Lipemia Retinalis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Lipemia Retinalis is a rare manifestation of hypertriglyceridemia manifested by abnormal appearance of the retinal arteries and veins, and occasionally the entire fundus.
Disease
Lipemia Retinalis, is caused by hypertriglyceridemia with serum triglyceride levels typically greater than 1000 mg/dl. Multiple genes responsible for triglyceride metabolism have been identified as causing the serum triglyceride levels to see characteristic retinal vasculature abnormalities. Based on the National Health and Nutrition Examination Survey from 2001 and 2006, approximately 1.7% of the total US population, or 3.4 million Americans, were estimated to have severe hypertriglyceridemia (500 to 2,000 mg/dl). Individuals with severe hypertriglyceridemia tended to be men (75.3%), non-Hispanic whites (70.1%), and aged 40-59 years (58.5%). Diabetes and hypertension was associated in 14% and 31.3% of cases respectively. [1]
Etiology
Lipemia retinalis is commonly associated with high triglyceride levels in hyperlipoproteinemias types 1, 3, 4, and 5 with different underlying causes, [2] and chromosome microarray and lipid gene sequencing may demonstrate a homozygous lipoprotein lipase gene coding mutation. However, genotype–phenotype correlations have not been established, as there is no established association between the nature or location of the mutation, age at diagnosis, lipid levels, and severity of symptoms. [3]
Risk Factors
Lipemia retinalis is an ocular finding associated with elevated plasma levels of triglycerides. It serves as a vital clinical sign of hypertriglyceridemia because acute triglyceride elevations may be asymptomatic at first, delaying treatment of a potentially lethal metabolic disorder as elevations of this magnitude may lead to cardiovascular consequences including heart attack or stroke. [4]
General Pathology
The ocular findings result from light scatter induced by the triglyceride-laden chylomicrons in the plasma. [5] Hyperlipidemia without accompanying hypertriglyceridemia does not present this clinical picture. [4]
Pathophysiology
The early signs of lipemia retinalis occur in the peripheral retina, and as triglyceride levels increase, they spread to the posterior pole. At triglyceride levels of 2500–3499 mg/dL, the peripheral vessels appear creamy and thin; at levels of 3500–5000 mg/dL, the vessels in the posterior pole assume a creamy color; and at levels exceeding 5000 mg/dL, the fundus becomes salmon-colored, with creamy arteries and veins that can be distinguished by caliber only. The clinical appearance is graded accordingly as early, moderate, or marked (Stages I-III, respectively).
Primary Prevention
Reduction and control of serum triglyceride levels will prevent lipemia retinalis from developing. Correction of the lipid levels may reverse the abnormal findings within one week. Strict adherence to a low-fat diet without breast milk supplementation may be effective in treating infants with severe lipemia retinalis associated with very high serum triglyceride levels. [6]
Diagnosis
Lipemia retinalis is diagnosed based upon its clinical appearance on dilated fundoscopic exam and coexistent hypertriglyceridemia.
History
There may be a family history of lipid abnormalities. Hypertriglyceridemia occurs as a primary familial disorder or secondary to other diseases. The familial disorders include ApoC-II deficiency, endogenous circulating LPL inhibitor, and LPL deficiency. [7]
Physical Examination
The physical exam on a patient with lipemia retinalis includes vital signs, cardiovascular exam, integumentary exam and dilated fundoscopy. Vital signs should focus on atherosclerotic changes. The cardiovascular exam should include heart sounds, carotid or renal bruits, and peripheral pulses. Skin exam should look for eruptive xanthomas. Ocular exam may reveal corneal arcus and dilated fundoscopic exam is necessary for the diagnosis and staging of lipemia retinalis.
Signs
Signs of lipemia retinalis include peripheral vessels that appear creamy and thin; later in the disease, the vessels in the posterior pole assume a creamy color; and in the most advanced stage, the fundus becomes salmon-colored, with creamy arteries and veins.
Symptoms
Lipemia retinalis is typically asymptomatic and generally does not affect visual acuity unless it is associated with vascular occlusion and/ or retinal ischemia. The diagnosis of lipemia retinalis is made based on ophthalmoscopic examination demonstrating the appearance of pink to milky white retinal veins and arteries. Chronic hypertriglyceridemia may cause patients to complain of recurrent abdominal pain in the setting of recurrent or acute pancreatitis. [4] Markedly elevated triglycerides in lipemia retinalis might predispose patients to develop potential ocular complications including loss of vision caused by inner retinal ischemia or the development of retina vein occlusion.[5]
Clinical diagnosis
Lipemia retinalis generally does not affect visual acuity unless it is associated with vascular occlusion and/ or retinal ischemia. The diagnosis of lipemia retinalis is made based on clinical examination demonstrating the appearance of pink to milky white retinal veins and arteries.
