Secondary Intraocular Lens (IOL) Implantation
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Indications
- IOL exchange which can be done for different reasons:
- Incorrect IOL power
- IOL luxation
- Opacification of IOL
- Photopsias
- Dissatisfied patient with multifocal IOL
- IOL induced inflammatory response and CMO.
- IOL induced endothlial decompdnsation.
- IOL removal and later 2ndary implantation in chronic endophthalmitis
- After congenital cataract removal in children less than 1-2 years of age.
- After complicated cataract surgery.
- Trauma patients with crystalline lens loss.
- Uveitis patients.
- After refractive surprise.
Patient selection
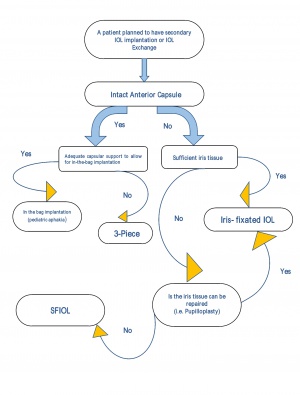
Before making the decision of which secondary IOL implantation technique is suitable to the individual patient, it is important to take several points in consideration.
First, history is important regrading the time of the previous surgey , trauma…..etc.
Second, A detailed anterior segment examination including:
- Conjunctival status including the presence of glaucoma drainage devices.
- Cornea; clarity, edema, pachymetry and specular microscopy to assess the endothelial cell count
- Anterior chamber depth and any evidence of vitreous prolapse in AC.
- Iris and capsule status.
- If an IOL is present; the degree of subluxation and the type of IOL is mportant.
And finally, Posterior segment examination is valuable in case that some conditions limit the postoperative results or might need treatment at the same time of surgery.[1]
Techniques
- Single piece or 3-piece Foldable IOL in the bag
- 3 piece implantation in the sulcus
- Iris fixated IOL ( anterior or retropupillary)
- Scleral fixation
Single piece or 3-piece Foldable IOL in the bag
A novel technique was described for secondary IOL implantation in the bag for pediatric aphakia in 2011.
In this in the bag technique, the presence of soemmering’s ring and proliferating epithelial cells helped in maintenance of the potential space between the anterior and posterior capsule. This space between the two capsules is opened with an MVR 360 degree in small can-opener movement and the residual cortical material present is aspirated by a 20 gauge vitrectomy hand-piece in bimanual closed chamber technique followed by single piece foldable or 3-piece IOL implantation.[2]
3 piece implantation in the ciliary sulcus
Usually 3 piece IOL is implanted in the ciliary sulcus with/without optic capture. The presence of intact anterior capsulorrhexis is a perquisite for this technique. Optic capture provides more stability and more centration of the IOL, preventing vitreous prolapse anterior to the IOL in addition to causing less myopic shift in comaprison with sulcus fixation alone.[3]
Various techniques have been described for optic capture including :
- Optic capture through the CCC with haptics in the sulcus.
- Haptics in the sulcus with the optic capture through the posterior rrhexis.
- Haptics in the bag with optic capture through the postreior rrhexis.
- Haptics in the bag with optic capture through the CCC.[4]
Placing the haptics in the ciliary sulcus with optic capture through the CCC is the best way ensuring long term IOL stability, nearly eliminates the risk of phimosis, and tends to decrease zonular damage.
