Retrobulbar Hemorrhage
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Retrobulbar hemorrhage (RBH) is a rapidly progressive, sight-threatening emergency that results in an accumulation of blood in the retrobulbar space. [1] The blood accumulation can lead to proptosis and an increased IOP that may result in stretching of the optic nerve and blockage of ocular perfusion leading to venous and/or arterial occlusive process. [2]
Etiology
RBH can occur due to orbital trauma, a complication of eyelid or orbital surgery, or any process that can affect blood supply to the eye, such as arteriovenous malformations, orbital varicosities, or lymphangiomas. It can be potentiated by the use of anticoagulation medication.[1]
Risk Factors
Risk factors include postoperative valsalva maneuvers such as vomiting or coughing after eyelid or orbital surgery. Additionally, hypertension has been shown to be a risk factor for retrobulbar hemorrhage in post-operative patients. One study has shown that perioperative aspirin use can lead to hemorrhage, however another study did not achieve this finding. [3] [4] In addition, retrobulbar anesthesia has been shown to be a risk factor for RBH. Orbital trauma can also lead to retrobulbar hemorrhage. Multiple studies have found an association between the use of anticoagulation medication and retrobulbar hemorrhage in trauma and postoperative patients. [3],[4][5]
Epidemiology
Retrobulbar hemorrhage is rare. The incidence of RBH depends on the etiology of the injury. As previously discussed, RBH can result from orbital trauma or postoperative complications of eye surgery. In a study that examined ER visits for orbital trauma, of the 1386 patients suffering orbital trauma, only 50 patients had retrobulbar hemorrhage. [6] In another study examining 68 orbital fractures, only six patients developed orbital hemorrhages. Two of the six were post-operative complications of surgical reconstruction of the orbit. [4] Although the incidence of retrobulbar hemorrhage is low, the association between RBH and blindness is strong, with an incidence around 48%. [7] However, in patients that received proper and prompt treatment, the incidence of blindness was only 0.14%, demonstrating the importance and benefit of treatment. [6]The large difference in the incidence of blindness is due to the etiology and severity of the initial injury.
Anatomy
In order to appreciate the pathophysiology of retrobulbar hemorrhage, it is important to understand the anatomy of the orbital compartment. The compartment surrounds the globe of the eye. It is comprised anteriorly of the orbital septum, a fibrous sheath originating from the orbital rims.[1] The orbital septum is attached to the lateral canthal tendon and the lateral orbital rim. The medial, lateral, as well as the posterior sides are bordered by orbital bones. [1] (Figure 1) The optic nerve and many blood vessels that supply the eye travel through the orbital compartment. Due to the compactness of the region and location of the vessels, this creates an area that can accumulate blood.
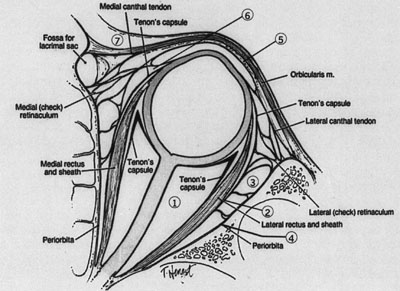 (Figure 1: Illustration of eye and retrobulbar space) [8]
(Figure 1: Illustration of eye and retrobulbar space) [8]
Pathophysiology
Due to retrobulbar space being surrounded by bone medially, laterally, and posteriorly, any increase in pressure in the space will result in a forward shift. Trauma or post-operative complications can lead to bleeding in the space, usually from the infraorbital artery or one of its branches. [9] The eye can handle slight forward displacement, however any further proptosis can result in optic nerve defects, as the optic nerve reaches its stretch limitations. Essentially, retrobulbar hemorrhage results in a compartment syndrome which can lead to compression or ischemia of the optic nerve, blockage of the optic nerve venous drainage, or a central retinal arterial occlusion leading to vision loss. [2]
Diagnosis
The diagnosis of RBH is clinical and depends on the history of the patient. Diagnostic clues of RBH include severe pain, double vision, difficulty opening the lids, proptosis and/or loss of vision. [6] If patients are victims of trauma, periorbital ecchymosis and eyelid hematoma may be seen. [1] Due to the severity of RBH and the possibility of vision loss, imaging modalities are usually not recommended for initial diagnostic purposes, as this is a clinical diagnosis and treatment must be prompt. [2] However, a CT scan can be useful to visualize the orbits (Figure 2), particularly to rule out concomitant injuries in cases of trauma or when the origin of the bleeding is unknown. Decrease in extraocular motility is a concerning feature of pending optic neuropathy even if proptosis is minimal and IOP is normal.
 (Figure 2: CT scan demonstrating hematoma and proptosis on the right side) [10]
(Figure 2: CT scan demonstrating hematoma and proptosis on the right side) [10]
History and Physical
It is important to note the history of the patient. As discussed, RBH can result from trauma or a postoperative complication. Visual acuity, intraocular pressure, and a full ophthalmologic exam, including ocular motility, is required. It is important to note the pupil responses to assess for an afferent pupillary defect. [9] Severity of RBH can typically be determined by the physical exam findings. [1]
Symptoms
Symptoms of RBH include pain, periorbital ecchymosis, eyelid hematoma, ophthalmoplegia, proptosis, visual loss, subconjunctival hemorrhage, nausea, and vomiting.