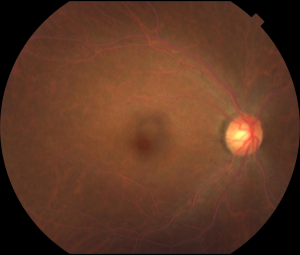
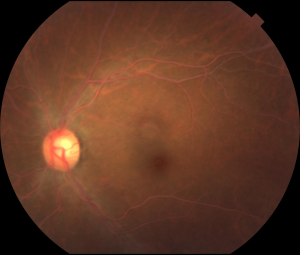
Case Report
Figures: Right and left eyes of a 43-year-old asymptomatic woman who was referred by an optometrist for abnormal-appearing blood vessels. Visual acuity and examination were normal except for the retinal vessels seen on dilated exam. Note the creamy ‘cake batter’ appearance of the retinal arteries and veins bilaterally. Subsequent serum lab testing revealed an elevated total cholesterol with a triglyceride level >3500 mg/ dl. She was started on oral fenofibrate and niacin which normalized her triglyceride level within 6 weeks. Subsequent dilated exam at that time by the referring optometrist showed a normal fundus appearance (photo unavailable). Photo courtesy of Daniel F. Kiernan, MD, FACS and Barbara McGinley, CRA, COT.
Diagnostic procedures
Fluorescein and indocyanine angiography testing is typically unremarkable. Spectral-domain optical coherence tomography is useful in demonstrating inner retinal changes associated with lipemia retinalis at the histopathological level. Testing may demonstrate hyperreflective and engorged retinal vessels and white dots in the inner nuclear and ganglion cell layer which may slowly dissipate over several months after serum triglyceride levels are normalized. This is notably more gradual than the gross appearance of the retinal blood vessel appearance which typically normalizes within 5 days after lipid levels are lowered. A case report described the hyperreflective appearance of the retinal vessels in OCT reversing five days after the treatment, whereas the hyperreflective dots seen on OCT disappeared over 3 months.[8] OCT-angiography findings have not yet been reported. Testing with electroretinography may show decreased a- and b-wave amplitudes in both cone and rod responses. [9]
Laboratory test
A fasting lipid profile as a general medical examination should be sought in a patient found to have lipemia retinalis. Hypertriglyceridemia occurs as a primary familial disorder or secondary to other diseases. The familial disorders include ApoC-II deficiency, endogenous circulating LPL inhibitor, and LPL deficiency. [7]
Differential diagnosis
The differential for lipemia retinalis includes branch retinal artery or vein occlusion, hypertensive retinopathy, and diffuse choroidal hemangioma (the salmon fundus seen in late stage lipemia retinalis cases may resemble the tomato catsup fundus seen in patients with diffuse hemangioma).
Management
Treatment is necessary for the systemic effects of hypertriglyceridemia, although no treatment is required for the lipemia retinalis itself. The treatment for lipemia retinalis is primarily is directed at reducing serum triglyceride (and therefore serum cholesterol) levels.
General treatment
Lipemia retinalis is an important ocular sign of a life-threatening but easily treatable metabolic disorder. Therefore, the treatment is to reduce the serum triglyceride levels to below 500 mg/dl. This can be accomplished by a number of medical treatments for lowering triglyceride and cholesterol. The patient should be followed by his primary medical doctor to treat the hyperlipidemia.
