Fuchs' Superficial Marginal Keratitis
All content on Eyewiki is protected by copyright law and the Terms of Service. This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
Disease Entity
Disease
Fuchs’ superficial marginal keratitis (FSMK) is a rare inflammatory disease of the peripheral cornea in which recurrent infiltration causes progressive peripheral corneal thinning.[1][2] It was initially described by Ferdinand Von Arlt in 1881, but is named eponymously for Ernst Fuchs who described the condition in greater detail in 1895.[2] It is most common in young[1][3][4][5][6] or middle-aged[2][5][7][8] adults, although cases in older patients have also been reported.[5][7][9]
Etiology
The underlying cause of FSMK is unknown. Evaluation for autoimmune or other inflammatory systemic disease is often unrevealing.[1][2][5][8] One case of FSMK in association with a perinuclear antineutrophil cytoplasmic antibody (p-ANCA)–positive vasculitis (demonstrated on skin biopsy) has been reported.[3]
Due to overlapping clinical features and reported rare co-occurrence, it has been suggested that Terrien’s marginal degeneration and FSMK may be different manifestations of the same pathological process.[3]
Pathology
Histopathology shows squamous hyperplasia without atypia, loss of Bowman layer, stromal thinning, mixed chronic inflammatory infiltrate, and vascular congestion.[2][7][8]
Diagnosis
History
Patients may provide a history of recurrent episodes of eye redness which are commonly accompanied by pain or discomfort.[1][4][5] Duration of episodes is generally on the order of days,[4][5] but can be longer.[7] Episodes may be self-limited.
Clinical Findings

FSMK characteristically presents with bilateral (often asymmetric) peripheral corneal stromal infiltration which causes thinning (Figure 1). [1][5][9] The area of thinning may be well-demarcated by a grey linear band.[5] Corneal thinning may be severe and cause a descemetocele[1] or spontaneous perforation, although this is not usually observed.[4][8] Pseudopterygia characteristically form over areas of peripheral thinning.[2][6][8][9] Peripheral hydropic cysts with Descemet membrane breaks may also form.[4] The absence of lipid deposition in the vicinity of thinning, which is characteristic of Terrien’s, distinguishes FSMK from Terrien’s marginal degeneration.[1]
Visual acuity may be normal when the central cornea is relatively uninvolved, but irregular corneal astigmatism which encroaches centrally may worsen visual acuity.[1][5][6][9]
Diagnostic Procedures
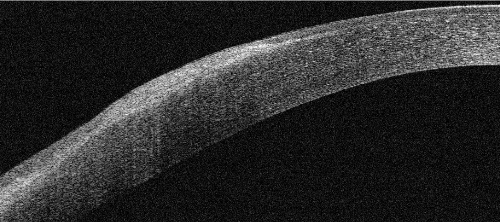
Multimodal imaging may be helpful to demonstrate characteristic findings. Corneal topography/tomography can demonstrate irregular corneal astigmatism and peripheral thinning.[1] Anterior segment optical coherence tomography (Figure 2) may be useful for assessing the extent of peripheral corneal thinning, especially when there is concern for evolving descemetocele.[1][9]
Laboratory testing
There is no specific laboratory test to diagnose FSMK. However, laboratory testing may be utilized to exclude alternate diagnoses (such as PUK) or to assess for possible underlying systemic inflammatory etiologies.[1][3][8]
Differential diagnosis
- Dellen
- Furrow degeneration (senile furrow degeneration)
- Infectious keratitis
- Marginal keratitis (staphylococcal marginal keratitis)
- Mooren's ulcer
- Ocular surface squamous neoplasia
- Peripheral ulcerative keratitis
- Pterygium
- Terrien's marginal degeneration
Management
Medical therapy
Owing to the rarity of FSMK, an optimal medical strategy is not known, and there is very limited data regarding the relative efficacy of various interventions. In fact, in most reported cases, disease progression occurs in spite of medical therapy. Topical steroids may be utilized to quell inflammation in acute episodes.[2][3][6][8] Topical lubricants[2][6] and antibiotics[2] are also commonly utilized acutely. Systemic use of doxycycline (to modulate matrix metalloproteinase activity) and Vitamin C (to promote collagen synthesis) might be beneficial in either acute episodes or chronic/maintenance therapy,[2][3] but data regarding such use are limited.
Medical follow-up
Patients should be followed longitudinally, as disease progression occurs over years.[3][5][6][9] Severe thinning and perforation may occur years after a patient’s initial presentation.[6]
Surgical management
Cyanoacrylate glue may be utilized for spontaneous micro-perforations.[1][8] Excision of pseudopterygia (as for excisional biopsy and/or ocular surface reconstruction) should not be routinely performed as iatrogenic perforation of severely thinned underlying stroma may occur.[6][9] For example, if a pseudopterygium of FSMK is mistaken for a true pterygium and underlying thinning is not recognized, then an iatrogenic perforation may be more likely. However, Kotecha et al report a case in which superficial keratectomy with conjunctival autograft was utilized bilaterally and appeared to reduce disease activity.[2] Amniotic membrane grafting may also be considered.[9] If ocular surface reconstruction is to be pursued, superficial keratectomy should be performed cautiously to minimize risk of perforation.
For cases of spontaneous descemetocele or imminent perforation, marginal reconstruction with tectonic lamellar corneoscleral patch graft may be used.[1][4][6][8][9] In diffuse severe thinning, 270 degree[1] and 360 degree grafts[9] have been utilized. FSMK may re-occur after grafting.[8]
References
- ↑ Jump up to: 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Mejía LF, Santamaría JP, Gaviria AM, Rodríguez AM. Fuchs' superficial marginal keratitis managed with circumferential marginal corneoscleral lamellar patch graft. Eur J Ophthalmol. 2013;23(6):925-927.
- ↑ Jump up to: 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Kotecha A, Raber IM. Superficial keratectomy and conjunctival autograft for Fuchs' superficial marginal keratitis. Cornea. 2001;20(2):214-216.
- ↑ Jump up to: 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Keenan JD, Mandel MR, Margolis TP. Peripheral ulcerative keratitis associated with vasculitis manifesting asymmetrically as Fuchs superficial marginal keratitis and Terrien marginal degeneration. Cornea. 2011;30(7):825-827.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 4.4 4.5 Goldberg MA, Lubniewski AJ, Williams JM, Smith ME, Pepose JS. Cystic hydrops and spontaneous perforation in Fuchs' superficial marginal keratitis. Am J Ophthalmol. 1996;121(1):91-93.
- ↑ Jump up to: 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Gifford SR. Marginal dystrophy of cornea: furrow keratitis. Am J Ophthalmol. 1925;8(1):16-23.
- ↑ Jump up to: 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Bierly JR, Dunn JP, Dawson CR, Ostler HB, Wong IG. Fuchs' superficial marginal keratitis. Am J Ophthalmol. 1992;113(5):541-545.
- ↑ Jump up to: 7.0 7.1 7.2 7.3 Ellis OH. Superficial marginal keratitis: clinical and anatomic findings in fellow eyes. Am J Ophthalmol. 1939;22(2):161-168.
- ↑ Jump up to: 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 8.9 Brilakis HS, Nordlund ML, Holland EJ. Recurrence of Fuchs marginal keratitis within a lamellar graft. Cornea. 2004;23(6):639-640.
- ↑ Jump up to: 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 9.8 9.9 Cheung AY, Sarnicola E, Kurji KH, Genereux BM, Holland EJ. Three hundred sixty-degree Fuchs superficial marginal keratitis managed with annular lamellar keratoplasty. Cornea. 2018;37(2):260-262.