In case of a very young patient or a patient who is expected to be uncooperative for future YAG capsulotomy, putting the haptics in the ciliary sulcus and the pushing the optic through both the CCC and posterior rrhexis which is called “ bicapsular capture “ provides very stable IOL configuration and less risk of decentration.[5]
Iris-fixated IOL ( Anterior or Retropupillary Artisan)
Iris-fixated lenses were first described in 1954 ("collar stud": Epstein 1954, "iris-clip": Binkhorst 1959). In the early 1960s, Collar implanted the first iris-fixated lens after an intra-capsular cataract extraction, but in 1971, Worst came in with the Iris Claw lens, and its modification evolved in the Artisan lens.[6] [7]
Iris claw lens is an effective, predictable and safe option for aphakic eyes without capsule support, compared to other options, it has a quicker visual recovery, better visual outcomes and fewer complications than the other secondary IOL implantation options. Furthermore, its placement can be performed with a lower invasiveness and in a shorter surgical time what reduces the risk of photic retinal damage.[8] [9]
Surgical technique
Iris claw lens can be implanted using either corneal incision or through a scleral tunnel (which is reported to cause less corneal endothelial cell loss, less astigmatism and a lower risk of wound leakage compared to corneal incision). [10] Implantation can be either Antepupillary or Retropupillary. Despite a higher incidence of IOL dislocation, it is reported that the retropupillary fixation offers the advantage with physiological posterior chamber implantation, resulting in a deeper anterior chamber and a lower intraoperative and postoperative risk of corneal de-compensation than anterior fixation. However, there is no evidence available about the best placement method for secondary iris-claw IOL implantation that offers the maximum and earliest visual recovery over many years and the lowest complication rate. A peripheral iridectomy is required to decrease the risk of pupillary block.[11] [12]
Requirements for successful implantation
- Removal of vitreous from the anterior chamber.
- At least 270 degrees of iris tissue with pupil size smaller than 6 mm (suture pupilloplasty may be required to reform pupil to provide this).
- Anterior chamber depth of 3 mm or greater.[13]
Complications
Endothelial cell loss
It is suggested that the corneal endothelial cell loss may be mainly because of a mechanical injury due to the contact between the endothelium and the instruments or the IOL which occurs during the surgical procedure. It is higher in the first year post aphakic Artisan IOL implantation, with a further drop noted over the subsequent years to a lesser extent, this seems to stabilise 3 years post operatively. Güell et al. reported that Artisan IOL implantation caused approximately 10.9% endothelial cell loss in the 3 years follow-up.
Two main risk factors had been identified for endothelial cell loss:
- shallow anterior chamber depth and a shorter distance from IOL edge to the endothelium
- Implantation through a scleral tunnel seems to cause less corneal endothelial cell loss.[14][15]
Retropupillary implantation seems to cause less corneal endothelial cell loss than AC iris fixated lens (antepupillary) implantation.[16][17][18][19]
Intraocular pressure (IOP) elevation.Reported incidence is about (0-7%)
IOP elevation can be a consequence of
- Iritis
- pupillary block
- pigment dispersion (iris chaffing)
Wound leak
as a consequence of a 5.5 mm corneal incision in eyes with previously incised cornea.[20]
Persistent ovalisation of the pupil
(reported in up to 13.9% of cases), especially in patients who underwent iris reconstruction and more frequently after retropupillary IOL implantation.[21] [22]
Dislocation
Dislocation of posterior-fixated iris-claw IOLs (0% to 10%), it is lower than the dislocation rate due to suture breakage in scleral-fixated PC IOL (between 7.8% and 27.9%)[23] [24] [25] [26] [27]
Cystoid macular edema (CME)
explanation of the macular oedema could be chronic low-grade irritation of the iris, this can be a result of: first, a lack of IOL stability causing movement of the IOL against the iris because insufficient iris tissue is captured in the claw or from iris progressive atrophy in the claw; secondly, microscopic imperfections in the surface of the IOL rubbing on the iris; and thirdly, malposition of the iris claw on the ciliary body. Another explanation for chronic, resistant cystoid macular oedema with iris-fixated IOLs is persistent vitreous traction after incomplete vitrectomy.[28]
Hyphema
Retinal detachment
Endophthalmitis
Retropupillary ARTISAN versus SFIOL*
| Retropupillary Artisan | Scleral fixation IOL | ||||
|---|---|---|---|---|---|
| Operation time | Shorter | Longer | |||
| Difficulty | Easier operation | More difficult | |||
| BCVA | No significant difference in final visual outcome | ||||
| Earlier visual rehabilitaion | Takes longer time | ||||
| Complications - general | |||||
| IOL dislocation | No significant difference | ||||
| CME | No significant difference | ||||
| Retinal detachment | No significant difference | ||||
| Complications - specific | |||||
| Iris atrophy | Suture erosion | ||||
| Pigment dispersion | IOL tilt and decentration | ||||
| Pupil distortion | |||||
| Endothelial cell loss | |||||
BCVA: best corrected visual acuity
CME: cystoid macular edema
IOL: intraocular lens
*Meta analysis [29]
Scleral fixation
Scleral fixated IOLs have gained increased popularity over the last decades but the history actually is dated back to 1980.
