, Midena E. Biphasic solitary fibrous tumor of the orbit with distant metastases. Int Ophthalmol. 2013;33(6):701-705.
- ↑ Jump up to: 15.0 15.1 Young TK, Hardy TG. Solitary fibrous tumor of the orbit with intracranial involvement. Ophthal Plast Reconstr Surg. 27(3):e74-e76.
- ↑ Jump up to: 16.0 16.1 hen H, Xiao C-W, Wang T, et al. Orbital solitary fibrous tumor: a clinicopathologic study of ten cases with long-term follow-up. Acta Neurochir (Wien). 2012;154(2):249-255; discussion 255.
- ↑ Lucci LM, Anderson RL, Harrie RP, Mamalis N, Coffin C, Crandall DC. Solitary fibrous tumor of the orbit in a child. Ophthal Plast Reconstr Surg. 2001;17(5):369-373.
- ↑ Jump up to: 18.0 18.1 Kim HJ, Kim H-J, Kim Y-D, et al. Solitary fibrous tumor of the orbit: CT and MR imaging findings. AJNR Am J Neuroradiol. 2008;29(5):857-862.
- ↑ Polomsky M, Sines DT, Dutton JJ. Solitary fibrous tumor of the orbit with multiple cavities. Ophthal Plast Reconstr Surg. 29(5):e117-e119.
- ↑ Graue GF, Schubert HD, Kazim M. Correlation between clinical features, imaging and pathologic findings in recurrent solitary fibrous tumor of the orbit. Orbit. 2013;32(6):375-380.
- ↑ Levard A, Derbel O, Méeus P, et al. Outcome of patients with advanced solitary fibrous tumors: the Centre Léon Bérard experience. BMC Cancer. 2013;13:109.
- Petrovic, A., Obéric, A., Moulin, A. et al. , Ocular adnexal (orbital) solitary fibrous tumor: nuclear STAT6 expression and literature review.Graefes Arch Clin Exp Ophthalmol (2015) 253: 1609. https://doi.org/10.1007/s00417-015-2975-5