Lacrimal Sac Tumors
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Lacrimal sac tumors are rare, but their early recognition and management is imperative as the tumors can be locally invasive and potentially life threatening. Tumors can be benign or malignant, and 55% of lacrimal sac tumors are malignant. Mortality rates for malignant tumors vary with stage and type, but fatal outcomes are reported in up to a third of patients. Patients present in a number of ways, including with symptoms of secondary acquired nasolacrimal obstruction. [1] [2] [3] [4] [5]
Anatomy: Tears are produced by the lacrimal glands; paired almond shaped exocrine glands, which sit in the superolateral orbit within the lacrimal fossa, an area within the frontal bone. The tears lubricate the eye and are then collected into the superior and inferior puncta and then drain into the inferior and superior canaliculi. From the canaliculi, the tears pass through the valve of Rosenmuller into the lacrimal sac, where they then flow down the nasolacrimal duct, the Valve of Hasner, and finally into the nasal cavity via the inferior meatus.[6]
Epidemiology
Benign tumors tend to present in younger patients, while malignant tumors present more commonly in the fifth decade.[4]
Signs and Symptoms
Most patients with lacrimal sac tumors present with signs and symptoms of chronic nasolacrimal duct obstruction - unilateral epiphora and/or a palpable mass in the lacrimal sac area. Blood-stained tears, aka hemolacria, have also been reported. The diagnosis of lacrimal sac tumor is typically made incidentally; unusual tissue is noticed during a dacryocystorhinostomy and so a biopsy is done. Late stage tumors may present with signs of orbital invasion, such as proptosis and nonaxial globe displacement, lymphadenopathy, overlying skin ulceration, and rarely, distant metastasis. [4][7] [8]
Pathology
Lacrimal sac tumors can be divided into epithelial and non-epithelial tumors.
Epithelial tumors: Epithelial tumors account for 60-94% of tumors. The lacrimal sac, like the upper respiratory tract, is lined by a pseudostratified columnar epithelium with cilia and goblet cells.
- Benign epithelial tumors include papillomas, oncocytomas, adenomas and cylindromas. Papillomas are the most common and comprise 36% of epithelial tumors. They are believed to develop secondary to pre-existing inflammation through squamous metaplasia. It is important to note that though papillomas are designated as "benign," the inverted papilloma type is associated with aggressive growth and recurrence, requiring careful management.
- Malignant epithelial tumors or carcinomas generally arise de novo, but can also arise from an existing papilloma. Squamous cell carcinoma (which presents histopathologically as a well differentiated tumor with keratin pearls) is most frequently seen, followed by transitional cell carcinoma (a tumor with papillary growth pattern), oncocytic adenocarcinoma (a tumor with nuclear atypia arranged in a pseudoglandular pattern), mucoepidermoid carcinoma (a tumor with mucous secreting cells), and cystic adenoid carcinoma (tumor composed of cells arranged in a cribriform pattern).[9] [10]Inverted papilloma is a locally aggressive tumor with a propensity for recurrence and malignant transformation, typically transforming to squamous cell carcinoma. A risk factor for both inverted papilloma and squamous cell carcinoma is human papillomavirus, specifically strains HPV-6 and HPV-18.[11] [12]
Non Epithelial Tumors: As compared to epithelial tumors, non-epithelial tumors are rarer, representing about 25% of lacrimal sac tumors. Non-epithelial tumors can be further divided into lymphoproliferative, melanocytic, and mesenchymal tumors.
- Lymphoproliferative tumors account for approximately 2-8% of lacrimal sac tumors. These tumors may be primary tumors of the lacrimal sac, but more commonly arise secondary to systemic spread in a patient with leukemia or lymphoma.[13]
- Melanocytic tumors account for 4-5% of lacrimal sac tumors. Benign lesions are incredibly rare with only a single case of a benign lacrimal sac nevus, and a handful of cases of lacrimal sac benign melanosis reported in the literature. Malignant melanomas account for 0.7% of ocular melanomas. The tumors arise either from melanocytes in the epidermal lining of the lacrimal sac or secondary to seeding of conjunctival melanomas along the lacrimal drainage system. [4][14] [15]
- Mesenchymal tumors constitute 12-14% of lacrimal sac tumors. Benign mesenchymal tumors include fibrous histiocytoma, which is the most common, followed by fibroma, hemangioma, hemangiopericytoma, angiofibroma, lipoma, leiomyoma, and osteoma. Malignant mesenchymal tumors of the lacrimal sac include Kaposi sarcoma and rhabdomyosarcoma. [4][16] [17]
Diagnosis
Physical Exam
The workup for a patient with a lacrimal mass and epiphora includes a full history, a complete ophthalmic exam, lacrimal probe and irrigation, and examination of the nose. Given that a mass may not be appreciated during early stages, diagnosis may be difficult to differentiate from chronic dacryocystitis.[4] On examination, the swelling can extend below the medial canthal tendon, is typically firm in consistency, and is usually adherent to the underlying structures.