Scleral fixation of the IOL is indicated for secondary IOL implanation when there is no sufficient iris tissue or capsular bag to allow implantation of iris-fixation or sulcus IOL respectively but also it may be the preferred choice in patient with corneal decompensation or shallow AC even if there s an adequate iris tissue.
There are two ways to fixate an IOL to the sclera: suture-less and sutured fixation.
Scleral-sutured IOLs
Sutured fixation of the IOL can be either in an ab interno or ab externo approach. In the ab interno approach, the sutures are passed from inside to outside blindly, and this way can lead to retinal detachment, vitreous hemorrhage and improper haptic position. The ab externo approach is more reliable and sutures are passed from outside to inside the eye.
Sutures used are either 9-0 polypropylene, 7-0 Gore-tex (CV-8) or 6-0 prolene, and today the preferred IOL types are; CZ70BD (Alcon, Fort Worth, TX), enVista MX60 and the Akreos AO60 (Bausch and Lomb, Rochester, NY) which have eyelets for sutures.
The Bausch & Lomb Akreos AO60 hydrophilic acrylic lens with 4 eyelets is susceptible to calcification and opacification through calcium salt deposition when comes in contact with intraocular air or gas this makes it as an unpreferred choice for patients who may undergo posterior segment surgery while The Bausch & Lomb enVista Mx60 IOL with 2 eyelets is hydrophobic acrylic and does not opacify in contact with air or gas.
IOLs with 4 eyelets show more stability than the 2 eyelets IOLs in terms of less IOL tilt and decentration that may result in high order aberration uncorrectable by spectacles post-operatively and this was shown in several studies.
The first ab externo approach described by Lewis in 1991, used 10-0 polypropylene sutures and the sclerotomy sites are positioned 2 mm posterior to the limbus but several studies showed late suture breakage up to 8 years post-placement. For this reason, 9-0 polypropylene and Gore-tex sutures become more popular which show more suture stability on short term.
The sclerotomy sites are made 3 mm posterior to the limbus and these sites can be horizontal, vertical, or oblique, all are acceptable. It has been shown that with in-the-bag IOL calculation the postoperative myopic shift is more when sclerotomy sites are made 2 mm posterior to the limbus than when performed 3 mm posterior to the limbus.
Complications of sutured-fixated IOL include:
Suture knot erosion
Suture knot erosion carries the risk of endopthalmitis, therefore many attempts have been used to avoid this complication. Lewis introduced the creation of triangular scleral flap after conjunctival periotomy to cover the suture knots but this approach sacrifices the conjunctiva which presents a problem for patients who may undergo glaucoma surgery in the future. In 2005, Hoffman described the idea of creating scleral pockets without conjunctival periotomy with adequate coverage of the suture knots. Other ways described were the burying if the suture knots in the sclera which can be difficult in case of Gore-tex suture, and the avoidance of tying any knots by using the so called “Z- suture”. In this maneuver, the sutures are passed in zigzag fashion through the sclera and it was found that five passes are sufficient to secure the IOL.
