Small Incision Lenticule Extraction (SMILE)
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Surgical Therapy
Small incision lenticule extraction (SMILE) is a relatively new refractive procedure designed to treat a multitude of refractive errors such as myopia, hyperopia, presbyopia, and astigmatism. The procedure involves using a femtosecond laser to create a corneal lenticule, which is extracted whole through a small incision without the use of an excimer laser. It is reported to achieve effects similar to laser-assisted in situ keratomileusis (LASIK) with excellent postoperative outcomes.
Background/Overview
Starting in 2007, an intrastromal lenticule method was reintroduced as an alternative to LASIK called Femtosecond Lenticule Extraction (FLEx) intended for patients with extreme myopia. After improvements to scan modes and energy parameters, improved visual recovery times were noted, with refractive results similar to LASIK. Following the implementation of FLEx, a procedure called small incision lenticule extraction (SMILE) was developed, involving a small 2-3 mm incision used to allow for extraction of the whole corneal lenticule without the need to create a flap.[1]
SMILE is noted for achieving similar effects as LASIK but with some possible benefits such as faster recovery of post-op dry eye, reinnervation of corneal nerves, and a potential biomechanical advantage. The commencement of this procedure began in September 2011 and is established in various locations such as Europe, China and India. Approval from the FDA in the United States was received in 2016 for spherical myopic corrections; approval for compound myopic astigmatism followed in October 2018.[2]
SMILE is also considered more cost effective to LASIK, because it requires one laser platform as compared the two required by LASIK.
Surgical Candidates
SMILE is approved in the US by the Food and Drug Administration for the treatment of myopia from -1D to -8D and astigmatism up to -0.5 D, with a manifest refraction spherical equivalent (MRSE) of less than or equal to -8.25 D in patients aged 22 years or older.
Contraindications to surgery are similar to those of LASIK. Absolute contraindications include corneal ectasia, exposure keratopathy, unstable refractive error, pregnant or breastfeeding, severe ocular surface/tear film disorders, uncontrolled glaucoma or uveitis, and one-eyed patients. Relative contraindications include age under 22 years, mild ocular surface/tear film disorders, corneal dystrophies, controlled diabetes, past ocular herpes infection, systemic immunodeficiencies, and autoimmune deficiencies.
Compared to LASIK, SMILE is preferable for patients with preexisting dry eye, patients with higher refractive error, athletes in contact sports, and patients with larger pupils.[3]
Surgical Technique & History of Procedure
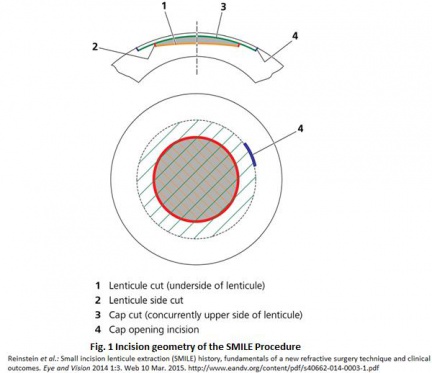
During the SMILE procedure, the patient is raised to the contact glass of the femtosecond laser and suction ports are activated to keep the patient's eye fixated in the correct position while the lenticule is created. The lower interface of the intrastromal lenticule is created first (using an out-to-in direction with the laser to maximize the time without blurring the patient’s central vision), followed by the upper interface of the lenticule (using an in-to-out direction), known as the cap, and finally a 2–3 mm tunnel incision (usually supero-temporal) that links the cap interface to the corneal surface. To avoid any undesirable effects in the cornea such as haziness, the two interfaces (lower and upper) are created from the endothelial side of the cornea to the epithelial side. The patient is then moved to the surgical microscope for the lenticule separation and extraction part of the procedure. The layers of the lenticule are outlined and the lenticule is removed from the cornea using a pair of retinal micro-forceps, or can be extracted directly from within the pocket with the latest versions of the lenticule stripper, one of many instruments being developed for the SMILE procedure specifically.[4]
When planning the treatment, the following parameters can be selected by the surgeon: cap thickness, cap diameter, cap sidecut angle, refractive correction, lenticule diameter (optical zone), lenticule sidecut angle, and the minimum lenticule thickness (so that the lower lenticule interface can be easily differentiated from the upper interface).
