Fibrous Histiocytoma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Fibrous histiocytoma is the most common primary mesenchymal orbital tumor in adults. It may involve ocular structures such as the orbit, lids, conjunctiva, and ocular limbus. Most fibrous histiocytomas are benign, but some are locally aggressive and malignant. Malignant fibrous histiocytoma can develop after ocular irradiation for heritable retinoblastoma.[1]
Disease Entity
- ICD9 = 376.9
- ICD10 = H05.9
Disease
A recent review of orbital tumors at the Armed Forces Institute of Pathology has shown that fibrous histiocytoma is the most common primary mesenchymal orbital tumor in adults. It may involve ocular structures such as the orbit, lids, conjunctiva, and ocular limbus. Most fibrous histiocytomas are benign, but some are locally aggressive and malignant. It is usually seen in middle-aged patients (40-60 years).[2] Classification of fibrous histiocytoma has changed over the past few decades, and is now believed to be part of a spectrum of tumors known as solitary fibrous tumors.
Etiology
The site of origin is thought to be a histiocyte or fibroblast, it is most likely a primitive mesenchymal cell with divergent differentiation that expresses fibroblastic, histiocytic, and myofibroblastic phenotypes.
Risk Factors
Malignant fibrous histiocytoma can develop after ocular irradiation for heritable retinoblastoma.
General Pathology
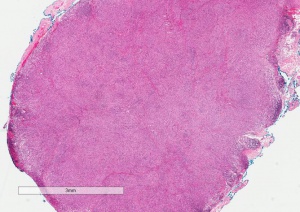
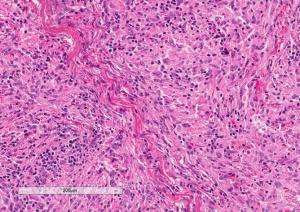
Histologically, fibrous histiocytoma is a mixture of spindle-shaped fibroblasts and histiocytes arranged in "storiform" or cartwheel-like pattern.[3] Pathologic analysis and diagnosis are often challenging, usually based on a combination of light microscopy, immunohistochemistry, and electron microscopic findings. Fibrous histiocytoma stains positive for vimentin. Based on pathologic criteria, orbital fibrous histiocytoma has been divided into benign (~60% incidence) and malignant (~40%) categories.
Other fibrous tumors, such as fibrosarcoma, fibroma, hemangiopericytoma and solitary fibrous tumors can be easily confused histologically with fibrous histiocytoma. A herringbone pattern is usually found in fibrosarcoma. A "patternless pattern" and CD34 staining is found most commonly in solitary fibrous tumor. The tumor can be richly vascularized, and hence, easily confused with hemangiopericytoma
Primary prevention
Avoidance of orbital radiation in patients who are affected by hereditary retinoblastoma is the only known environmental factor in preventing fibrous histiocytoma.
Diagnosis
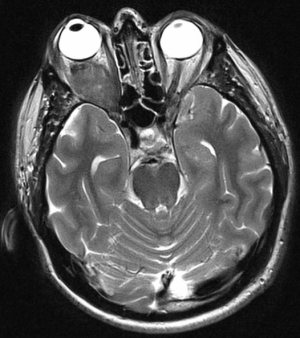
Orbital fibrous histiocytoma can occur in adulthood or childhood. It appears as a circumscribed, homogeneous, soft tissue orbital mass that can produce proptosis and decrease in vision. Although it can occur anywhere in the orbit, it is usually confined to the orbital soft tissues. Differentiating fibrous histiocytoma from other common orbital tumors may present a diagnostic dilemma even with advanced time-resolved contrast imaging.[4]
In rare circumstances, it can invade the globe.
History
Patients typically present with painless proptosis and a mass on orbital imaging. One study shows that most common signs and symptoms were proptosis (60 %), mass (46%), and decreased vision (25%).[5]
Physical examination
A complete eye exam with measurement of exophthalmos and retropulsion.
Signs
Proptosis (or bulging of the eye).
Symptoms
Decreased vision, dry eye, or other symptoms resulting from proptosis may occur.
Clinical diagnosis
History, imaging, physical examination, and high clinical suspicion are required to make the diagnosis of fibrous histiocytoma.
Diagnostic procedures
Orbital CT, MRI, and/or time-resolved contrast kinetics imaging, will demonstrate a well-circumscribed soft tissue mass. It can mimic a schwannoma or cavernous hemangioma. It rarely erodes bone or extends intracranially. Biopsy with special immunohistochemistry staining is required to make a definitive diagnosis.
Differential diagnosis
Cavernous hemangioma (cavernous venous malformation), rhabdomyosarcoma, hemangiopericytoma, schwannoma, and other orbital tumors should be included in the differential diagnosis.
Management
The preferred management is complete surgical resection of the mass within its capsule. The literature has reported that incomplete excision can lead to recurrence of disease and malignant transformation in some cases. Advanced cases may require orbital exenteration or irradiation.
General treatment
Complete surgical excision is the treatment of choice. Exenteration may be required in advanced cases.
Medical therapy
Chemotherapy and radiotherapy have so far been limited in the treatment of fibrous histiocytoma.
Surgery
Orbital surgery should be performed by a qualified oculoplastic surgeon. The surgeon will choose the best approach to the orbit based on the location of the tumor, with the goal of complete excision. With invasive tumors, orbital exenteration may be required.
Surgical follow up
The ten-year survival of patients with benign, locally aggressive, and malignant fibrous histiocytoma was 100 percent, 92 percent, and 23 percent, respectively.[5]
Complications
Retrobulbar hemorrhage, infection, loss of vision, incomplete excision, recurrence with malignant transformation, and loss of the eye are potential complications of orbital surgery.
Prognosis
The rate of recurrence was 31 percent for the benign tumors, 57 percent for the locally aggressive tumors, and 64 percent for the malignant tumors in one study.[5]
References
- ↑ Shields, Jerry. Shields, Carol. Eyelid, Conjunctival, and Orbital Tumors. Lippincott Williams and Wilkins. 2008.
- ↑ Yanoff M, Duker J. Ophthalmology 3rd Ed. Pages 1453-1454
- ↑ Yanoff, M. Sassani, J.W. Ocular Pathology sixth edition. Elsevier 2009.
- ↑ Warner EJ, Burkat CN, Gentry LR. Orbital fibrous histiocytoma mimicking cavernous hemangioma on dynamic contrast-enhanced MRA imaging. Ophthal Plast Reconstr Surg. 2013 Jan-Feb;29(1):e3-5. doi: 10.1097/IOP.0b013e31825412f7.
- ↑ Jump up to: 5.0 5.1 5.2 Font RL, Hidayat AA. Fibrous histiocytoma of the orbit. A clinicopathologic study of 150 cases. Hum Pathol. 1982 Mar;13(3):199-209.