IOL dislocation and tilt
Retinal detachment
Suprachoroidal or vitreous hemorrhage
Endophthalmitis
Hypotony
Ocular hypertension
CME
Sutureless SFIOLs
This technique is used to avoid suture related complications such as erosion or breakage. The first sutureless approach was introduced by Scharioth et al. who used 24-gauge needle to create 50% thickness scleral tunnels 1.5 -2 mm posterior to the limbus, then a 3-piece IOL was implanted and its haptics externalized through the scleral tunnels leaving a small exposed part of the haptics between the scleral tunnel and sclerotomy sites.
Later on, microvitreoretinal blade and 23-gauge trocar to form the scleral tunnels instead of using the 24-gauge needles. Abbey et al. described the same technique but without periotomy of the conjunctiva and used a 25-gauge trocar to create transconjunctival 3mm the scleral tunnels.
Agarwal and colleague in 2008 introduced the use of fibrin glue for securing the haptics of the IOL. In this approach, scleral flaps a are made and after the haptics are externalized, fibrin glue is applied to the bed of the scleral flap and the outer part of the flap is folded over the haptics securing the 3-piece haptics in place under the cover of the scleral flaps. Complications include, haptic extrusion, dislocation, breakage and subconjunctival haptics, most of them are caused by improper scleral tucking.
Agarwal also described the use of handshake technique for easier externalization of the haptics. In this technique, he used a MST forceps to catch the first (leading) haptic of the 3-piece IOL and this is externalized through the sclerotomy site. The second (trailing) haptic is then flexed inside the eye with one hand, at the same time, a MST forceps is introduced with the other hand through a side port and catches the tip of the second haptic. Then, the first hand is released and another forceps introduced through the sclerotomy site catches the second haptic and externalized.[30] [31]
In 2014, Yamane et al. developed a new adaptation of sutureless scleral fixation in which the haptics of the implanted 3-piece are externalized using a 27- gauge needle and cauterized to create bulbs at the end of the haptics to provide more stability in the scleral tunnels. In this technique, Yamane used EC-3 PAL 3- piece IOLs which has more durable and malleable haptics in comparison with the 3-piece IOLs used in United States.[32] [33]
What to choose the sutured-scleral fixation or the sutureless method ?
Till now, there is no study proved the superiority of one method over the other . Ganekal and colleagues compared sutured SFIOLs with fibrin-glue assisted SFIOLs and found that both groups have similar visual acuity but higher rates of complications were noticed in the sutured SFIOLs group like postoperative glaucoma and inflammation.
Another study compared the sutured SFIOLs ( using the Hoffman technique) with Scharioth SIS technique and also there was no significant difference in VA between the two groups but two cases of SIS group developed IOL dislocation while no one developed this complication in the first group.[34]
References
- ↑ Manoharan N, Prasad P. Secondary Intraocular Lens. InIntraocular Lens 2019 Nov 7. IntechOpen.
- ↑ Nihalani BR, Vanderveen DK. Secondary intraocular lens implantation after pediatric aphakia. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2011 Oct 1;15(5):435-40.
- ↑ Millar ER, Merchant K, Steel D. The Effect Of Anterior Capsulorhexis Optic Capture Of A Sulcus Fixated Iol Implant On Refractive Outcome. Investigative Ophthalmology & Visual Science. 2012 Mar 26;53(14):6646-.
- ↑ Gimbel HV, DeBroff BM. Intraocular lens optic capture. Journal of Cataract & Refractive Surgery. 2004 Jan 1;30(1):200-6.
- ↑ Kemp PS, Oetting TA. Stability and safety of MA50 intraocular lens placed in the sulcus. Eye (Lond) 2015;29:11:1438-41.
- ↑ Gerstmeyer K, Scholtz SK, Auffarth GU. [Sutured Posterior Chamber IOL Fixation in the Absence of Capsular Support, First Described in 1954]. Klin Monbl Augenheilkd. 2015 Aug;232(8):962-5. doi: 10.1055/s-0035-1545739. Epub 2015 May 6. Review. German. PubMed PMID: 25959008.