Outcomes
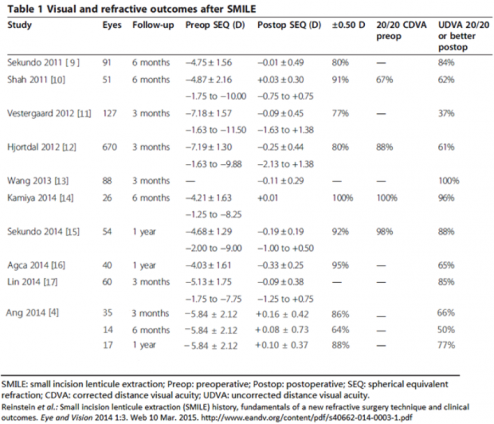
A meta-analysis of randomized controlled trials and comparative studies comparing SMILE and FS-LASIK by Zhang et al found no significant difference between them except corneal sensation and tear break-up time, which favored SMILE. Refractive spherical equivalent (P = .72), eyes losing 2 or more lines of corrected vision after surgery (P = .69), eyes obtaining 20/20 uncorrected distance visual acuity (P = .35), and eyes falling within +/- 1.00 diopters of target spherical equivalent (P = .70) were similar in the two groups.[5] SMILE was found to be superior to LASIK and comparable to PRK in preserving corneal biomechanical properties of corneal hysteresis and corneal resistance factor after surgery.[6] One prospective randomized controlled trial between wavefront-guided (WFG) LASIK and SMILE showed that WFG LASIK was superior in achieving better low-contrast visual acuity, and better uncorrected visual acuity.[7] It has also been compared to PRK (another flapless refractive procedure) and was shown to have similar objective and subjective visual outcomes[8].
A recent focus of study has been on the corneal biomechanical outcomes of SMILE, as the factors contributing to its long-term impact on corneal biomechanics are incompletely understood. A prospective non-randomized controlled trial involving 45 eyes treated with LASIK and 45 eyes treated with SMILE compared biomechanical parameters at 6 months and found similar results between the two groups[9]. One review paper found that while both LASIK and SMILE results in weakened corneal biomechanical stability postoperatively, there is mixed evidence on whether SMILE or LASIK may be preferable for high myopes versus low myopes in this regard.[10]
Lenticule cap thickness has also been proposed to affect these parameters, as one study involving 146 eyes suggested corneas were stiffer postoperatively when a 130 um cap was used when compared to 110um and 120um caps[11]. A third study involving 80 eyes noted decreased height of the central posterior corneal surface and increased height of the peripheral posterior corneal surface at 3 year follow up in SMILE patients. These changes were not seen when a limited ablation ratio was used[12]. More studies are likely to further elucidate how various technical parameters and surgical techniques impact long-term corneal stability.
Complications
Complications arising during the SMILE procedure have been reported very infrequently, supporting the reported safety and predictability of the procedure. Studies using SMILE found epithelial abrasions, small tears at the incision, and perforated caps in a few cases. However, none of these patients had late visual symptoms.[13] The loss of suction during the femtosecond laser portion of the procedure is one of the primary complications with SMILE since it requires longer duration than a LASIK flap. While noted to be very infrequent, one study showed that the majority of cases in which suction loss occurred were able to be reapplied in the same sitting (81.8%). [14] The rest of the suction loss cases were aborted, though it should be noted that for all cases involving suction-loss, there remained a significant number of patients that attained UDVA within attempted correction.
A review article found the following incidences for postoperative complications: epithelial defects (3.3% compared to 4.9% for LASIK); epithelial ingrowth (0.016%-0.5%); microstriae (0.14%). The lower rate of epithelial complications in comparison to LASIK are attributable to the abscence of flap creation and mechanical scraping in SMILE. [24]
Because a small incision (2-3 mm) is used in place of an entire flap, corneal nerve severance is minimal in comparison to LASIK. This coincides with the decreased occurrence of post-operative dry eye and studies have indeed shown an increase in nerve reinnervation after treatment. In a study by Xu et al. comparing dry eye parameters between SMILE and LASIK, all parameters were found to be worse in the early postoperative period for both groups, however the SMILE group showed better scores in tear break up time, the McMonnies score, and Schirmer’s test.[25] These findings by Xu et al. coincide with similar results from a study by Denoyer et al. [26]which found high rates of dry eye symptoms for both procedures reported one month after surgery, but at 6 months after surgery, 80% of SMILE patients finished using any eye drops in contrast to only 57% of the patients in the LASIK group. An additional study that followed 80 eyes over 12 months in which the patients had one eye treated with LASIK and the fellow eye treated with SMILE noted gradual improvement of visual symptoms over time (glare, halos, etc) in both eyes after both procedures[27].
