Xanthelasma
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity

Xanthelasma Palpebrarum (XP) is a benign condition involving cutaneous lesions in the periocular region.[2] It presents as a xanthoma found on the medial aspect of the eyelids.[3] These lesions are do not typically present with functional limitations.[1] It occurs more commonly in women (1.2% incidence rate) than in men (0.3% incidence rate) with a peak incidence at the ages of 30-50 years old. [3] [1] [4]
Disease
Nearly half of patients with xanthelasma have associated lipid disorders. These include Type II hyperlipidemia, Type IV hyperlipidemia, high total cholesterol, high triglycerides, and low levels of high density lipoprotein (HDL).[3][5] However, despite the strong association of XP with lipid imbalance, 25-70% of patients are normolipidemic on presentation.[6]
Risk Factors
- Diabetes Mellitus
- Hypothyroidism
- Cardiovascular disease
- Obesity
- Pancreatitis
- hyperuricemia
- Smokers
- Excessive alcohol intake here
Pathophysiology
This is currently unclear, one possible etiology results from increased plasma peroxidation of low density lipoprotein (LDL) resulting in cholesterol accumulating within macrophages to form foam cells.[7] In xanthoma formation, the ability to remove cholesterol from the tissue is reduced due to low HDL levels. Additionally, the rate by which LDL leaks from the capillaries is increased in areas that endure friction and constant motion which may indicate the reason the eyelid skin is most commonly affected. An increase in inflammatory cells within the eyelid tissue is also thought to have an effect on the formation of xanthelasma.[6]
Diagnosis
XP lesions present as soft, yellow papules or plaques filles with cholesterol at the medial canthus of the eyelids. They can appear as multiple, symmetric lesions that more commonly are found on the upper eyelid than the lower one [4][5]. Patients will seek professional treatment for xanthelasma due to cosmetic concerns, additionally these lesions tend to be permanent and can grow in size with time which may be distressing [5]. From a provider standpoint, the diagnosis can be made clinically.
Biopsy:
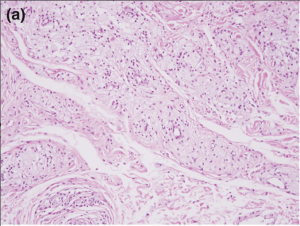
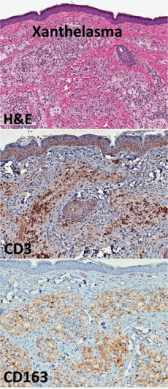
Reticular dermis infiltration of foamy macrophages with sparing of the epidermis, papillary dermis, and subcutaneous fatty layer. The inflammatory infiltrate in the superficial reticular dermis will be perivascular and consist of foam cells with lipid-laden cytoplasmic vacuoles [5]. Foam cells, or xanthoma cells, originate from macrophages that have accumulate intracellular cholesterol, lipids, and fat [7][8].
Laboratory test
- HbA1C
- Liver panel
- Thyroid function tests
- Lipid panel
Differential diagnosis
In patients presenting with XP, a differential diagnosis must take into account other conditions that can present with xanthelasma or lesions that appear very closely to xanthelasma.
A chronic granulomatous disorder in which 80-85% of patients present with yellowish lesions in the periorbital region that can appear very similarly to XP [8].
Syringoma:
A benign eccrine tumor that presents as a papule in the periocular area of middle-aged women [9].
A form of non-Langerhans cell histiocytosis in which xanthelasmas are present in about 30% of patients [10]. In patients with adult-onset asthma with periocular xanthogranuloma (AAPOX), patients have periocular infiltrates made up of foamy histiocytes like those seen in xanthelasma [11] [12].
Treatment
Conservative therapy begins with a low-fat diet and statins- the therapeutic effect is questionable.[5] Popular treatment options include surgical excision, laser therapy, chemical peel, cryotherapy, and radiofrequency ablation [2] [1].
Surgical excision of the xanthelasma was one of the earliest treatments, however post-operative adverse outcomes must be considered. Risk of cicatricial ectropion, transient hematomas, poor cosmetic outcome, recurrence, and infection are possible [1]. Thickness of these lesions are difficult to measure which may necessitate the need for grafts at the time of surgery.
Trichloroacetic acid (TCA) is commonly used for the peel at a 70% concentration. The peel induces a chemical cauterization causing coagulation of proteins within the skin- this is then neutralized within the superficial dermal plexus. The formation of salts results in the serum turning a white color. TCA is most effective on small lesions but adverse effects can be related to the depth of skin penetration [4]. Risks include atrophy, scar formation, and discoloration of the affected skin [1].