- ↑ Toro M, Longo A, Avitabile T, Nowomiejska K, Gagliano C, Tripodi S et al. Five-year follow-up of secondary iris-claw intraocular lens implantation for the treatment of aphakia: Anterior chamber versus retropupillary implantation. PLOS ONE. 2019;14(4):e0214140.
- ↑ Helvaci S,Demirduzen S, Oksuz H. Iris-claw intraocular lens implantation: anterior chamber versus retropupillary implantation. Indian J Ophthalmol. 2016; 64: 45–49. https://doi.org/10.4103/0301-4738. 178139 PMID: 26953023.
- ↑ Guell JL, Velasco F, Malecaze F, Va´zquez M, Gris O, Manero F. Secondary Artisan-Verysise aphakic lens implantation. J Cataract Refract Surg. 2005; 31: 2266–2271. https://doi.org/10.1016/j.jcrs.2005.06. 047 PMID: 16473216.
- ↑ Baykara M, Ozcetin H, Yilmaz S, Timuc¸in OB. Posterior iris fixation of the iris-claw intraocular lens implantation through a scleral tunnel incision. Am J Ophthalmol. 2007; 144: 586–591. https://doi.org/10. 1016/j.ajo.2007.06.009 PMID: 17692274.
- ↑ Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM, Bertelmann E, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012; 38: 2139–2143. https://doi.org/10.1016/j.jcrs.2012.07.035 PMID: 23036355.
- ↑ Gicquel JJ,Guigou S, Bejjani RA, Briat B, Ellies P, Dighiero P. Ultrasound biomicroscopy study of the Verisyseaphakic intraocular lens combined with penetrating keratoplasty in pseudophakic bullous keratopathy. J Cataract Refract Surg. 2007; 33: 455–464. https://doi.org/10.1016/j.jcrs.2006.11.017 PMID: 17321397.
- ↑ Teichman, J, Ahmed I. Improved Technique with the Artisan Aphakic IOL [Internet]. Reviewofophthalmology.com. 2020 [cited 25 March 2020]. Available from: https://www. reviewofophthalmology.com/article/improved-technique-with-the-artisan-aphakic-iol
- ↑ Jonker SMR, Berendschot TTJM, Ronden AE, Saelens IEY, Bauer NJC, Nuijts RMMA. Long-TermEndothelial Cell Loss in Patients with ArtisanMyopia and ArtisanToricPhakicIntraocularLenses: 5- and 10Year Results.Ophthalmology. 2018; 125: 486–494. https://doi.org/10.1016/j.ophtha.2017.08.011 PMID: 28935401.
- ↑ Güell JL, Velasco F, Malecaze F, Vázquez M, Gris O, Manero F. Secondary ArtisanVerysise aphakic lens implantation. J Cataract Refract Surg. 2005;31:2266–71.
- ↑ Wolter-Roessler M, Kuchle M. [Correction of aphakia with retroiridally fixated IOL]. Klin. Monbl. Augenheilkd. 2008;225:1041–4. doi: 10.1055/s-2008-1027721. [PubMed] [ CrossRef] [Google Scholar]
- ↑ Baykara M, Ozcetin H, Yilmaz S, Timucin OB. Posterior iris fixation of the iris-claw intraocular lens implantation through a scleral tunnel incision. AmJ Ophthalmol. 2007; 144:586–91. doi: 10.1016/j.ajo.2007.06.009. [PubMed] [CrossRef] [Google Scholar]
- ↑ Gicquel JJ, Guigou S, Bejjani RA, Briat B, Ellies P, Dighiero P. Ultrasound biomicroscopy study of the Verisyse aphakic intraocular lens combined with penetrating keratoplasty in pseudophakic bullous keratopathy. J Cataract Refract Surg. 2007;33:455–64. doi: 10.1016/j.jcrs.2006.11.017. [PubMed] [CrossRef] [Google Scholar]
- ↑ Dighiero P, Guigou S, Mercie M, Briat B, Ellies P, Gicquel JJ. Penetrating keratoplasty combined with posterior Artisan iris-fixated intraocular lens implantation. Acta Ophthalmol Scand. 2006;84:197–200. doi: 10.1111/j.1600-0420.2005.00573.x. [PubMed] [CrossRef] [ Google Scholar]
- ↑ De Silva SR, Arun K, Anandan M, Glover N, Patel CK, Rosen P. Iris-claw intraocular lenses to correct aphakia in the absence of capsule support. J Cataract Refract Surg. 2011; 37: 1667–1672. https://doi.org/10.1016/j.jcrs.2011.03.051 PMID: 21855764.