Ectasia risk, while thought to be low even in high risk eyes,[28][29] is still possible with SMILE, with incidence noted to be around 0.15%.[30] [31][32][33][34] The majority of the reported cases involved patients noted to be borderline or high risk for LASIK, highlighting that the risk of ectasia, while lower, persists even with SMILE. Similarly, other interface-related complications, including diffuse lamellar keratitis (DLK), corneal haze, interface infections,[35] pressure-induced stromal keratitis (PISK),[36] interface fluid syndrome,[37] and epithelial ingrowth[38][39][40] have been reported.
Conclusions
The SMILE procedure seems to be a promising alternative to LASIK in some cases. Given its flapless technique and results that appear to be similar to LASIK, it may offer the same correctional abilities with the potential benefits of faster recovery of post-op dry eye, quicker reinnervation of corneal nerves, and biomechanical advantages. This procedure may be an upcoming option for more patients undergoing refractive surgery, due to its minimally invasive technique and promising outcomes.
Additional Resources
- Turbert D, Huffman JM. Small Incision Lenticule Extraction (SMILE). American Academy of Ophthalmology. EyeSmart/Eye health. https://www.aao.org/eye-health/treatments/small-incision-lenticule-extraction-smile. Accessed July 2, 2024.
References
- ↑ Reinstein et al.: Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye and Vision 2014 1:3. Web 10 Mar. 2015. http://www.eandv.org/content/pdf/s40662-014-0003-1.pdflink=[1]link=
- ↑ "ZEISS Receives FDA Approval for ReLEx SMILE Expanding Myopia Treatment to Patients with Astigmatism." Innovative SMILE Procedure from ZEISS. ZEISS, 05 Oct. 2018. Web. 06 Feb. 2020. https://www.zeiss.com/meditec/int/news/2018/fda-approval-for-smile-astigmatism.html
- ↑ Titiyal JS, Kaur M, Shaikh F, Gagrani M, Brar AS, Rathi A. Small incision lenticule extraction (SMILE) techniques: patient selection and perspectives. Clin Ophthalmol. 2018 Sep 5;12:1685-1699. doi: 10.2147/OPTH.S157172. PMID: 30233132; PMCID: PMC6134409.
- ↑ Liu Y-C, Pujara T, Mehta JS (2014) New Instruments for Lenticule Extraction in Small Incision Lenticule Extraction (SMILE). PLoS ONE 9(12): e113774. doi:10.1371/journal.pone.0113774
- ↑ Zhang "et al.:" Clinical Outcomes of SMILE and FS-LASIK Used to Treat Myopia: A Meta-analysis. J Refractive Surg, Vol 32, No. 4. 2016.
- ↑ Guo H, Hosseini-Moghaddam SM, Hodge W. Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis. BMC Ophthalmol 2019;19:167
- ↑ Chiang B, Valerio GS, Manche EE. Prospective, Randomized Contralateral Eye Comparison of Wavefront-Guided Laser In Situ Keratomileusis and Small Incision Lenticule Extraction Refractive Surgeries. Am J Ophthalmol. 2022
- ↑ Zhang, R., Zhang, Y., Yuan, Y. et al. Comparison of objective and subjective visual quality after flapless laser vision correction for mild to moderate myopia: SMILE vs PRK. Graefes Arch Clin Exp Ophthalmol (2023). https://doi.org/10.1007/s00417-022-05937-7
- ↑ Liu, Mingna MD*,†,‡; Li, Na MD*,†,‡; Chen, Tong MD*,†,‡; Tian, Ge MD*,†,‡; Lin, Yue MD*,†,‡; Gao, Hua MD, PhD*,†,‡; Shi, Weiyun MD, PhD*,†,‡. Comparison of Corneal Biomechanics Treated With Femtosecond Laser-Assisted in situ Keratomileusis and Small-Incision Lenticule Extraction by New Corneal Biomechanical Parameters of Corvis ST II. Cornea ():10.1097/ICO.0000000000003191, December 13, 2022. | DOI: 10.1097/ICO.0000000000003191
- ↑ Huang G, Melki S. Small Incision Lenticule Extraction (SMILE): Myths and Realities. Semin Ophthalmol. 2021 May 19;36(4):140-148. doi: 10.1080/08820538.2021.1887897. Epub 2021 Apr 6. PMID: 33822679.
- ↑ Lv X, Zhang F, Song Y, Zhai C, Guo N, Lai L, Xu Y. Corneal biomechanical characteristics following small incision lenticule extraction for myopia and astigmatism with 3 different cap thicknesses. BMC Ophthalmol. 2023 Jan 30;23(1):42. doi: 10.1186/s12886-023-02786-8. PMID: 36717828; PMCID: PMC9885585.