Laser therapy utilizes energy to coagulate vessels and damage the perivascular foam cells that make up the lesion. Fractionated Er:YAG and fractionated CO2 lasers are the most commonly used but other options include erbium, pulsed dye, and argon [5]. Complications of laser therapy include erythema, hypo- and hyperpigmentation, scar formation, infection, severe burn, ectropion, corneal injury, ocular perforation, and a 13-16% recurrence rate.[2] [1]
Cryotherapy causes vasoconstriction and the formation of microthrombi as a result of cell death within XP lesions. Edema, scar formation, skin discoloration, vesicle formation, and blister formation are potential adverse effects. Due to the risk of extreme swelling in the eyelid, cryotherapy is usually avoided.15
Radiofrequency treatment works by causing electrocoagulation for instant hemostasis and is used in vascular lesions. This treatment option can be used for lesions that are very close to the globe or that have indistinct borders. The main complication is hypo- and hyperpigmentation of the skin and price limits its use [1] [5].
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Dincer D, Koc E, Erbil AH, Kose O. Effectiveness of low-voltage radiofrequency in the treatment of xanthelasma palpebrarum: a pilot study of 15 cases. Dermatol Surg. Dec 2010;36(12):1973-8. doi:10.1111/j.1524-4725.2010.01770.x
- ↑ Jump up to: 2.0 2.1 2.2 Esmat SM, Elramly AZ, Abdel Halim DM, Gawdat HI, Taha HI. Fractional CO2 laser is an effective therapeutic modality for xanthelasma palpebrarum: a randomized clinical trial. Dermatol Surg. Dec 2014;40(12):1349-55. doi:10.1097/DSS.0000000000000172
- ↑ Jump up to: 3.0 3.1 3.2 Aggarwal R, Rathore PK. A study evaluating xanthelasma palpebrarum clinically and biochemically. International Journal of Contemporary Medical Research. 2016;3(9):2565-7.
- ↑ Jump up to: 4.0 4.1 4.2 Nahas TR, Marques JC, Nicoletti A, Cunha M, Nishiwaki-Dantas MC, Filho JV. Treatment of eyelid xanthelasma with 70% trichloroacetic acid. Ophthalmic Plast Reconstr Surg. Jul-Aug 2009;25(4):280-3. doi:10.1097/IOP.0b013e3181aa9a1f
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Al Aboud AM, Al Aboud DM. Xanthelasma Palpebrarum. StatPearls. 2021.
- ↑ Jump up to: 6.0 6.1 6.2 Govorkova MS, Milman T, Ying GS, Pan W, Silkiss RZ. Inflammatory Mediators in Xanthelasma Palpebrarum: Histopathologic and Immunohistochemical Study. Ophthalmic Plast Reconstr Surg. May/Jun 2018;34(3):225-230. doi:10.1097/iop.0000000000000921
- ↑ Jump up to: 7.0 7.1 Abdelkader M, Alashry SE. Argon laser versus erbium:YAG laser in the treatment of xanthelasma palpebrarum. Saudi J Ophthalmol. Apr-Jun 2015;29(2):116-20. doi:10.1016/j.sjopt.2014.09.017
- ↑ Jump up to: 8.0 8.1 Wood AJ, Wagner MVU, Abbott JJ, Gibson LE. Necrobiotic Xanthogranuloma: A Review of 17 Cases With Emphasis on Clinical and Pathologic Correlation. Archives of Dermatology. 2009;145(3):279-284. doi:10.1001/archdermatol.2008.583
- ↑ Lim Y, Lee J, Jang D, Abudureyimu G, Lee JH. Clinical characteristics and pathological depths of syringomas in 94 Korean patients. Skin Res Technol. Jan 2021;27(1):70-73. doi:10.1111/srt.12910
- ↑ Campochiaro C, Tomelleri A, Cavalli G, Berti A, Dagna L. Erdheim-Chester disease. Eur J Intern Med. May 2015;26(4):223-9. doi:10.1016/j.ejim.2015.03.004
- ↑ Rajput R, Mathewson P, Mudhar HS, Hiley P, Sandramouli S, Bhatt R. Periocular cutaneous sarcoid: case series and review of the literature. Eye (Lond). Oct 2019;33(10):1590-1595. doi:10.1038/s41433-019-0448-5
- ↑ Baykal C, Polat Ekinci A, Yazganoglu KD, Buyukbabani N. The clinical spectrum of xanthomatous lesions of the eyelids. Article. International Journal of Dermatology. 10// 2017;56(10):981-992. doi:10.1111/ijd.13637