- ↑ Helvaci S, Demirduzen S, Oksuz H. Iris-claw intraocular lens implantation: anterior chamber versus retropupillary implantation. Indian J Ophthalmol. 2016; 64: 45–49. https://doi.org/10.4103/0301-4738. 178139 PMID: 26953023.
- ↑ Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM, Bertelmann E, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012; 38: 2139–2143. https://doi.org/10.1016/j.jcrs.2012.07.035 PMID: 23036355.
- ↑ Bading G, Hillenkamp J, Sachs HG, Gabel VP, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007; 144: 371–377. https://doi.org/10.1016/j.ajo.2007.05.014 PMID: 17624290.
- ↑ Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long- term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006; 141: 308–312. https://doi.org/10.1016/j.ajo.2005.09.012 PMID: 16458685.
- ↑ Rufer F, Saeger M, No¨ lle B, Roider J. Implantation of retropupillar iris claw lenses with and without combined penetrating keratoplasty. Graefes Arch ClinExpOphthalmol. 2009; 247: 457–462.
- ↑ Wolter-Roessler M, Ku¨chle M. Correction of aphakia with retroiridally fixated IOL. KlinMonatsblAugenheilkd. 2008; 225: 1041–1044.
- ↑ Mohr A, Hengerer F, Eckardt C. Retropupillary fixation of the iris claw lens in aphakia; 1 year outcome of a new implantation technique. Ophthalmologe. 2002; 99: 580–583. PMID: 12148307.
- ↑ Massa H, Gobej I, Jacquier P, Jonescu-Cuypers C, Le Quoy O. Cystoid macular oedema and iris-fixated intraocular lens treated with intraocular lens exchange: A case series and review. Journal of International Medical Research. 2018;47(1):188-195.
- ↑ Jing W, Guanlu L, Qianyin Z, Shuyi L, Fengying H, Jian L et al. Iris-Claw Intraocular Lens and Scleral-Fixated Posterior Chamber Intraocular Lens Implantations in Correcting Aphakia: A Meta-Analysis. Investigative Opthalmology & Visual Science. 2017;58(9):3530.
- ↑ Narang P, Agarwal A. The “correct shake” for “handshake” in glued intrascleral fixation of intraocular lens. Indian journal of ophthalmology. 2016 Nov;64(11):854.
- ↑ Agarwal A, Jacob S, Kumar DA, Agarwal A, Narasimhan S, Agarwal A. Handshake technique for glued intrascleral haptic fixation of a posterior chamber intraocular lens. Journal of Cataract & Refractive Surgery. 2013 Mar 1;39(3):317-22.
- ↑ Manoharan N, Prasad P. Secondary Intraocular Lens. InIntraocular Lens 2019 Nov 7. IntechOpen.
- ↑ Stem MS, Todorich B, Woodward MA, Hsu J, Wolfe JD. Scleral-fixated intraocular lenses: past and present. Journal of vitreoretinal diseases. 2017 Mar;1(2):144-52.
- ↑ Stem MS, Todorich B, Woodward MA, Hsu J, Wolfe JD. Scleral-fixated intraocular lenses: past and present. Journal of vitreoretinal diseases. 2017 Mar;1(2):144-52.