- ↑ Yang, L., Liu, S., Zhou, X. et al. Correlation between the ablation ratio and posterior corneal stability after small incision lenticule extraction for high myopia. Graefes Arch Clin Exp Ophthalmol (2023). https://doi.org/10.1007/s00417-023-05979-5
- ↑ Vestergaard et al. : 'Efficacy, safety, predictability, contrast sensitivity and aberrations after femtosecond laser lenticule extraction' Journal of Cataract & Refractive Surgery, vol 40, no.3, pp. 403–411., 10.1016/j.jcrs.2013.07.053
- ↑ Wong, Chee Wai et al. : Incidence and management of suction loss in refractive lenticule extraction. Journal of Cataract & Refractive Surgery , Volume 40 , Issue 12 , 2002 – 2010
- ↑ Shah R, Shah S, Sengupta S: Results of small incision lenticule extraction: All-in-one femtosecond laser refractive surgery. J Cataract Refract Surg 2011, 37:127–137.
- ↑ Sekundo W, Kunert KS, Blum M: Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol 2011, 95:335–339.
- ↑ Vestergaard A, Ivarsen AR, Asp S, Hjortdal JO: Small-incision lenticule extraction for moderate to high myopia: predictability, safety, and patient satisfaction. J Cataract Refract Surg 2012, 38:2003–2010.
- ↑ Hjortdal JO, Vestergaard AH, Ivarsen A, Ragunathan S, Asp S: Predictors for the outcome of small-incision lenticule extraction for Myopia. J Refract Surg 2012, 28:865–871.
- ↑ Wang Y, Bao XL, Tang X, Zuo T, Geng WL, Jin Y: Clinical study of femtosecond laser corneal small incision lenticule extraction for correction of myopia and myopic astigmatism. Zhonghua Yan Ke Za Zhi 2013, 49:292–298.
- ↑ Kamiya K, Shimizu K, Igarashi A, Kobashi H: Visual and refractive outcomes of femtosecond lenticule extraction and small-incision lenticule extraction for myopia. Am J Ophthalmol 2014, 157:128–134. e122.
- ↑ Sekundo W, Gertnere J, Bertelmann T,Solomatin I: One-year refractive results, contrast sensitivity, high-order aberrations and complications after myopic small-incision lenticule extraction (ReLEx SMILE). Graefes Arch Clin Exp Ophthalmol 2014, 252(5):837-843.
- ↑ Agca A, Demirok A, Cankaya KI, Yasa D, Demircan A, Yildirim Y, Ozkaya A, Yilmaz OF: Comparison of visual acuity and higher-order aberrations after femtosecond lenticule extraction and small-incision lenticule extraction. Cont Lens Anterior Eye 2014, 37(4):292-296.
- ↑ Lin F, Xu Y, Yang Y: Comparison of the visual results after SMILE and femtosecond laser-assisted LASIK for myopia. J Refract Surg 2014, 30:248–254.
- ↑ Moshirfar M, Santos JM, Wang Q, Stoakes IM, Porter KB, Theis JS, Hoopes PC. A Literature Review of the Incidence, Management, and Prognosis of Corneal Epithelial-Related Complications After Laser-Assisted In Situ Keratomileusis (LASIK), Photorefractive Keratectomy (PRK), and Small Incision Lenticule Extraction (SMILE). Cureus. 2023 Aug 22;15(8):e43926. doi: 10.7759/cureus.43926. PMID: 37614825; PMCID: PMC10443604.
- ↑ Xu Y, Yang Y: Dry eye after small incision lenticule extraction and LASIK for myopia. J Refract Surg 2014, 30:186–190.
- ↑ Denoyer et al. : Dry Eye Disease after Refractive Surgery: Comparative Outcomes of Small Incision Lenticule Extraction versus LASIK, Ophthalmology, Available online 22 November 2014, ISSN 0161-6420, http://dx.doi.org/10.1016/j.ophtha.2014.10.004. (http://www.sciencedirect.com/science/article/pii/S016164201400952X)
- ↑ Ma, Kevin K. MD1; Manche, Edward E. MD1,*. Patient-Reported Quality of Vision in a Prospective Randomized Contralateral-Eye Trial Comparing LASIK and SMILE. Journal of Cataract & Refractive Surgery ():10.1097/j.jcrs.0000000000001127, December 20, 2022. | DOI: 10.1097/j.jcrs.0000000000001127
- ↑ Kirmaci Kabakci A, Kepez Yildiz B, Yildirim Y, Agca A, Ondes Yilmaz F, Demir G, Tulu Aygun B, Demirok A. Refractive and visual outcomes of small incision lenticule extraction (SMILE) in eyes with thin corneas. Eye (Lond). 2021 Aug;35(8):2302-2309. doi: 10.1038/s41433-020-01256-5. Epub 2020 Nov 2. PMID: 33139876; PMCID: PMC8302576.