Differential
Retrobulbar hematoma, Acute angle closure glaucoma, or other etiologies of orbital compartment syndrome.
Management
Vision loss is a major concern of retrobulbar hemorrhage. As a result, intervention must be rapid. Firstly, postoperative patients with surgery to the eye or injections to the retrobulbar space must be carefully monitored. Development of hemorrhage usually occurs within the first 24 hours. [3] In patients with vision loss, proptosis, extraocular movement deficiencies, or any sign of elevated IOP, lateral canthotomy with cantholysis has been shown to be an effective first line treatment. [9] It is crucial to decompress the orbit and relieve pressure to prevent compartment syndrome and permanent vision loss. If the symptoms do not improve with lateral canthotomy/cantholysis, inferior septectomy and/or surgical treatment can be performed. The inferior lateral orbitomy in which blunt dissection is performed through the lateral cantholysis incision has also been reported to evacuate retrobulbar hemorrhage that may be entrapped within the numerous fibrous Koorneef's septae in the orbit (Burkat CN, Lemke BN. Retrobulbar hemorrhage: inferolateral anterior orbitotomy for emergent management. Arch Ophthalmol. 2005 Sep;123(9):1260-2). A pre-canthal "one-snip" approach of making a single full-thickness eyelid incision with tenotomy scissors, 5 mm medial to the lateral canthal angle, that is approximately 15 mm in length to connect to the inferior orbital rim has been shown to achieve a decrease in intraocular pressure in a cadaver model of retrobulbar hemorrhage (Blandford AD, Young JM, Arepalli S, Li A, Hwang CJ, Perry JD. Paracanthal "One-Snip" Decompression in a Cadaver Model of Retrobulbar Hemorrhage. Ophthalmic Plast Reconstr Surg. 2018 Sep/Oct;34(5):428-431.) Emergent decompression through these techniques has been shown to lead to decreased intraocular pressure and vision improvement. Other recent studies demonstrate efficacy using a simple vertical split incision, particularly useful in the emergency room setting with providers not familiar with eyelid anatomy.
[11] To avoid permanent damage, it has been shown that intervention must be carried out within 2 hours of onset. [9] Surgical management is preferred over medical management due to better results. However, medical management can be used in conjunction with surgery. Some recommend IV acetazolamide 500 mg or IM/IV hydrocortisone 100 mg to be used to decrease pressure. [9] Proper management of patients can prevent permanent vision loss.
Additional Resources
- Porter D, Vemulakonda GA. Blood Pressure. American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/anatomy/blood-pressure-list. Accessed January 06, 2023.
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 Kent, T, Morris, C. Evaluation and Management of Orbital Hemorrhage. Ophthalmic Pearls: Orbit found on www.aao.org. January 2011 .
- ↑ Jump up to: 2.0 2.1 2.2 Goodall K L, Brahma A, Bates A, Leatherbarrow B. Lateral canthotomy and inferior cantholysis: an effective method of urgent orbital decompression for sight threatening acute retrobulbar haemorrhage.Injury. 1999;30(7):485–490.
- ↑ Jump up to: 3.0 3.1 3.2 Hass A N, Penne R B, Stefanyszyn M A, Flanagan J C. Incidence of postblepharoplasty orbital hemorrhage and associated visual loss. Ophthal Plast Reconstr Surg. 2004;20(6):426–432
- ↑ Jump up to: 4.0 4.1 4.2 Maurer P, Conrad-Hengerer I, Hollstein S, Mizziani T, Hoffmann E, Hengerer F. Orbital haemorrhage associated with orbital fractures in geriatric patients on antiplatelet or anticoagulant therapy. Int J Oral Maxillofac Surg. 2013 Dec;42(12):1510-4
- ↑ Cionni RJ, Osher RH. Retrobulbar hemorrhage. Ophthalmology98(8),1153–1155 (1991)
- ↑ Jump up to: 6.0 6.1 6.2 Fattahi T, Brewer K, Retana A, Ogledzki M. Incidence of retrobulbar hemorrhage in the emergency department. J Oral Maxillofac Surg. 2014 Dec;72(12):2500-2
- ↑ Ansari, M.H. Blindness after Facial Fractures: A 19 year retrospective study. J Oral Maxillofac Surg 63:229-237, 2005.
- ↑ Kersten, R, Neard J. Orbital Surgery. Eyecalcs.com. Chapter 86. Available from:http://www.eyecalcs.com/DWAN/pages/v5/v5c086.html
- ↑ Jump up to: 9.0 9.1 9.2 9.3 9.4 Winterton J V, Patel K, Mizen K D. Review of management options for a retrobulbar hemorrhage. J Oral Maxillofac Surg. 2007;65(2):296–299
- ↑ McAllister AR, Sobel RK, Allen RC. Spontaneous Retrobulbar Hemorrhage with Subsequent Orbital Compartment Syndrome. EyeRounds.org. April 18, 2013; Available from:http://www.EyeRounds.org/cases/168-Orbital-Compartment-Syndrome.htm
- ↑ Lee K YC, Tow S, Fong K S. Visual recovery following emergent orbital decompression in traumatic retrobulbar haemorrhage. Ann Acad Med Singapore. 2006;35(11):831–832