Medical therapy
Three classes of medications are appropriate for the management of major triglyceride elevations: fibric acid derivatives, niacin, and omega-3 fatty acids. High doses of a strong statin (simvastatin, atorvastatin, rosuvastatin) also lower triglycerides, by as much as approximately 50%. Four fibrates are used in clinical practice: gemfibrozil and fenofibrate are available in the United States; bezafibrate and ciprofibrate are available in Europe and other countries. [10]
Medical follow up
Once triglyceride levels return to normal, the clinical ocular findings of lipemia retinalis should quickly resolve. [4]
Surgery
Surgery is not specifically indicated for the treatment of lipemia retinalis. However, plasmapheresis can be used in the setting of severe hypertriglyceridemia to reduce triglycerides in the acute setting. Ileal bypass surgery has demonstrated improvement in all lipid parameters but should be reserved for refractory cases. [11] Lipemia retinalis has been reported in association with hypercholesterolemia, skin xanthelasmas and a pulmonary cholesteroloma lung lesion as complications following allogeneic bone marrow transplant for treatment of diffuse mixed T cell lymphoma in a 22-year-old woman. These complications resolved and cholesterol levels following plasmapheresis and hypolipidemic treatment with a statin. [12]
Surgical follow up
After plasmapheresis therapy, delayed transfusion reactions or infection related to the use of central venous catheter can occur days after the treatment, and patients should seek medical attention if signs and symptoms occur.[13]
Complications
The elevated serum lipid levels associated with lipemia retinalis predisposes patients to many other systemic vascular pathologies including cardiovascular accidents and acute myocardial infarction. Retinal vascular diseases may also occur including retinal artery and vein occlusions. Ischemia secondary to vascular occlusions can lead to neovascularization and vitreous hemorrhage.
Prognosis
Patients with lipemia retinalis are at increased systemic risk for coronary artery disease, myocardial infarction and stroke and increased ophthalmic risk for retinal artery and vein occlusions and retinal ischemia. Retinal changes secondary to lipemia retinalis will improve once serum triglyceride levels are normalized.
Additional Resources
- https://www.medscape.org/viewarticle/585045_2
- https://www.ncbi.nlm.nih.gov/pubmed/?term=lipemia+retinalis
- https://www.nejm.org/doi/full/10.1056/NEJMicm040437
References
- ↑ Christian JB, Bourgeois N, Snipes R, Lowe KA. Prevalence of severe (500 to 2,000 mg/dl) hypertriglyceridemia in United States adults. Am J Cardiol. 2011 Mar 15;107(6):891-7.
- ↑ Thomas PK, Smith EB. Ocular manifestations in idiopathic hyperlipaemia and xanthomatosis. Br J Ophthalmol. 1958;42(8):501–506.
- ↑ Mailly F, Palmen J, Muller DP, et al. Familial lipoprotein lipase (LPL) deficiency: a catalogue of LPL gene mutations identified in 20 patients from the UK, Sweden, and Italy. Hum Mutat. 1997;10(6):465–473.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Horton M, Thompson K. Lipemia retinalis preceding acute pancreatitis. Optometry 2011;82:475-80.
- ↑ Jump up to: 5.0 5.1 Nagra PK, Ho AC, Dugan JD Jr. Lipemia retinalis associated with branch retinal vein occlusion. Am J Ophthalmol 2003;135:539-42.
- ↑ Yin HY, Warman R, Suh EH, Cheng AM. Exceptionally elevated triglyceride in severe lipemia retinalis. Int Med Case Rep J. 2016 Oct 21;9:333-336.
- ↑ Jump up to: 7.0 7.1 Rahalkar AR, Giffen F, Har B, et al. Novel LPL mutations associated with lipoprotein lipase deficiency: Two case reports and a literature review. Can J Physiol Pharmacol 2009;87:151-60.
- ↑ Özturk BT, Bozkurt B, Meşen A, et al. Spectral-Domain Optical Coherence Tomography Findings in Lipemia Retinalis. Ophthalmic Surg Lasers Imaging Retina. 2016 1;47.
- ↑ Lu CK, Chen SJ, Niu DM, et al. Electrophysiological changes in lipaemia retinalis. Am J Ophthalmol 2005;139:1142-5.
- ↑ Maki KC, Bays HE, Dicklin MR. Treatment options for the management of hypertriglyceridemia: strategies based on the best-available evidence. J Clin Lipidol. 2012 Sep-Oct. 6(5):413-26.
- ↑ Schaap-Fogler M, Schurr D, Schaap T, et al. Long-term plasma exchange for severe refractory hypertriglyceridemia: a decade of experience demonstrates safety and efficacy. J Clin Apher. 2009. 24(6):254-8.
- ↑ Toren A, Nagler A. Solitary pulmonary cholesteroloma, multiple xanthelasmas and lipemia retinalis complicating hypercholesterolemia after bone marrow transplantation. Bone Marrow Transplant. 1996 Aug;18(2):457-9.
- ↑ Chang CT, Tsai TY, Liao HY, et al. Double Filtration Plasma Apheresis Shortens Hospital Admission Duration of Patients With Severe Hypertriglyceridemia-Associated Acute Pancreatitis. Pancreas. 2016 Apr. 45 (4):606-12.