- ↑ Zhou X, Shang J, Qin B, Zhao Y, Zhou X. Two-year observation of posterior corneal elevations after small incision lenticule extraction (SMILE) for myopia higher than -10 dioptres. Br J Ophthalmol. 2020 Jan;104(1):142-148. doi: 10.1136/bjophthalmol-2018-313498. Epub 2019 Apr 29. PMID: 31036587; PMCID: PMC6922016.
- ↑ Brar S, Roopashree CR, Ganesh S. Incidence of Ectasia After SMILE From a High-Volume Refractive Surgery Center in India. J Refract Surg. 2021 Dec;37(12):800-808. doi: 10.3928/1081597X-20210812-03. Epub 2021 Dec 1. PMID: 34914554.
- ↑ Zarei-Ghanavati S, Hassanzadeh S, Ambrósio R Jr. Corneal Ectasia after Laser-Assisted Small-Incision Lenticule Extraction: The Case for an Enhanced Ectasia Risk Assessment. J Curr Ophthalmol. 2022 Nov 30;34(3):357-363. doi: 10.4103/joco.joco_79_22. PMID: 36644473; PMCID: PMC9832456.
- ↑ Hernández-Chavarría C, Benedetti S M, García de Oteyza G, García-Albisua AM, Hernández-Quintela E. Bilateral Corneal Ectasia 3 Years After Small Incision Lenticule Extraction in a Borderline Case. Cornea. 2022 Mar 1;41(3):359-362. doi: 10.1097/ICO.0000000000002952. PMID: 34864796.
- ↑ Goupillou P, Boutillier G, Naguszewski D, Muraine M. Long-term follow-up of bilateral ectasia after laser-assisted Small-Incision Lenticule Extraction (SMILE) with known risk factors. Eur J Ophthalmol. 2022 Mar 2:11206721221085397. doi: 10.1177/11206721221085397. Epub ahead of print. PMID: 35234069.
- ↑ Huang TZ, Jin HY. Case Report: Bilateral Corneal Ectasia Developed during Pregnancy after Small-incision Lenticule Extraction. Optom Vis Sci. 2022 Jun 1;99(6):528-533. doi: 10.1097/OPX.0000000000001877. Epub 2022 Feb 11. PMID: 35149635; PMCID: PMC9169746.
- ↑ Wang Y, Ma J, Zhang L, Zou H, Li J, Zhang Y, Jhanji V. Postoperative Corneal Complications in Small Incision Lenticule Extraction: Long-Term Study. J Refract Surg. 2019 Mar 1;35(3):146-152. doi: 10.3928/1081597X-20190118-02. PMID: 30855091.
- ↑ Moshirfar M, Somani AN, Vaidyanathan U, Ronquillo YC, Hoopes PC. Pressure-Induced Interlamellar Stromal Keratitis After Small-Incision Lenticule Extraction Procedure: A Case Report. Cornea. 2020 Feb;39(2):254-257. doi: 10.1097/ICO.0000000000002196. PMID: 31688202.
- ↑ Mokumu D, Hu W, Damaola A, Wu J. Interface fluid syndrome after small incision lenticule extraction surgery secondary to posner schlossman syndrome - A case report. Heliyon. 2023 Nov 4;9(11):e21863. doi: 10.1016/j.heliyon.2023.e21863. PMID: 38027722; PMCID: PMC10663904.
- ↑ Thulasi P, Kim SW, Shetty R, Randleman JB. Recalcitrant Epithelial Ingrowth After SMILE Treated With a Hydrogel Ocular Sealant. J Refract Surg. 2015 Dec;31(12):847-50. doi: 10.3928/1081597X-20151111-09. PMID: 26653731.
- ↑ Kamiya K, Takahashi M, Shoji N, Naruse S. Two cases of epithelial ingrowth after small incision lenticule extraction. Am J Ophthalmol Case Rep. 2020 Jul 9;19:100819. doi: 10.1016/j.ajoc.2020.100819. PMID: 32715156; PMCID: PMC7374183.
- ↑ Srivatsa S, Sood S. Epithelial ingrowth following small incision lenticule extraction. Indian J Ophthalmol. 2020 Dec;68(12):3062-3064. doi: 10.4103/ijo.IJO_941_20. PMID: 33229707; PMCID: PMC7856964.