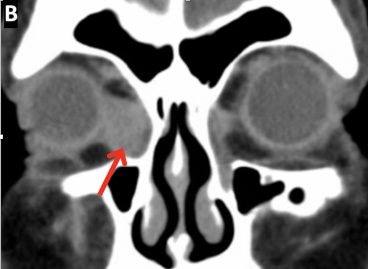
Imaging
Imaging can aid in diagnosis, determining extent of disease, and for surgical preparation. CT of the orbit and sinus is helpful for identifying changes to bone and invasion through bone while MRI provides increased visualization of the soft tissue. Examples of lacrimal sac tumors evident on CT and MRI imaging are included below. CT dacryocystography of the lacrimal system can be used to demonstrate a lacrimal sac filling defect, but does not delineate soft tissue well. Fine needle aspiration biopsy (FNAB) of lacrimal sac tumors is not recommended as interpretation of results are difficult and complications include hemorrhage, infection, and inadequate biopsy. Instead, a direct incisional biopsy is recommended for adequate tissue samples. A careful histopathologic assessment and diagnosis is needed to both confirm tumor type and guide treatment. Once detected, communication with oncology specialists is required to coordinate and assess the necessity of a metastatic workup. [4][7] [9]
Prognosis
The prognosis of lacrimal sac tumors depends on tumor type, malignancy, stage, grade, and the patient’s overall health. However, the overall mortality of malignant lacrimal sac tumors is approximately 38%, with transitional cell carcinoma and melanoma having the worst prognosis. [4]
Management
Benign epithelial or mesenchymal tumors confined to the lacrimal sac are often treated with a dacryocystectomy.
In cases of malignancy, an intact/en bloc tumor excision along with removal of the periosteum surrounding the lacrimal sac and the nasolacrimal duct is recommended, as cancer recurrence is believed to be due to the extension of premalignant lesions along the nasolacrimal duct. In cases with radiological evidence of tumors, which have spread beyond the lacrimal drainage system, resection of the orbital and nasal walls may be necessary. Postoperative radiation and or chemotherapy may be indicated in cases with bony and/or lymphatic invasion, as well as in cases without clear surgical margins, to both aid in tumor clearance and decrease recurrence risk. Recurrent tumors often require additional surgical intervention and, occasionally, palliative radiation therapy.[4][7][18]Patients should be managed by a multidisciplinary team with both short- and long-term monitoring, as recurrence and metastasis can occur years after initial management.[4]
References
- ↑ Ashton N, Choyce DP, Fison LG. Carcinoma of the lacrimal sac. Br J Ophthalmol.1951;35:366-376.
- ↑ Radnot M, Gall J. Tumors of the lacrimal sac. Ophthalmologica.1966;151: 2-22.
- ↑ Stefanyszyn MA, Hidayat AA, Pe’er JJ, et al. Lacrimal sac tumors. Ophthal Plast Reconstr Surg.1994;10:169-184.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Krishna Y, Coupland SE. Lacrimal Sac Tumors--A Review. Asia Pac J Ophthalmol (Phila). 2017;6(2):173–178. doi:10.22608/APO.201713
- ↑ Elner VM, Burnstine MA, Goodman ML, Dortzbach RK. Inverted Papillomas that Invade the Orbit. Arch Ophthalmol. 1995;113(9):1178-83.
- ↑ Newell FW. The lacrimal apparatus. In: Ophthalmology: Principles and Concepts, 6th, CV Mosby, St. Louis 1986. p.254.
- ↑ Jump up to: 7.0 7.1 7.2 Kim HJ, Shields CL, Langer PD. Lacrimal sac tumors: diagnosis and treatment. In: Black EH, Nesi FA, Cavana CJ, et al, eds. Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery. New York: Springer; 2012: 609-614.
- ↑ Schaefer DP. Acquired causes of lacrimal system obstructions. In: Black EH, Nesi FA, Cavana CJ, et al, eds. Smith and Nesi’s Ophthalmic Plastic and Reconstructive Surgery. New York: Springer; 2012:609-614.
- ↑ Jump up to: 9.0 9.1 Bi YW, Chen RJ, Li XP. Clinical and pathological analysis of primary lacrimal sac tumors. Zhonghua Yan Ke Za Zhi.2007;43:499-504.
- ↑ Flanagan JC, Stokes DP. Lacrimal sac tumors. Ophthalmology.1978;85: 1282-1287.
- ↑ Sjö NC, von Buchwald C, Cassonnet P, et al. Human papillomavirus: cause of epithelial lacrimal sac neoplasia? Acta Ophthalmol Scand.2007;85:551-556.
- ↑ Wang J, Ford J, Esmaeli B et al. Inverted papilloma of the orbit and nasolacrimal system. Ophthal Plast Reconstr Surg. In Press.
- ↑ Yip CC, Bartley GB, Habermann TM, et al. Involvement of the lacrimal drainage system by leukemia or lymphoma. Ophthal Plast Reconstr Surg.2002;18:242-246.
- ↑ Ren M, Zeng JH, Luo QL, et al. Primary malignant melanoma of lacrimal sac. Int J Ophthalmol.2014;7:1069-1070.
- ↑ Jakobiec FA, Stagner AM, Sutula FC, Freitag SK, Yoon MK. Pigmentation of the Lacrimal Sac Epithelium. Ophthalmic Plast Reconstr Surg. 2016;32(6):415–423. doi:10.1097/IOP.0000000000000541
- ↑ Pe’er JJ, Stefanyszyn M, Hidayat AA. Non epithelial tumors of the lacrimal sac. Am J Ophthalmol.1994;118:650-658.
- ↑ Anderson NG, Wojno TH, Grossniklaus HE. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthal Plast Reconstr Surg.2003;19:173-176.
- ↑ Stokes DP, Flanagan JC. Dacryocystectomy for tumors of the lacrimal sac. Ophthalmic Surg.1977;8:85-90.